Abstract
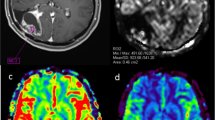
Magnetic resonance imaging (MRI) with a dynamic susceptibility contrast perfusion-weighted imaging (DSC-PWI) sequence to study brain tumours provides information on the haemodynamic characteristics of the neoplastic tissue. Brain perfusion maps and calculation of perfusion parameters, such as relative cerebral blood flow (rCBF), relative cerebral blood volume (rCBV) and mean transit time (MTT) allow assessment of vascularity and angiogenesis within tumours of the central nervous system (CNS), thus providing additional information to conventional MRI sequences. Although DSC-PWI has long been used, its clinical use in the study of brain tumours in daily clinical practice is still to be defined. The aim of this review was to analyse the application of perfusion MRI in the study of brain tumours by summarising our personal experience and the main results reported in the literature.
Riassunto
L’utilizzo della sequenza dinamica di perfusione con mezzo di contrasto (DSC-PWI) in risonanza magnetica (RM) nello studio dei tumori cerebrali fornisce informazioni sulle caratteristiche emodinamiche del tessuto neoplastico. L’elaborazione delle mappe di perfusione cerebrale ed il calcolo dei parametri di perfusione, come il flusso ematico cerebrale relativo (rCBF), il volume ematico cerebrale relativo (rCBV) ed il tempo di transito medio (MTT), consentono di studiare la vascolarizzazione ed i processi angiogenetici presenti nel contesto dei tumori del sistema nervoso centrale (CNS), fornendo informazioni aggiuntive alle sequenze RM convenzionali. Nonostante abbia un impiego diagnostico diffuso, l’esatto ruolo assunto dalla metodica nello studio delle neoplasie cerebrali, nella pratica clinica quotidiana, non è esattamente definito. Lo scopo di questa revisione è quello di analizzare le applicazioni della sequenza di perfusione nello studio dei tumori cerebrali riassumendo l’esperienza personale ed i principali risultati emergenti dalla letteratura.
Similar content being viewed by others
References/Bibliografia
Cha S (2004) Perfusion MR imaging of brain tumors. Top Magn Reson Imaging 15:279–289
Cha S, Knopp EA, Johnson G et al (2002) Intracranial mass lesions: dynamic contrast-enhanced susceptibility-weighted echo-planar perfusion MR imaging. Radiology 223:11–29
Schmainda KM, Rand SD, Joseph AM et al (2004) Characterization of a first-pass gradient-echo spin-echo method to predict brain tumor grade and angiogenesis. AJNR Am J Neuroradiol 25:1524–1532
Lupo JM, Cha S, Chang SM, Nelson SJ (2005) Dynamic susceptibility-weighted perfusion imaging of high-grade gliomas: characterization of spatial heterogeneity. AJNR Am J Neuroradiol 26:1446–1454
Knopp EA, Cha S, Johnson G et al (1999) Glial neoplasms: dynamic contrast-enhanced T2*-weighted MR imaging. Radiology 211:791–798
Law M, Yang S, Wang H et al (2003) Glioma grading: sensitivity, specificity, and predictive values of perfusion MR imaging and proton MR spectroscopic imaging compared with conventional MR imaging. AJNR Am J Neuroradiol 24:1989–1998
Aronen HJ, Gazit IE, Louis DN et al (1994) Cerebral blood volume maps of gliomas: comparison with tumor grade and histologic findings. Radiology 191:41–51
Henry RG, Vigneron DB, Fischbein NJ et al (2000) Comparison of relative cerebral blood volume and proton spectroscopy in patients with treated gliomas. AJNR Am J Neuroradiol 21:357–366
Sugahara T, Korogi Y, Kochi M et al (1998) Correlation of MR imaging-determined cerebral blood volume maps with histologic and angiographic determination of vascularity of gliomas. AJR Am J Roentgenol 171:1479–1486
Caseiras GB, Chheang S, Babb J et al (2010) Relative cerebral blood volume measurements of low-grade gliomas predict patient outcome in a multi-institution setting. Eur J Radiol 73:215–220
Danchaivijitr NWA, Tozer DJ (2008) Low-grade gliomas: do changes in rCBV measurements at longitudinal perfusion-weighted MR imaging predict malignant trasformation? Radiology 247:170–178
Law M, Oh S, Johnson G et al (2006) Perfusion magnetic resonance imaging predicts patient outcome as an adjunct to histopathology: a second reference standard in the surgical and nonsurgical treatment of low-grade gliomas. Neurosurgery 58:1099–1107
Law M, Young RJ, Babb JS et al (2008) Gliomas: predicting time to progression or survival with cerebral blood volume measurements at dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. Radiology 247:490–498
Bisdas S, Kirkpatrick M, Giglio P et al (2009) Cerebral blood volume measurements by perfusion-weighted MR imaging in gliomas: ready for prime time in predicting short-term outcome and recurrent disease? AJNR Am J Neuroradiol 30:681–688
Hirai T, Murakami R, Nakamura H et al (2008) Prognostic value of perfusion MR imaging of high-grade astrocytomas: long-term follow-up study. AJNR Am J Neuroradiol 29:1505–1510
