Abstract
Cardiorespiratory fitness is one of the most important indicators of health and improves length of life. The attention and acceptance for endurance training in patients with several cancer diagnoses increased during the last decade. This review highlight’s the effect of endurance training in cancer patients by summarizing exemplary randomized clinical trials and systematic reviews both within the acute hospital treatment context, as in a rehabilitation setting. To date, most studies focus on endurance training in patient groups with moderate to good prognosis. The studies within these patient groups evaluate the endurance training in cancer patients using a moderate training intensity between 50 and 75 % of the VO2 peak with an exercise time varying from 20 min (five times per week) in hospital up to 45 min (two to three times per week) in an ambulatory setting. Recently, the American College of Sports Medicine indicated that cancer survivors should follow the Physical Activity Guidelines for Americans, which represents ≥150 min per week of moderate intensity, ≥75 min per week of vigorous intensity aerobic exercise, or an equivalent combination of moderate and vigorous intensity aerobic exercises. To date, fewer studies evaluate the effects of endurance training in a palliative setting to maintain physical function of the patient. Future studies should investigate the effect of endurance training by evaluating different types of intensity training (moderate vs. high intensity training), the use of high-tech devices to improve physical activity, and to evaluate the effect of endurance training in patients with a palliative intention.
Similar content being viewed by others
Majority of the patients with oncological diseases are suffering from deconditioning and fatigue during and after completion of cancer treatment [16, 21, 24, 26, 32, 37]. These circumstances may last, even if patients surpassed the completion of the oncological therapy. This often leads to a reduced physical performance and a decline of all daily activities of cancer patients. As a result, patients may be restricted in their social life, which may negatively influence the patient’s quality of life [22].
A growing amount of evidence documents the positive effect of aerobic endurance training, both during and shortly after the oncological treatment [32]. Endurance training is an essential component of physical training and has gathered an important role in the (early) rehabilitation of oncological patients during the last decade [2, 16, 21, 25, 32].
An increase of the aerobic capacity is not only associated with a decrease of the infamous fatigue syndrome, but also with a significant improvement in the overall quality of life during and after the oncological treatment therapy [32]. Yet, the effectiveness of the endurance training in patients with oncological disease is influenced by several factors, such as time point of implementation of the endurance training (during or after the oncological treatment), stage of cancerous disease, type and degree of seriousness of the oncological treatment, and lifestyle of the patient [22].
The intention of this narrative review is to summarize and highlight exemplary randomized clinical trials and systematic reviews (meta-analyses) of aerobic exercise training in oncological patients during and shortly after cancer treatment both within the stationary treatment context, as in an ambulatory rehabilitation setting. Furthermore, the effects of endurance training in a palliative setting are presented. Finally, recommendations for aerobic exercise training are discussed. The results of the study analysis regarding the effects of endurance training are summarized in Table 1.
Endurance training within the stationary treatment context
Endurance training after hematological stem cell transplantation
The effects of endurance training on aerobic capacity after hematological stem cell transplantation in hospital have been examined by Baumann et al. [3], Jarden et al. [19] and Wiskemann et al. [36]. The training group consisting of 64 participants (five times weekly, 10–20 min, 80 % of VO2 max.) stabilized the intensity of the performance workload and the patients’ activities of daily living, following a supervised endurance training (on stationary ergometer) during the stem cell transplantation treatment [3]. The results of this study were equal to those in the study of Jarden et al. [19]. These patients carried out a combined endurance training (five times weekly, 15–30 min, 50–75 % of the maximum heart rate) combined with a resistive strength program and stretch and relaxation exercises.
The study of Wiskemann et al. [36] showed an improvement of the walking distance after a combined endurance and muscle training program which started 1–4 weeks before the transplantation procedure and ended 6–8 weeks after discharge from hospital (endurance training is three to five times weekly for 20–40 min).
Lung cancer patients
Directly after thoracotomy, 58 large cellular lung carcinoma patients were treated by a combined mobilization and muscle training program in a hospital (maximum heart rate was calculated by the formula 220 − age). A home endurance training program was added to the physical exercise training program in the hospital (12 weeks, content and intensity of the program are not clearly described). The exercise group was compared to a non-exercise control group. At baseline, the 6-min walking test decreased in both groups (5 days after surgery). However, both groups returned to the performance level (before the surgical intervention) at the end of the exercise program. This study could not show a benefit of endurance training on aerobic capacity in lung cancer patients compared to non-exercising controls [1].
