Summary
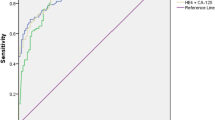
To determine whether ultrasound features can improve the diagnostic performance of tumor markers in distinguishing ovarian tumors, we enrolled 719 patients diagnosed as having ovarian tumors at Nanfang Hospital from September 2014 to November 2016. Age, menopausal status, histopathology, the International Federation of Gynecology and Obstetrics (FIGO) stages, tumor biomarker levels, and detailed ultrasound reports of patients were collected. The area under the curve (AUC), sensitivity, and specificity of the bellow-mentioned predictors were analyzed using the receiver operating characteristic curve. Of the 719 patients, 531 had benign lesions, 119 had epithelial ovarian cancers (EOC), 44 had borderline ovarian tumors (BOT), and 25 had non-EOC. AUCs and the sensitivity of cancer antigen 125 (CA125), human epididymis-specific protein 4 (HE4), Risk of Ovarian Malignancy Algorithm (ROMA), Risk of Malignancy Index (RMI1), HE4 model, and Rajavithi-Ovarian Cancer Predictive Score (R-OPS) in the overall population were 0.792, 0.854, 0.856, 0.872, 0.893, 0.852, and 70.2%, 56.9%, 69.1%, 60.6%, 77.1%, 71.3%, respectively. For distinguishing EOC from benign tumors, the AUCs and sensitivity of the above mentioned predictors were 0.888, 0.946, 0.947, 0.949, 0.967, 0.966, and 84.0%, 79.8%, 87.4%, 84.9%, 90.8%, 89.1%, respectively. Their specificity in predicting benign diseases was 72.9%, 94.4%, 87.6%, 95.9%, 86.3%, 90.8%, respectively. Therefore, we consider biomarkers in combination with ultrasound features may improve the diagnostic performance in distinguishing malignant from benign ovarian tumors.
Similar content being viewed by others
References
Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer, 2015,136(5):E359–386
Kaijser J, Van Belle V, Van Gorp T, et al. Prognostic value of serum HE4 levels and risk of ovarian malignancy algorithm scores at the time of ovarian cancer diagnosis. Int J Gynecol Cancer, 2014,24(7):1173–1180
Duffy MJ, Bonfrer JM, Kulpa J, et al. CA125 in ovarian cancer: European Group on Tumor Markers guidelines for clinical use. Int J Gynecol Cancer, 2005,15(5):679–691
Rosen DG, Wang L, Atkinson JN, et al. Potential markers that complement expression of CA125 in epithelial ovarian cancer. Gynecol Oncol, 2005,99(2):266–277
Paramasivam S, Tripcony L, Crandon A, et al. Prognostic importance of preoperative CA-125 in International Federation of Gynecology and Obstetrics stage I epithelial ovarian cancer: an Australian multicenter study. J Clin Oncol, 2005,23(25):5938–5942
Moore RG, Brown AK, Miller MC, et al. The use of multiple novel tumor biomarkers for the detection of ovarian carcinoma in patients with a pelvic mass. Gynecol Oncol, 2008,108(2):402–408
Wu L, Dai ZY, Qian YH, et al. Diagnostic value of serum human epididymis protein 4 (HE4) in ovarian carcinoma: a systematic review and meta-analysis. Int J Gynecol Cancer, 2012,22(7):1106–1112
Drapkin R, von Horsten HH, Lin Y, et al. Human epididymis protein 4 (HE4) is a secreted glycoprotein that is overexpressed by serous and endometrioid ovarian carcinomas. Cancer Res, 2005,65(6):2162–2169
Moore RG, McMeekin DS, Brown AK, et al. A novel multiple marker bioassay utilizing HE4 and CA125 for the prediction of ovarian cancer in patients with a pelvic mass. Gynecol Oncol, 2009,112(1):40–46
Li F, Tie R, Chang K, et al. Does risk for ovarian malignancy algorithm excel human epididymis protein 4 and CA125 in predicting epithelial ovarian cancer: a meta-analysis. BMC Cancer, 2012,12:258
Smorgick N, Maymon R. Assessment of adnexal masses using ultrasound: a practical review. Int J Womens Health, 2014,6:857–863
Jacobs I, Oram D, Fairbanks J, et al. A risk of malignancy index incorporating CA 125, ultrasound and menopausal status for the accurate preoperative diagnosis of ovarian cancer. Br J Obstet Gynaecol, 1990,97(10):922–929
