Summary
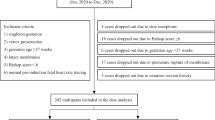
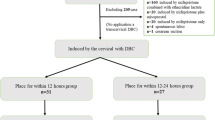
Labor induction is commonly used for achieving successful vaginal delivery. This study aimed to compare the effectiveness of dinoprostone and Cook’s balloon as labor-inducing agents in primipara women at term. A retrospective cohort study among primipara women was conducted in Hubei Maternity and Child Health Hospital. Basic clinical characteristics were collected. The main outcomes were vaginal delivery rate, cesarean section rate and forceps delivery rate. Obstetric and perinatal outcomes were also compared. Univariate and multivariate analyses were further performed to evaluate the predictors for vaginal delivery within 24 h. A total of 845 eligible primipara women undergoing labor induction were recruited. Of them, 141 women were induced with dinoprostone (dinoprostone group, DG), and 704 with Cook’s balloon (Cook’s balloon group, CG). Groups were homogeneous except more women with premature rupture of membranes in DG, with gestational hypertension in CG (P<0.05). The vaginal delivery rate within 12 h was 1.98% and 16.52% in CG and DG respectively (P=0.0001). Besides, the vaginal delivery rate within 24 h was 37.62% and 52.26% in CG and DG respectively (P=0.0079). DG showed the lower rate of oxytocin augmentation, artificial rupture of membrane and postpartum hemorrhage and the shorter interval from insertion to active labor than CG (P<0.05). Multivariate regression analysis revealed that abortion history, oxytocin augmentation, artificial rupture of membrane, and obstetric analgesia were independent predictors for vaginal delivery within 24 h. In conclusion, dinoprostone was more effective than Cook’s balloon to induce labor and achieve vaginal birth in the sample of primipara women at term.
Similar content being viewed by others
References
Lawani OL, Onyebuchi AK, Iyoke CA, et al. Obstetric outcome and significance of labour induction in a health resource poor setting. J Obstet Gynecol Int, 2014,2014(419621):1–5
Bulletins—Obstetrics ACOP ACOG Practice Bulletin No. 107: Induction of labor. Obstet Gynecol, 2009, 114(1):386–397
Laughon SK, Zhang J, Grewal J, et al. Induction of labor in a contemporary obstetric cohort. Am J Obstet Gynecol, 2012,206(6):486.e481–486.e489
Vogel JP, Souza JP, Gülmezoglu AM. Patterns and outcomes of induction of labour in Africa and Asia: a secondary analysis of the WHO Global Survey on Maternal and Neonatal Health. PloS One, 2013,8(6):e65612
Mozurkewich E, Chilimigras J, Koepke E, et al. Indications for induction of labour: a best-evidence review. BJOG, 2009,116(5):626–636
Vrouenraets FP, Roumen FJ, Dehing CJ, et al. Bishop score and risk of cesarean delivery after induction of labor in nulliparous women. Obstet Gynecol, 2005,105(4):690–697
Rosenstein MG, Cheng YW, Snowden JM, et al. The risk of stillbirth and infant death stratified by gestational age in women with gestational diabetes. Am J Obstet Gynecol, 2012,206(4):309.e301–309.e307
Lumbiganon P, Laopaiboon M, Gülmezoglu AM, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007–08. Lancet, 2010,375(9713):490–499
Duro-Gómez J, Garrido-Oyarzún MF, Rodríguez-Marín AB, et al. Efficacy and safety of misoprostol, dinoprostone and Cook’s balloon for labour induction in women with foetal growth restriction at term. Arch Gynecol Obstet, 2017,296(4):777–781
Diederen M, Gommers J, Wilkinson C, et al. Safety of the balloon catheter for cervical ripening in outpatient care: complications during the period from insertion to expulsion of a balloon catheter in the process of labour induction: a systematic review. BJOG, 2018,125(9):1086–1095
Wise MR, Marriott J, Battin M, et al. Outpatient balloon catheter vs inpatient prostaglandin for induction of labour (OBLIGE): a randomised controlled trial. Trials, 2020,21(1):1–11
Wilkinson C, Adelson P, Turnbull D. A comparison of inpatient with outpatient balloon catheter cervical ripening: a pilot randomized controlled trial. BMC Pregnancy Childbirth, 2015,15(1):126–133
Wilkinson C, Bryce R, Adelson P, et al. A randomised controlled trial of outpatient compared with inpatient cervical ripening with prostaglandin E 2 (OPRA study). BJOG, 2015,122(1):94–104
Jozwiak M, Bloemenkamp KW, Kelly AJ, et al. Mechanical methods for induction of labour. Cochrane Database Syst Rev, 2012,210(3):1–3