Law M, Oh S, Babb JS et al (2006) Low-grade gliomas: dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging—prediction of patient clinical response. Radiology 238:658–667
Xu M, See SJ, Ng WH et al (2005) Comparison of magnetic resonance spectroscopy and perfusion-weighted imaging in presurgical grading of oligodendroglial tumors. Neurosurgery 56:919–926
Cha S, Tihan T, Crawford F et al (2005) Differentiation of low-grade oligodendrogliomas from low-grade astrocytomas by using quantitative blood-volume measurements derived from dynamic susceptibility contrast-enhanced MR imaging. AJNR Am J Neuroradiol 26:266–273
Lev MH, Ozsunar Y, Henson JW et al (2004) Glial tumor grading and outcome prediction using dynamic spin-echo MR susceptibility mapping compared with conventional contrast-enhanced MR: confounding effect of elevated rCBV of oligodendrogliomas [corrected]. AJNR Am J Neuroradiol 25:214–221
Maia AC Jr, Malheiros SM, da Rocha AJ et al (2005) MR cerebral blood volume maps correlated with vascular endothelial growth factor expression and tumor grade in nonenhancing gliomas. AJNR Am J Neuroradiol 26:777–783
Brasil Caseiras G, Ciccarelli O, Altmann DR (2009) Low-grade gliomas: six-month tumor growth predicts patient outcome better than admission tumor volume, relative cerebral blood volume, and apparent diffusion coefficient. Radiology 253:505–512
Sugahara T, Korogi Y, Shigematsu Y et al (1999) Perfusion-sensitive MRI of cerebral lymphomas: a preliminary report. J Comput Assist Tomogr 23:232–237
Cotton F, Ongolo-Zogo P, Louis-Tisserand G et al (2006) Diffusion and perfusion MR imaging in cerebral lymphomas. J Neuroradiol 33:220–228
Hakyemez B, Erdogan C, Bolca N et al (2006) Evaluation of different cerebral mass lesions by perfusion-weighted MR imaging. J Magn Reson Imaging 24:817–824
Lee IH, Kim ST, Kim HJ et al (2010) Analysis of perfusion weighted image of CNS lymphoma. Eur J Radiol 76:48–51
Dandois V, De Coene B, Laloux P et al (2010) Increased relative cerebral blood volume (rCBV) in brain lymphoma. J Neuroradiol 38:191–193
Zhang H, Rödiger LA, Shen T et al (2008) Perfusion MR imaging for differentiation of benign and malignant meningiomas. Neuroradiology 50:525–530
Kremer S, Grand S, Remy C et al (2004) Contribution of dynamic contrast MR imaging to the differentiation between dural metastasis and meningioma. Neuroradiology 46:642–648
Law M, Cha S, Knopp EA et al (2002) High-grade gliomas and solitary metastases: differentiation by using perfusion and proton spectroscopic MR imaging. Radiology 222:715–721
Bulakbasi N, Kocaoglu M, Farzaliyev A et al (2005) Assessment of diagnostic accuracy of perfusion MR imaging in primary and metastatic solitary malignant brain tumors. AJNR Am J Neuroradiol 26:2187–2199
Hakyemez B, Erdogan C, Gokalp G et al (2010) Solitary metastases and high-grade gliomas: radiological differentiation by morphometric analysis and perfusion-weighted MRI. Clin Radiol 65:15–20
Cha S, Lupo JM, Chen MH et al (2007) Differentiation of glioblastoma multiforme and single brain metastasis by peak height and percentage of signal intensity recovery derived from dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. AJNR Am J Neuroradiol 28:1078–1084
Sugahara T, Korogi Y, Tomiguchi S et al (2000) Posttherapeutic intraaxial brain tumor: the value of perfusion-sensitive contrast-enhanced MR imaging for differentiating tumor recurrence from nonneoplastic contrast-enhancing tissue. AJNR Am J Neuroradiol 21:901–909
Hu LS, Baxter LC, Smith KA et al (2009) Relative cerebral blood volume values to differentiate high-grade glioma recurrence from posttreatment radiation effect: direct correlation between image-guided tissue histopathology and localized dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging measurements. AJNR Am J Neuroradiol 30:552–558
Mitsuya K, Nakasu Y, Horiguchi S et al (2010) Perfusion weighted magnetic resonance imaging to distinguish the recurrence of metastatic brain tumors from radiation necrosis after stereotactic radiosurgery. J Neurooncol 99:81–88
Barajas RF, Chang JS, Sneed PK et al (2009) Distinguishing recurrent intra-axial metastatic tumor from radiation necrosis following gamma knife radiosurgery using dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. AJNR Am J Neuroradiol 30:367–372
Barajas RF, Jr., Chang JS, Segal MR et al (2009) Differentiation of recurrent glioblastoma multiforme from radiation necrosis after external beam radiation therapy with dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. Radiology 253:486–496
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Romano, A., Rossi Espagnet, M.C., Calabria, L.F. et al. Clinical applications of dynamic susceptibility contrast perfusion-weighted MR imaging in brain tumours. Radiol med 117, 445–460 (2012). https://doi.org/10.1007/s11547-011-0715-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-011-0715-4