Abstract
Purpose
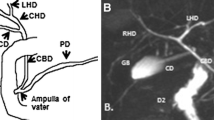
We assessed the usefulness of contrast-enhanced magnetic resonance cholangiography (CE-MRC) with liver-specific contrast agent in evaluating the biliary tree after hepatic surgery.
Materials and methods
A total of 142 patients with suspected biliary complications after liver surgery underwent hepatobiliary MR before and after administration of gadolinium ethoxy benzylic diethylenetriamine pentaacetic acid (Gd-EOB-DTPA). Unenhanced MR cholangiopancreatography (MRCP) and postcontrast MRC were obtained in all patients. Blinded image evaluation and semiquantitative analysis comparing MRCP and CE-MRC were performed by two experienced radiologists.
Results
In all cases, optimal postcontrast visualisation of the biliary tract was obtained. In 22 patients, a postsurgical biliary complication was confirmed. MRCP detected 64% of lesions, but in 36% of cases, an alteration was only suspected but not clearly defined. CE-MRC allowed definite diagnosis in 100% of cases.
Conclusions
Hepatobiliary-specific contrast agents allow for accurate and extensive study of biliary tract alterations, especially in assessing postsurgical complications.
Riassunto
Obiettivo
Scopo del nostro lavoro è valutare l’utilità della colangio-risonanza magnetica (RM) con mezzo di contrasto epatospecifico (CE-MRC) nello studio delle complicanze post-chirurgia epatica.
Materiali e metodi
Sono stati valutati 142 pazienti sottoposti ad intervento di chirurgia epatica con sospette complicanze biliari con colangio-pancreato-RM (MRCP) e sequenze post-contrasto con somministrazione di gadolinio-acido etossi-benzil-dietilen-triamino-pentaacetico (Gd-EOB-DTPA). Due radiologi con decennale esperienza specifica hanno valutato in cieco le immagini ottenute dalla MRCP e quelle della CE-MRC con analisi semiquantitativa dei reperti.
Risultati
In tutti i casi si è ottenuta adeguata visualizzazione biliare dopo somministrazione di mezzo di contrasto (MdC). ventidue dei 142 casi esaminati hanno mostrato complicanze biliari post-chirurgiche. La MRCP ha rilevato il 64% delle lesioni, ma nel 36% dei casi ha permesso solo di sospettare un’alterazione, senza consentire una definizione dirimente. La CE-MRC ha consentito una diagnosi certa nel 100% dei casi.
Conclusioni
L’uso di MdC ad escrezione epatobiliare consente uno studio accurato e panoramico delle alterazioni delle vie biliari, specie nelle complicanze postchirurgiche.
Similar content being viewed by others
References/Bibliografia
Rodríguez FJG, Montalvo MB, Freire RC et al (2008) Management of patients with iatrogenic bile duct injury. Cir Esp 84:20–27
Lau WY, Lai ECH (2007) Classification of iatrogenic bile duct injury. Hepatobiliary Pancreat Dis Int 6:459–463
Ragozzino A, De Ritis R, Mosca A et al (2004) Value of MR cholangiography in patients with iatrogenic bile duct injury after cholecystectomy. AJR Am J Roentgenol 183:1567–1572
Yamashita Y, Takada T, Kawarada Y et al (2007) Surgical treatment of patients with acute cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg 14:91–97
Flum DR, Cheadle A, Prela C et al (2003) Bile duct injury during cholecystectomy and survival in medicare beneficiaries. JAMA 290:2168–2173
Özogğul YB, Özer İ, Orugğ T et al (2009) Spontaneous hepaticoduodenal fistula functioning like a bilioenteric anastomosis following bile duct injury: case report. The Turkish Journal of Gastroenterology 20:220–222
McMahon AJ, Russell IT, Baxter JN et al (1994) Laparoscopic versus minilaparotomy cholecystectomy: a randomised trial. Lancet 343:135–138
Shea JA, Healey MJ, Berlin JA et al (1996) Mortality and complications associated with laparoscopic cholecystectomy. A meta-analysis. Ann Surg 224:609–620
