Abstract
Objectives
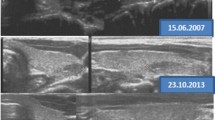
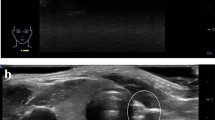
The prevalence of thyroid nodules in pediatric population is 0.2–2%, which is lower than adults. However, the probability of the nodule to be malignant is higher than adults (20–73%). Differential diagnosis of thyroid lesions in children includes intrathyroidal ectopic thymus tissue (ITT). ITT can present as a thyroid nodule, and be confused with malignancy with its hyperechoic pattern; this might cause unnecessary fine-needle aspiration biopsies and/or surgical interventions. In the current study, we mainly aim to define both US and color Doppler ultrasonography (CDUS) characteristics of ITT. We also aim to describe the most sensitive and most specific diagnostic parameters of ITT.
Methods
We have evaluated US examination reports of 56 children for whom differential diagnosis included ITT between February 2015 and August 2018. We have recorded sonographic characteristics of the lesions, CDUS data, and thyroid hormone levels.
Results
Study population consists of 56 patients (22 ITT, 34 other diagnoses). Median age of the population is 10 years. Age, sex, laboratory results, and follow-up change in lesion diameters do not show any significant difference between ITT and other diagnosis groups. Typical US appearance, fusiform lesion shape, and isovascular CDUS characteristics are higher in ITT group. The median value of the lesion’s highest diameter is smaller in ITT group. The most valuable criteria to predict ITT presence were the fusiform shape and the longest diameter of the lesion.
Conclusions
Fusiform shape and a maximum diameter of ≤ 9 mm are the most selective criteria to predict ITT diagnosis.


Similar content being viewed by others
References
Babcock DS (2006) Thyroid disease in the pediatric patient: emphasizing imaging with sonography. Pediatric radiology 36(4):299–308. https://doi.org/10.1007/s00247-005-0062-5 (quiz 372–293)
Hernandez-Cassis C, Poniecka A, Vogel CK, McKenzie JM (2008) A six-year-old boy with a suspicious thyroid nodule: intrathyroidal thymic tissue. Thyroid Off J Am Thyroid Assoc 18(3):377–380. https://doi.org/10.1089/thy.2007.0262
Kim HG, Kim MJ, Lee MJ (2012) Sonographic appearance of intrathyroid ectopic thymus in children. J Clin Ultrasound 40(5):266–271. https://doi.org/10.1002/jcu.21898
Spigland N, Bensoussan AL, Blanchard H, Russo P (1990) Aberrant cervical thymus in children: three case reports and review of the literature. J Pediatr Surg 25(11):1196–1199
Vlachopapadopoulou EA, Vakaki M, Karachaliou FE, Kaloumenou I, Kalogerakou K, Gali C, Michalacos S (2016) Ectopic intrathyroidal thymus in childhood: a sonographic finding leading to misdiagnosis. Horm Res Paediatr 86(5):325–329. https://doi.org/10.1159/000450724
Nasseri F, Eftekhari F (2010) Clinical and radiologic review of the normal and abnormal thymus: pearls and pitfalls. Radiogr Rev Publ Radiol Soc N Am Inc 30(2):413–428. https://doi.org/10.1148/rg.302095131
Avula S, Daneman A, Navarro OM, Moineddin R, Urbach S, Daneman D (2010) Incidental thyroid abnormalities identified on neck US for non-thyroid disorders. Pediatr Radiol 40(11):1774–1780. https://doi.org/10.1007/s00247-010-1684-9
Kim A, Kang SH, Bae YK (2014) Ectopic intrathyroidal thymus accompanied by intrathyroidal parathyroid as a cause of a solitary thyroid nodule in adult. Int J Clin Exp Pathol 7(9):6375–6378
Kabaalioglu A, Oztek MA, Kesimal U, Ceken K, Durmaz E, Apaydin A (2017) Intrathyroidal ectopic thymus in children: a sonographic survey. Med Ultrasonogr 19(2):179–184. https://doi.org/10.11152/mu-913
Han BK, Suh YL, Yoon HK (2001) Thymic ultrasound. I. Intrathymic anatomy in infants. Pediatr Radiol 31(7):474–479. https://doi.org/10.1007/s002470100467
Yildiz AE, Ceyhan K, Siklar Z, Bilir P, Yagmurlu EA, Berberoglu M, Fitoz S (2015) Intrathyroidal ectopic thymus in children: retrospective analysis of grayscale and doppler sonographic features. J Ultrasound Med Off J Am Inst Ultrasound Med 34(9):1651–1656. https://doi.org/10.7863/ultra.15.14.10041
Frates MC, Benson CB, Dorfman DM, Cibas ES, Huang SA (2018) Ectopic intrathyroidal thymic tissue mimicking thyroid nodules in children. J Ultrasound Med Off J Am Inst Ultrasound Med 37(3):783–791. https://doi.org/10.1002/jum.14360
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Institutional review board approval was obtained, and the need for informed consent was waived for the current retrospective study.
Rights and permissions
About this article
Cite this article
Aydin, S., Fatihoglu, E. & Kacar, M. Intrathyroidal ectopic thymus tissue: a diagnostic challenge. Radiol med 124, 505–509 (2019). https://doi.org/10.1007/s11547-019-00987-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-019-00987-0