Lymphoma patients
Courneya et al. [10] presented an example of the effectiveness of aerobic exercise training in lymphoma patients during adjuvant chemotherapy treatment. The included patients carried out an aerobic endurance training program between the chemotherapy cycles (12-week training program, thrice weekly, bicycle ergometer, 60–75 % of VO2 max.). During the first 4 weeks of the exercise program, patients exercised 15–20 min on a bicycle ergometer. Then, the time limit increased 5 min per week until 40–45 min of endurance training was achieved. During weeks 7 and 9, interval training (estimated VO2 peak. level above 75 %) was added to the basic aerobic training. The chemotherapeutic treatment was not disturbed during the endurance training. Yet, 3 of the 60 patients in the endurance group developed musculoskeletal problems (back, hip, or knee) and therefore had to apply an easier workout schedule. After 12 weeks of training, the oxygen intake capacity increased significantly in the endurance group (n = 60), while patients in the control group (n = 62) showed a decrease of the aerobic capacity.
During adjuvant therapy in ambulatory hospital
Breast cancer
The effects of an endurance training on the aerobic capacity of early stage breast cancer patients [9] during adjuvant therapy (chemotherapy, radiotherapy, and hormone therapy) provided good results after a supervised ergometer training during 18 weeks in 78 patients (thrice weekly, 15–45 min, estimated VO2 max. level 70–80 %). Yet, Segal et al. [30] could not show any difference in aerobic capacity between a supervised running program (33 participants), a home running program (32 participants), and a control group (34 participants). The study endured 26 weeks and included physical exercise training (three to five times per week, 50–60 % of the VO2 max.).
Prostate cancer
The effects of an endurance training on the aerobic capacity in prostate cancer patients during ambulatory radiotherapy provided good results after a 24-week supervised ergometer program, including 40 participants (thrice weekly, 15–45 min, 50–75 % of the maximal oxygen uptake capacity) [31].
The study of Windsor et al. [35] reported the effect of a home-based physical training program (running, thrice weekly, 50–60 % of the maximum heart rate during 26 weeks). The modified shuttle run test improved in the endurance group (33 participants). The quality of life and level of well-being also improved as a result of the supervised endurance training [35].
Furthermore, two studies examined the effects of a combined strength and endurance training program, reporting either the feasibility of a home-based walking program (16 weeks, three to five times weekly [11] or a supervised endurance training (ride bicycle or walking/running, twice weekly, 15–20 min, at 65–80 % of the maximum heart rate) [14] in prostate cancer patients receiving hormone treatment. These physical exercise programs lead to an improvement in physical fitness, quality of life, and fatigue.
Shortly after medical treatment
Breast cancer patients
A supervised ergometer endurance training program (15 weeks, thrice weekly, up to 35 min, at 70–75 % of the maximal oxygen uptake capacity) after adjuvant therapy improved the aerobic capacity of 25 breast cancer patients [8], compared to a non-exercising control group. Daley et al. [12] examined the effect of a monitored running program (8 weeks, thrice weekly, 60–85 % of the maximum heart rate adapted to age) on walking distance. Walking distance increased significantly after completion of the running program in the exercise group compared to the placebo and control groups. The study of Rogers et al. [28] could not demonstrate any significant difference between 21 patients participating in a home-based running program (12 weeks, 150 min weekly at 85 % of the maximum heart rate) and 21 control patients assessed with the Naughton treadmill test.
Colorectal cancer
Courneya et al. [6] examined the impact of a self-monitored running program in 102 colorectal cancer patients after surgery. The researchers found an increase in the walking distance among both the running and the control groups, whereas there was no statistical difference between the walking performance of both groups (duration of the running program 15 weeks, three to five times weekly, minimum loading time 20–30 min, 60–75 % of the maximum heart rate).
Patients with anemia
Courneya et al. [7] also examined the effect of a supervised bicycle ergometer program (12 weeks, three to five times weekly, 20–45 min, >60 % of the maximal oxygen uptake capacity) in 55 non-myeloid anemic cancer patients after chemotherapy. Both the physical exercise and the control groups received darbepoetine alpha during chemotherapy treatment. A significant difference regarding the oxygen intake capacity could be retrieved between the training and the control groups. Although the improvement of the oxygen uptake capacity in the exercise group was larger, no statistical difference concerning fatigue or quality of life could be pointed out between both groups.
Patients after hematological stem cell transplantation
The improvement of the 6-min walking test in the combined endurance and strengthening program group, including 64 allogeneic and autologous patients after stem cell transplantation (12 weeks, twice weekly, minimum 20 min of walking or cycling in an ambulatory setting, up to 75 % of the maximum heart rate), was statistically significant compared to the 6-min walking test result of the control group [23].