Karlsen MA, Sandhu N, Hogdall C, et al. Evaluation of HE4, CA125, risk of ovarian malignancy algorithm (ROMA) and risk of malignancy index (RMI) as diagnostic tools of epithelial ovarian cancer in patients with a pelvic mass. Gynecol Oncol, 2012,127(2):379–383
Moore RG, Jabre-Raughley M, Brown AK, et al. Comparison of a novel multiple marker assay vs the Risk of Malignancy Index for the prediction of epithelial ovarian cancer in patients with a pelvic mass. Am J Obstet Gynecol, 2010,203(3):228.e1–6
Wilailak S, Chan KK, Chen CA, et al. Distinguishing benign from malignant pelvic mass utilizing an algorithm with HE4, menopausal status, and ultrasound findings. J Gynecol Oncol, 2015,26(1):46–53
Yanaranop M, Tiyayon J, Siricharoenthai S, et al. Rajavithi-ovarian cancer predictive score (R-OPS): A new scoring system for predicting ovarian malignancy in women presenting with a pelvic mass. Gynecol Oncol, 2016,141(3):479–484
Prat J. FIGO’s staging classification for cancer of the ovary, fallopian tube, and peritoneum: abridged republication. J Gynecol Oncol, 2015,26(2):87–89
Fluss R, Faraggi D, Reiser B. Estimation of the Youden Index and its associated cutoff point. Biom J, 2005,47(4):458–472
Tian Y, Wang C, Cheng L, et al. Determination of reference intervals of serum levels of human epididymis protein 4 (HE4) in Chinese women. J Ovarian Res, 2015,8:72
Zhang P, Wang C, Cheng L, et al. Comparison of HE4, CA125, and ROMA Diagnostic Accuracy: A Prospective and Multicenter Study for Chinese Women With Epithelial Ovarian Cancer. Medicine (Baltimore), 2015,94(52):e2402
Molina R, Escudero JM, Auge JM, et al. HE4 a novel tumour marker for ovarian cancer: comparison with CA 125 and ROMA algorithm in patients with gynaecological diseases. Tumour Biol, 2011,32(6):1087–1095
Shah CA, Lowe KA, Paley P, et al. Influence of ovarian cancer risk status on the diagnostic performance of the serum biomarkers mesothelin, HE4, and CA125. Cancer Epidemiol Biomarkers Prev, 2009,18(5):1365–1372
Timmerman D, Ameye L, Fischerova D, et al. Simple ultrasound rules to distinguish between benign and malignant adnexal masses before surgery: prospective validation by IOTA group. BMJ, 2010,341:c6839
Sassone AM, Timor-Tritsch IE, Artner A, et al. Transvaginal sonographic characterization of ovarian disease: evaluation of a new scoring system to predict ovarian malignancy. Obstet Gynecol, 1991,78(1):70–76
Van Gorp T, Veldman J, Van Calster B, et al. Subjective assessment by ultrasound is superior to the risk of malignancy index (RMI) or the risk of ovarian malignancy algorithm (ROMA) in discriminating benign from malignant adnexal masses. Eur J Cancer, 2012,48(11):1649–1656
Stiekema A, Lok CA, Kenter GG, et al. A predictive model combining human epididymal protein 4 and radiologic features for the diagnosis of ovarian cancer. Gynecol Oncol, 2014,132(3):573–577
Moszynski R, Szubert S, Szpurek D, et al. Usefulness of the HE4 biomarker as a second-line test in the assessment of suspicious ovarian tumors. Arch Gynecol Obstet, 2013,288(6):1377–1383
Xu Y, Zhong R, He J, et al. Modification of cut-off values for HE4, CA125 and the ROMA algorithm for early-stage epithelial ovarian cancer detection: Results from 1021 cases in South China. Clin Biochem, 2016,49(1–2):32–40
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of Interest Statement
We declare that we have no conflict of interest.
This work was supported by grants from Guangdong Science and Technology Department of China (No. 2016A020215115), Science and Technology Bureau of Tianhe District, Guangzhou, Guangdong (No. 201604KW010), and Science and Technology Bureau of Huadu District, Guangzhou, Guangdong (No. HD15CXY006).
Rights and permissions
About this article
Cite this article
Chen, Yn., Ma, F., Zhang, Yd. et al. Ultrasound Features Improve Diagnostic Performance of Ovarian Cancer Predictors in Distinguishing Benign and Malignant Ovarian Tumors. CURR MED SCI 40, 184–191 (2020). https://doi.org/10.1007/s11596-020-2163-7
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-020-2163-7