Abstract
Purpose
The elimination of abdominal tumors by percutaneous cryoablation has been shown to be an effective and less invasive alternative to open surgery. Cryoablation destroys malignant cells by freezing them with one or more cryoprobes inserted into the tumor through the skin. Alternating cycles of freezing and thawing produce an enveloping iceball that causes the tumor necrosis. Planning such a procedure is difficult and time-consuming, as it is necessary to plan the number and cryoprobe locations and predict the iceball shape which is also influenced by the presence of heating sources, e.g., major blood vessels and warm saline solution, injected to protect surrounding structures from the cold.
Methods
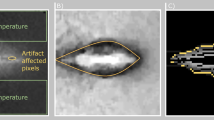
This paper describes a method for fast GPU-based iceball modeling based on the simulation of thermal propagation in the tissue. Our algorithm solves the heat equation within a cube around the cryoprobes tips and accounts for the presence of heating sources around the iceball.
Results
Experimental results of two studies have been obtained: an ex vivo warm gel setup and simulation on five retrospective patient cases of kidney tumors cryoablation with various levels of complexity of the vascular structure and warm saline solution around the tumor tissue. The experiments have been conducted in various conditions of cube size and algorithm implementations. Results show that it is possible to obtain an accurate result within seconds.
Conclusion
The promising results indicate that our method yields accurate iceball shape predictions in a short time and is suitable for surgical planning.







Similar content being viewed by others
References
Gonder MJ, Soanes WA, Smith V (1964) Experimental prostate cryosurgery. Investig Urol 1:610
Krunic AL, Marini LG (2015) Cryosurgery. In: Katsambas A, Lotti T, Dessinioti C, D’Erme AM (eds) European handbook of dermatological treatments. Springer, Berlin, pp 1139–1149
Gage AA, Baust J (1998) Mechanisms of tissue injury in cryosurgery. Cryobiology 37(3):171–186
Mazur P (1967) Physical-chemical factors underlying cell injury in cryosurgical freezing. Oak Ridge National Laboratory, TN. Technical report
Rezende KM, Moraes PdC, Oliveira LB, Thomaz LA, Junqueira JLC, Bönecker M (2014) Cryosurgery as an effective alternative for treatment of oral lesions in children. Braz Dent J 25(4):352–356
Magalov Z, Shitzer A, Degani D (2007) Isothermal volume contours generated in a freezing gel by embedded cryo-needles with applications to cryo-surgery. Cryobiology 55(2):127–137
Talbot H, Lekkal M, Béssard-Duparc R, Cotin S (2014) Interactive planning of cryotherapy using physically-based simulation. In: MMVR 21-medicine meets virtual reality-2014
Hossain SC, Zhang X, Haider Z, Hu P, Zhao G (2018) Optimization of prostatic cryosurgery with multi-cryoprobe based on refrigerant flow. J Therm Biol 76:58–67
Tsitskari M, Georgiades C (2015) Percutaneous cryoablation for renal cell carcinoma. J Kidney Cancer VHL 2(3):105–113
Young JL, McCormick DW, Kolla SB, Sountoulides PG, Kaufmann OG, Ortiz-Vanderdys CG, Huynh VB, Kaplan AG, Jain NS, Pick DL, Andrade LA, Osann KE, McDougall EM, Clayman RV (2012) Are multiple cryoprobes additive or synergistic in renal cryotherapy? Urology 79(2):484.e1–484.e6
Golkar E, Rao PP, Joskowicz L, Gangi A, Essert C (2018) Fast GPU computation of 3D isothermal volumes in the vicinity of major blood vessels for multiprobe cryoablation simulation. In: Proceedings of international conference on medical image computing and computer-assisted intervention (MICCAI). Springer, pp 230–237
Butz T, Warfield SK, Tuncali K, Silverman SG, van Sonnenberg E, Jolesz FA, Kikinis R (2000) Pre- and intra-operative planning and simulation of percutaneous tumor ablation. In: International conference on medical image computing and computer-assisted intervention. Springer, pp 317–326
Pennes HH (1948) Analysis of tissue and arterial blood temperatures in the resting human forearm. J Appl Physiol 1(2):93–122
Deng ZS, Liu J (2004) Numerical simulation of 3-D freezing and heating problems for combined cryosurgery and hyperthermia therapy. Numer Heat Transf Part A Appl 46(6):587–611
Deng ZS, Liu J (2006) Numerical study of the effects of large blood vessels on three-dimensional tissue temperature profiles during cryosurgery. Numer Heat Transf Part A Appl 49(1):47–67
Ge M, Chua K, Shu C, Yang W (2015) Analytical and numerical study of tissue cryofreezing via the immersed boundary method. Int J Heat Mass Transf 83:1–10
Ge M, Shu C, Chua K, Yang W (2016) Numerical analysis of a clinically-extracted vascular tissue during cryo-freezing using immersed boundary method. Int J Therm Sci 110:109–118
Ge M, Shu C, Yang W, Chua K (2017) Incorporating an immersed boundary method to study thermal effects of vascular systems during tissue cryo-freezing. J Therm Biol 64:92–99