Patients with various types of cancer
Dimeo et al. [13] reported a significant increase of the performance intensity in the endurance training group (bicycle ergometer during 3 weeks, five times weekly, up to 30 min, 50 rpm, at 80 % of the maximum heart rate) compared to the control group, which was instructed to perform the Jacobson muscle relaxation method. This study was postoperatively performed in the hospital in 51 patients with either lung, rectal, colonic, gastric, or sigmoid cancer.
Thorsen et al. [33] observed a 23 % increase of the maximum oxygen intake capacity in the endurance training group of 111 lymphoma, breast, testical, and gynecological cancer patients during chemotherapy treatment. The running and self-monitored home program endured 14 weeks (twice per week, minimum load duration 30 min, 60–70 % of the maximum heart rate, at a Borg scale of 13 “somewhat hard–steady pace” to 15 “hard”). The maximal oxygen uptake capacity of the control group improved also without physical exercise training (10 %).
The effect of a supervised endurance training program on the maximal oxygen uptake capacity of oncological patients was analyzed in a meta-analysis. Six studies were included, analyzing a total of 571 patients (endurance group, 344 patients; control group, 227 patients). The meta-analyses showed an improvement of the maximal oxygen uptake capacity in favor of the endurance training group. Another important conclusion of this review is that mainly oncological patients in the early cancer stages may benefit from the endurance training [20].
Effects of an endurance training on advanced cancer patients treated with a palliative intention
Headley et al. [18] investigated the effect of an armchair fitness device (fitness while seated, 12 weeks, thrice weekly) on fatigue in comparison to a non-active control group in 38 breast cancer patients (stage IV). The result of this study yielded positive results for fatigue symptomatology in the training group. The fatigue level in the exercise group increased significantly slower than the non-exercising patients in the control group. A specific endurance effect was not assessed in this study.
Methodological quality
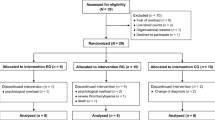
Earlier systematic reviews indicated that many of the RCTs undertaken to evaluate the effectiveness of exercise programs in cancer patients have been of only moderate methodological quality. However, since the introduction of criteria list for surveys of methodological concern regarding randomized studies, e.g., Delphi list [34], the quality of trials improved significantly from moderate to good in the second half of the last decade [22, 32]. However, some studies still fail to report a statement about important methodological quality criteria such as the blinding of examiner or exercise therapist, the concealment of group assignment, and the implementation of an intention-to-treat analysis. Reporting of these items may reduce the level of bias in randomized clinical trials. Furthermore, bias between randomized controlled studies in meta-analyses may also be caused by heterogeneity of the research designs of the studies, such as different therapeutic dosages or exercise strategies [27].
Recommendations for a disease-specific training
Oncological patients in ambulatory hospital settings should, if possible, perform an aerobic endurance training on a daily basis (15–30 min, at 50–75 % of the maximum heart rate). Patients in an ambulatory setting treated with (adjuvant) chemotherapy, radiotherapy, or hormonal therapy and patients in a rehabilitation setting following an exercise program directly after medical treatment should perform an endurance training program up to 45 min, at least two to three times weekly, in order to accomplish a safe and effective training. These patients should strive for a training intensity of 60–80 % of the maximum heart rate or for 50–75 % of the maximal oxygen uptake capacity. The endurance training should ideally be conducted using a bicycle ergometer or treadmill, because the physical performance level may be monitored continually.
Walking outdoors can also be a useful activity in order to improve endurance. It is recommended that the patient carries a heart rate monitor or pedometer to keep the physical effort during the walking training under surveillance.
Patients with no or little experience in physical exercise, patients who are suffering from severe side effects of the anti-cancer treatment or of an additional chronic disease should start with a daily training of lower intensity (10–15 min) or by means of a moderate interval training in order to achieve the desired overall duration [17]. According to current evidence, endurance training can be well-combined with resistive strength training. In order to prevent severe overload of the physical training, it is suggested to perform the endurance training on 2–3 days/week and to perform strength training on two other days [29].
The participation in endurance training is contraindicated in case of the following: acute hemorrhage, thrombocytopenia (below 10,000 units per μL blood), severe pain or infection, severe cardio-pulmonary complaints, and fever over 38 °C. Nausea and vomiting, days in which patients receive cardio- or nephrotoxic chemotherapy treatment, pallor, vomiting, headache, vertigo, and hyperventilation may challenge the participation of physical exercise training [4].