Hung HH, Chen TS, Tseng HS et al (2009) Percutaneous transhepatic cholangiography and drainage is an effective rescue therapy for biliary complications in liver transplant recipients who fail endoscopic retrograde cholangiopancreatography. J Chin Med Assoc 72:395–401
Yazumi S, Chiba T (2005) Biliary complications after a right-lobe living donor liver transplantation. J Gastroenterol 40:861–865
Pascher A, Neuhaus P (2005) Bile duct complications after liver transplantation. Transplant International 18:627–642
Alfieri S, Di Miceli D, Pericoli Ridolfini M et al (2006) Occlusione del dotto pancreatico dopo duodenocefalopancreasectomia. Tecnica, diabete post-operatorio e trattamento delle fistole pancreatiche. Osp Ital Chir 12:1–7
Alexakis N, Sutton R, Neoptolemos JP (2004) Surgical treatment of pancreatic fistula. Dig Surg 21:262–274
Brady AP, McGrath FP, Moote DJ, Malone DE (1992) Post-laparoscopic cholecystectomies bilomas: preliminary experience. Clin Radiol 46:333–336
Vitale GC, Stephens G, Wieman TJ, Larson GM (1993) Use of endoscopic retrograde cholangiopancreatography in the management of biliary complications after laparoscopic cholecystectomy. Surgery 114:806–814
Laurent V, Ayav A, Hoeffel C et al (2009) Imaging of the postoperative biliary tract. J Radiol 90:905–917
Hoeffel C, Azizi L, Lewin M et al (2006) Normal and pathologic features of the postoperative biliary tract at 3D MR cholangiopancreatography and MR imaging. Radiographics 26:1603–1620
De Filippo M, Calabrese M, Quinto S et al (2008) Congenital anomalies and variations of the bile and the pancreatic ducts: magnetic resonance cholangiopancreatography findings, epidemiology and clinical significante. Radiol Med 113:841–859
Filippone A, Ambrosini R, Fuschi M et al (2003) Impatto clinico della colangiopancreatografia a risonanza magnetica nei pazienti con patologia biliare. Radiol Med 105:27–35
Manfredi R, Mehrabi S, Motton M et al (2008) MR imaging and MR cholangiopancreatography of multifocal intraductal papillary mucinous neoplasm of the side branches: MR pattern and its evolution. Radiol Med 11:414–428
Hamm B, Staks T, Muhler A et al (1995) Phase I clinical evaluation of Gd-EOB-DTPA as a hepatobiliary MR contrast agent: safety, pharmacokinetics, and MR imaging. Radiology 195:785–792
Lee NK, Kim S, Lee FW et al (2009) Biliary MR imaging with Gd-EOBDTPA and its clinical applications. Radiographics 29:1707–1724
Rohrer M, Bauer H, Mintorovitch J et al (2005) Comparison of magnetic properties of MRI contrast media solutions al different magnetic field strengths. Invest Radiol 40:715–724
Van Erkel AR, Pijl, van de Berg-Huysmans AA et al (2002) Hepatic metastases in patients with colorectal cancer: relationship between size of metastases, standard of reference, and detection rates. Radiology 224:404–409
Narita M, Hatano E, Arizono S et al (2009) Expression of AOTP1B3 determines uptake of Gd-EOBDTPA in hepatocellular carcinoma. J Gastroenterol 44:793–798
Vander Borght S, Libbrecht L, Blokzijl H et al (2005) Diagnostic and pathogenetic implications of the expression of hepatic transporters in focal lesions occurring in normal liver. J Pathol 207:471–482
Zollner G, Wagner M, Fickert P et al (2005) Hepatobiliary transporter expression in human hepatocellular carcinoma. Liver Int 25:367–379
Pecchi A, De Santis M, Di Benedetto F et al (2010) Role of magnetic resonance cholangiography in biliary complications of orthotopic liver transplantation. Radiol Med 115:1065–1079
Palmucci S, Mauro LA, Coppolino M et al (2010) Evaluation of the biliary and pancreatic system with 2D SSFSE, breathhold 3D FRFSE and respiratorytriggered 3D FRFSE sequences. Radiol Med 115:467–482
Seale MK, Catalano OA, Saini S et al (2009) Hepatobiliary-specific MR contrast agents: role in imaging the liver and biliary tree. Radiographics 29:1725–1748