Jozwiak M, Rengerink KO, Ten Eikelder ML, et al. Foley catheter or prostaglandin E2 inserts for induction of labour at term: an open-label randomized controlled trial (PROBAAT-P trial) and systematic review of literature. Eur J Obstet Gynecol Reprod Biol, 2013,170(1):137–145
Thomas J, Fairclough A, Kavanagh J, et al. Vaginal prostaglandin (PGE2 and PGF2a) for induction of labour at term. Cochrane Database Syst Rev, 2014,1(6):No.: CD003101
Chen W, Zhou Y, Pu X, et al. Evaluation of Propess outcomes for cervical ripening and induction of labour in full-term pregnancy. J Obstet Gynaecol, 2014,34(3):255–258
Du C, Liu Y, Liu Y, et al. Double-balloon catheter vs. dinoprostone vaginal insert for induction of labor with an unfavorable cervix. Arch Gynecol Obstet, 2015,1(6):1221–1227
Ren H, Fan JH, Zhang L, et al. Clinical study of double-balloon catheter in full-term pregnancy to promote cevical maturity. Shanghai Jiaotong Univ, 2017,37(1):80–84
Løkkegaard E, Lundstrøm M, Kjær M, et al. Prospective multi-centre randomised trial comparing induction of labour with a double-balloon catheter versus dinoprostone. J Obstet Gynaecol, 2015,35(8):797–802
Suffecool K, Rosenn BM, Kam S, et al. Labor induction in nulliparous women with an unfavorable cervix: double balloon catheter versus dinoprostone. J Perinat Med, 2014,42(2):213–218
Sciscione AC, Ruhstaller K. Double-balloon catheter results in higher rate of vaginal delivery within 24 h when compared with dinoprostone vaginal insert. Evid Based Med, 2013,18(4):140–141
Grange J, Dimet J, Vital M, et al. Double-balloon catheter compared to vaginal dinoprostone for cervical ripening in obese women at term. Gynecol Obstet Fertil Senol, 2017,45(10):521–527
Edwards RK, Szychowski JM, Berger JL, et al. Foley catheter compared with the controlled-release dinoprostone insert: a randomized controlled trial. Obstet Gynecol, 2014,123(6):1280–1287
Cromi A, Ghezzi F, Uccella S, et al. A randomized trial of preinduction cervical ripening: dinoprostone vaginal insert versus double-balloon catheter. Am J Obstet Gynecol, 2012,207(2):125.e121–125.e127
Carlson NS, Corwin EJ, Hernandez TL, et al. Association between provider type and cesarean birth in healthy nulliparous laboring women: a retrospective cohort study. Birth, 2018,45(2):159–168
Pevzner L, Rayburn WF, Rumney P, et al. Factors predicting successful labor induction with dinoprostone and misoprostol vaginal inserts. Obstet Gynecol, 2009,114(2 Part 1):261–267
Scifres CM, Feghali M, Dumont T, et al. Large-for-gestational-age ultrasound diagnosis and risk for cesarean delivery in women with gestational diabetes mellitus. Obstet Gynecol, 2015,126(5):978–986
Nuthalapaty FS, Rouse DJ, Owen J. The association of maternal weight with cesarean risk, labor duration, and cervical dilation rate during labor induction. Obstet Gynecol, 2004,103(3):452–456
Beckmann M, Gibbons K, Flenady V, et al. Predictors of mode of birth and duration of labour following induction using prostaglandin vaginal gel. Aust N Z J Obstet Gynaecol, 2017,57(2):168–175
Ivars J, Garabedian C, Devos P, et al.. Simplified Bishop score including parity predicts successful induction of labor. Eur J Obstet Gynecol Reprod Biol, 2016,203:309–314
Obstetricians ACo, Gynecologists. ACOG practice bulletin no. 107: induction of labor. Obstet Gynecol, 2009,114(2):386–397
Zhao L, Lin Y, Jiang TT, et al. Vaginal delivery among women who underwent labor induction with vaginal dinoprostone (PGE2) insert: a retrospective study of 1656 women in China. J Matern Fetal Med, 2019,32(10):1721–1727
Son GH, Kim JH, Kwon JY, et al. Risk factors for cesarean delivery after induction of labor in nulliparous women with an unfavorable cervix at or beyond 41 weeks of gestation. Gynecol Obstet Inves, 2013,76(4):254–259
Liu YR, Pu CX, Wang XY, et al. Double-balloon catheter versus dinoprostone insert for labour induction: a meta-analysis. Arch Gynecol Obstet, 2019,299(1):7–12
Author information
Authors and Affiliations
Corresponding author
Additional information
This project was supported by Hubei Provine Health Commision Joint Foundation Project of China (No. WJ2019H281).
Conflict of Interest Statement
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Du, H., Zhang, N., Xiao, Cy. et al. Effectiveness of Dinoprostone and Cook’s Balloon for Labor Induction in Primipara Women at Term. CURR MED SCI 40, 951–959 (2020). https://doi.org/10.1007/s11596-020-2274-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-020-2274-1