Supervised endurance training is a safe and efficient method in order to stabilize or improve the aerobic capacity in cancer patients with different diagnoses in early and advanced stages. Endurance training can be applied in order to stabilize the aerobic capacity in hospital or in the ambulatory phase during medical treatment. In the rehabilitation phase (starting immediately after completing anti-cancer treatment), aerobic capacity will increase after an endurance training of 12–18 weeks at a frequency of two to three times per week. Endurance training (combined with resistive strength training) can improve the quality of life and reduce fatigue symptomatology. The benefits of endurance training were particularly gained when applied in patients with an early cancer. Currently, there is only few evidence that reports the effect of endurance training in patients with advanced cancer stages. Thus, further studies should examine the appropriate training program for palliative patients in order to improve aerobic capacity.
However, despite the growing evidence of physical exercise training to improve aerobic capacity, the main principles of exercise training (i.e., specificity, overload, progression, initial values, reversibility, and diminishing returns) are not always included in the exercise protocols for cancer patients. By following the principles of exercise training and thoroughly reporting all components of the exercise prescription and adherence, specific evidence-based exercise prescriptions administered by healthcare professionals could be available for cancer patients and survivors in the near future [5]. Yet, even though the direct effects of aerobic exercise on cancer patients during and directly after medical treatment are not definitively proven, given that physical exercise is generally safe and improves aerobic capacity and quality of life especially in early cancer stages, and has numerous other health benefits, adequate physical exercise should be a standard part of cancer care [15].
References
Arbane G, Tropman D, Jackson D et al (2011) Evaluation of an early exercise intervention after thoracotomy for non-small cell lung cancer (NSCLC), effects on quality of life, muscle strength and exercise tolerance: randomised controlled trial. Lung Cancer 71:229–234
Baumann FT, Jäger E, Bloch W (2012) Sport und körperliche aktivität in der onkologie. Springer, Berlin, 121–130
Baumann FT, Kraut L, Schüle K et al (2010) A controlled randomized study examining the effects of exercise therapy on patients undergoing haematopoietic stem cell transplantation. Bone Marrow Transpl 45:355–362
Baumann FT, Schüle K (2008) Bewegungstherapie und sport bei krebs: leitfaden für die praxis. Deutscher Ärzte, Köln, pp S33–S55
Campbell KL, Neil SE, Winters-Stone KM (2012) Review of exercise studies in breast cancer survivors: attention to principles of exercise training. Br J Sports Med 46:909–916
Courneya KS, Friedenreich CM, Quinney HA et al (2003) A randomized trial of exercise and quality of life in colorectal cancer survivors. Eur J Cancer Care (Engl) 12:347–357
Courneya KS, Jones LW, Peddle CJ et al (2008) Effects of aerobic exercise training in anemic cancer patients receiving darbepoetin alfa: a randomized controlled trial. Oncologist 13:1012–1020
Courneya KS, Mackey JR, Bell GJ et al (2003) Randomized controlled trial of exercise training in postmenopausal breast cancer survivors: cardiopulmonary and quality of life outcomes. J Clin Oncol 21:1660–1668
Courneya KS, Segal RJ, Mackey JR et al (2007) Effects of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized controlled trial. J Clin Oncol 25:4396–4404
Courneya KS, Sellar CM, Stevinson C et al (2009) Randomized controlled trial of the effects of aerobic exercise on physical functioning and quality of life in lymphoma patients. J Clin Oncol 20:4605–4612
Culos-Reed SN, Robinson JW, Lau H, Stephenson L et al (2010) Physical activity for men receiving androgen deprivation therapy for prostate cancer: benefits from a 16-week intervention. Support Care Cancer 18:591–599
Daley AJ, Crank H, Saxton JM et al (2007) Randomized trial of exercise therapy in women treated for breast cancer. J Clin Oncol 25:1713–1721
Dimeo FC, Thomas F, Raabe-Menssen C et al (2004) Effect of aerobic exercise and relaxation training on fatigue and physical performance of cancer patients after surgery. A randomised controlled trial. Support Care Cancer 12:774–779
Galvao DA, Taaffee DR, Spry N et al (2010) Combined resistance and aerobic exercise program reverses muscle loss in men undergoing androgen suppression therapy for prostate cancer without bone metastases: a randomized controlled trial. J Clin Oncol 28:340–347