Bollow M, Taupitz M, Hamm B et al (1997) Gadolinium-ethoxybenzyl-DTPA as a hepatobiliary contrast agent for use in MR cholangiography: results of an in vivo phase-I clinical evaluation. Eur Radiol 7:126–132
Carlos RC, Hussain HK, Song JH, Francis IR (2002) Gadoliniumethoxybenzyl-diethylenetriamine pentaacetic acid as an intrabiliary contrast agent: preliminary assessment. AJR Am J Roentgenol 179:87–92
Vitellas KM, El-Dieb A, Vaswani KK, et al (2002) Using contrastenhanced MR cholangiography with IV mangafodipir trisodium (Teslascan) to evaluate bile duct leaks after cholecystectomy: a prospective study of 11 patients. AJR Am J Roentgenol 179:409–416
Kapoor V, Baron RL, Peterson MS (2004) Bile leaks after surgery. AJR Am J Roentgenol 182:451–458
Li JH, Liu HT (2005) Diagnosis and management of cystic duct leakage after laparoscopic cholecystectomy: report of 3 cases. Hepatobiliary Pancreat Dis Int 4:147–151
Kim JY, Kim KW, Ahn C et al (2008) Spectrum of biliary and nonbiliary complications after laparoscopic cholecystectomy: radiologic findings. AJR Am J Roentgenol 191:783–789
Lohan D, Walsh S, McLoughlin R et al (2005) Imaging of the complications of laparoscopic cholecystectomy. Eur Radiol 15:904–912
Sharma S, Gurakar A, Jabbour N (2008) Biliary strictures following liver transplantation: past, present and preventive strategies. Liver Transpl 14:759–769
Verdonk RC, Buis CI, Porte RJ et al (2006) Anastomotic biliary strictures after liver transplantation: causes and consequences. Liver Transpl 12:726–735
Thethy S, Thomson B, Pleass H et al (2004) Management of biliary tract complications after orthotopic liver transplantation. Clin Transplant 18:647–653
Greif F, Bronsther OL, Van Thiel DH et al (1994) The incidence, timing and management of biliary tract complications after orthotopic liver transplantation. Ann Surg Jan 219:40–45
Eurich D, Seehofer D, Veltzke-Schlieker W et al (2009) Successful endoscopic and surgical management of non-anastomotic biliary strictures after liver transplantation — case report. Ann Transplant 14:47–51
Sicklick JK, Camp MS, Lillemoe KD et al (2005) Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann Surg 241:786–792
Gueroult S, Pann Y, Duron F et al (2004) Completion pancreatectomy for postoperative peritonitis after pancreaticoduodenectomy. Early and late outcome. Arch Surg 139:16–19
Benzoni E, Lorenzin D, Baccarani U et al (2006) Resective surgery for liver tumor: a multivariate analysis of causes and risk factors linked to postoperative complications. Hepatobiliary Pancreat Dis Int 5:526–533
Tanaka S, Hirohashi K, Tanaka H et al (2002) Incidence and management of bile leakage after hepatic resection for malignant hepatic tumors. J Am Coll Surg 195:484–489
Papanikolaou N, Prassopoulos P, Eracleous E et al (2001) Contrastenhanced magnetic resonance cholangiography versus heavily T2-weighted magnetic resonance cholangiography. Invest Radiol 36:682–686
Asbach P, Warmuth C, Stemmer A et al (2008) High spatial resolution T1-weighted MR imaging of liver and biliary tract during uptake phase of a hepatocyte-specific contrast medium. Invest Radiol 43:809–815
Holzapfel K, Breitwieser C, Prinz C et al (2007) Contrast-enhanced magnetic resonance cholangiography using gadolinium-EOB-DTPA. Preliminary experience and clinical applications. Radiologe 47:536–544
Marin D, Bova V, Agnello F et al (2010) Gadoxetate disodium-enhanced magnetic resonance cholangiography for the noninvasive detection of an active bile duct leak after laparoscopic cholecystectomy. J Comput Assist Tomogr 34:213–216
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salvolini, L., Urbinati, C., Valeri, G. et al. Contrast-enhanced MR cholangiography (MRCP) with GD-EOB-DTPA in evaluating biliary complications after surgery. Radiol med 117, 354–368 (2012). https://doi.org/10.1007/s11547-011-0731-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-011-0731-4