Nabaei M, Karimi M (2018) Numerical investigation of the effect of vessel size and distance on the cryosurgery of an adjacent tumor. J Therm Biol 77:45–54
Zhang X, Hossain SC, Zhao G, Qiu B, He X (2017) Two-phase heat transfer model for multiprobe cryosurgery. Appl Therm Eng 113:47–57
Kumar A, Kumar S, Katiyar V, Telles S (2017) Phase change heat transfer during cryosurgery of lung cancer using hyperbolic heat conduction model. Comput Biol Med 84:20–29
Kumar M, Upadhyay S, Rai K (2018) A study of cryosurgery of lung cancer using modified Legendre wavelet Galerkin method. J Therm Biol 78:356–366
Keelan R, Zhang H, Shimada K, Rabin Y (2016) Graphics processing unit-based bioheat simulation to facilitate rapid decision making associated with cryosurgery training. Technol Cancer Res Treat 15(2):377–386
Villard C, Soler L, Papier N, Agnus V, Thery S, Gangi A, Mutter D, Marescaux J (2003) Virtual radiofrequency ablation of liver tumors. In: Ayache N, Delingette H (eds) Surgery simulation and soft tissue modeling. Springer, Berlin, pp 366–374
Villard C, Soler L, Gangi A (2005) Radiofrequency ablation of hepatic tumors: simulation, planning, and contribution of virtual reality and haptics. Comput Methods Biomech Biomed Eng 8(4):215–227
Huang HW (2013) Influence of blood vessel on the thermal lesion formation during radiofrequency ablation for liver tumors. Med Phys 40(7):073303
Dos Santos I, Haemmerich D, Schutt D, da Rocha AF, Menezes LR (2009) Probabilistic finite element analysis of radiofrequency liver ablation using the unscented transform. Phys Med Biol 54(3):627
Shao Y, Arjun B, Leo H, Chua K (2017) A computational theoretical model for radiofrequency ablation of tumor with complex vascularization. Comput Biol Med 89:282–292
Rieder C, Kroeger T, Schumann C, Hahn HK (2011) GPU-based real-time approximation of the ablation zone for radiofrequency ablation. IEEE Trans Vis Comput Graph 17(12):1812–1821
Mariappan P, Weir P, Flanagan R, Voglreiter P, Alhonnoro T, Pollari M, Moche M, Busse H, Futterer J, Portugaller HR, Blanco Sequeiros R, Kolesnik M (2017) GPU-based RFA simulation for minimally invasive cancer treatment of liver tumours. Int J Comput Assist Radiol Surg 12(1):59–68
Audigier C, Mansi T, Delingette H, Rapaka S, Mihalef V, Carnegie D, Boctor E, Choti M, Kamen A, Ayache N, Comaniciu D (2015) Efficient lattice boltzmann solver for patient-specific radiofrequency ablation of hepatic tumors. IEEE Trans Med Imaging 34(7):1576–1589
Patil HM, Maniyeri R (2019) Finite difference method based analysis of bio-heat transfer in human breast cyst. Therm Sci Eng Prog 10:42–47
Blomberg T (1996) Heat conduction in two and three dimensions: computer modelling of building physics applications. Ph.D. thesis, Department of Building Physics, Lund University, Sweden. Report TVBH1008, ISBN 91-88722-05-8
Shah TT, Arbel U, Foss S, Zachman A, Rodney S, Ahmed HU, Arya M (2016) Modeling cryotherapy ice ball dimensions and isotherms in a novel gel-based model to determine optimal cryo-needle configurations and settings for potential use in clinical practice. Urology 91:234–240
Choi J, Bischof JC (2010) Review of biomaterial thermal property measurements in the cryogenic regime and their use for prediction of equilibrium and non-equilibrium freezing applications in cryobiology. Cryobiology 60(1):52–70
Nolden M, Zelzer S, Seitel A, Wald D, Müller M, Franz AM, Maleike D, Fangerau M, Baumhauer M, Maier-Hein L, Maier-Hein KH, Meinzer HP, Wolf I (2013) The medical imaging interaction toolkit: challenges and advances. Int J Comput Assist Radiol Surg 8(4):607–620
Joskowicz L, Cohen D, Caplan N, Sosna J (2019) Inter-observer variability of manual contour delineation of structures in ct. Eur Radiol 29(3):1391–1399
Acknowledgements
This work was partially supported by a grant from the Maimonide France-Israel Research in Biomedical Robotics, funded jointly by the French Ministry of Higher Education, Research and Innovation, the French Ministry for the Economy and Finance, and Israel Ministry of Science, Technology and Space, 2016–18, and by Grant 53681 (METASEG) from the Israel Ministry of Science, Technology and Space, 2016–2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any conflict of interest. The authors have no personal financial or institutional interest in any of the materials, software, or devices described in this article.
Human and animal rights
No animals or humans were involved in this research. All images were anonymized before delivery to the researchers.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Golkar, E., Rao, P.P., Joskowicz, L. et al. GPU-based 3D iceball modeling for fast cryoablation simulation and planning. Int J CARS 14, 1577–1588 (2019). https://doi.org/10.1007/s11548-019-02051-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-019-02051-8