Giovannucci EL (2012) Physical activity as a standard cancer treatment. J Natl Cancer Inst 104(11):797–799
Granger CL, McDonald CF, Berney S et al (2011) Exercise intervention to improve exercise capacity and health related quality of life for patients with non-small cell lung cancer: a systematic review. Lung Cancer 72:139–153
Hayes SC, Spence R, Galvao D, Newton R (2009) Australian Association for Exercise and Sport Science position stand: optimising cancer outcomes through exercise. J Sci Med Sport 12(4):428–434
Headley JA, Ownby KK, John LD (2004) The effect of seated exercise on fatigue and quality of life in women with advanced breast cancer. Oncol Nurs Forum 31:977–983
Jarden M, Baadsgaard MT, Hovgaard DJ et al (2009) A randomized trial on the effect of a multimodal intervention on physical capacity, functional performance and quality of life in adult patients undergoing allogeneic SCT. Bone Marrow Transpl 43:725–737
Jones LW, Liang Y, Pituskin EN et al (2011) Effect of exercise training on peak oxygen consumption in patients with cancer: a meta-analysis. Oncologist 16:112–120
Keogh JW, Macleod RD (2012) Body composition, physical fitness, functional performance, quality of life, and fatigue benefits of exercise for prostate cancer patients: a systematic review. J Pain Symptom Manage 43(1):96–110
Knols R, Aaronson NK, Uebelhart D et al (2005) Physical exercise in cancer patients during and after medical treatment: a systematic review of randomized and controlled clinical trials. J Clin Oncol 23:3830–3842
Knols RH, de Bruin ED, Uebelhart D et al (2011) Effects of an outpatient physical exercise program on hematopoietic stem-cell transplantation recipients: a randomized clinical trial. Bone Marrow Transpl 46(9):1245–1255
Lowe SS, Watanabe SM, Baracos VE et al (2010) Physical activity interests and preferences in palliative cancer patients. Support Care Cancer 18:1469–1475
McNeely ML, Campbell KL, Rowe BH et al (2006) Effects of exercise on breast cancer patients and survivors: a systematic review and meta-analysis. CMAJ 175(1):34–41
McNeely ML, Courneya KS (2010) Exercise programs for cancer-related fatigue: evidence and clinical guidelines. J Natl Compr Canc Netw 8:945–953
Mittlböck M, Heinzl H (2006) A simulation study comparing properties of the heterogeneity measures in meta-analyses. Statistics in Medicine 25:4321–4333
Rogers LQ, Hopkins-Price P, Vicari S et al (2009) A randomized trial to increase physical activity in breast cancer survivors. Med Sci Sports Exerc 41:935–946
Schneider C, Dennehy C, Carter S (2003) Exercise and cancer recovery. Human Kinetics, Leeds, pp S11–S42
Segal R, Evans W, Johnson D et al (2001) Structured exercise improves physical functioning in women with stages I and II breast cancer: results of a randomized controlled trial. J Clin Oncol 19:657–665
Segal RJ, Reid RD, Courneya KS et al (2009) Randomized controlled trial of resistance or aerobic exercise in men receiving radiation therapy for prostate cancer. J Clin Oncol 27:344–351
Speck RM, Courneya KS, Mâsse LC et al (2010) An update of controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv 4:87–100
Thorsen L, Skovlund E, Strømme SB et al (2005) Effectiveness of physical activity on cardiorespiratory fitness and health-related quality of life in young and middle-aged cancer patients shortly after chemotherapy. J Clin Oncol 23:2378–2388
Verhagen AP, de Vet HC, de Bie RA et al (1998) The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol 51:1235–1241
Windsor PM, Nicol KF, Potter J (2004) A randomized, controlled trial of aerobic exercise for treatment-related fatigue in men receiving radical external beam radiotherapy for localized prostate carcinoma. Cancer 101:550–557
Wiskemann J, Dreger P, Schwerdtfeger R et al (2011) Effects of a partly self-administered exercise program before, during, and after allogeneic stem cell transplantation. Blood 117:2604–2613
Wiskemann J, Huber G (2008) Physical exercise as adjuvant therapy for patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transpl 41:321–329
Acknowledgments
We like to thank Sabine Hanke for her support in the translation of the review.
Conflict of interest
The author declares that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
This text was composed on the book chapter 'Ausdauertraining' in: Sport und körperliche Aktivität in der Onkologie Baumann, Jäger and Bloch (2012), Springer Verlag, Berlin:121-130.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Knols, R.H. Endurance training for cancer patients during and shortly after completion of the anti-cancer treatment. Eur Rev Aging Phys Act 10, 47–52 (2013). https://doi.org/10.1007/s11556-012-0117-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11556-012-0117-1