Abstract
Purpose
The aim of this study was to evaluate the usefulness of imaging for correct clinical and therapeutic management of patients with scrotal disease.
Materials and methods
Between 2000 and 2007, 801 patients with suspected scrotal disease underwent colour Doppler ultrasonography (CDUS) at our centre. In 46 patients, the CDUS study was followed by magnetic resonance imaging (MRI).
Results
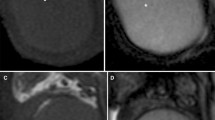
CDUS revealed an inflammatory process in 277 patients (34.58%), testicular trauma in 112 (13.9%), funicular torsion or torsion of the vestigial remnant in 44 (5.4%), findings suggestive of testicular neoplasm in 35 (4.3%) and no abnormality in 41.5%. MRI, used to further investigate the CDUS findings in 46 cases, showed three cases of intraparenchymal haematoma, one of intrascrotal cavernous body rupture, one of testicular abscess with intrascrotal fistula, two of testicular infarction and 15 of neoplasm. MRI allowed the exclusion of focal abnormalities in ten patients with testicular microlithiasis, in three with chronic orchitis and in four with atrophic involution. MRI confirmed the finding of inguinal hernia in three cases.
Conclusions
On the basis of our experience, CDUS is irreplaceable as an initial approach to patients affected by scrotal disease, whereas MRI is an ideal second-line investigation. MRI offers useful, and in some cases decisive, information, as it is capable of revealing unexpected findings and elucidating complex aspects. MRI helps improve patient management, with an overall reduction in costs.
Riassunto
Obiettivo
Scopo del lavoro è stato quello di valutare l’utilitá delle metodiche di immagine nei pazienti con patologia dello scroto per un corretto approccio clinico-terapeutico.
Materiali e metodi
Ottocentouno pazienti sono stati sottoposti ad indagine eco-color Doppler (ECD) e successivamente 46 pazienti sono stati indagati con risonanza magnetica (RM).
Risultati
L’ECD ha rilevato: in 277 pazienti (34,58%) processo flogistico, in 112 (13,9%) trauma del testicolo, in 44 (5,4%) torsione del funicolo o di un residuo embrionario, in 35 (4,3%) alterazioni riconducibili ad eteroplasia testicolare mentre nel 41,5% non erano presenti alterazioni patologiche. In 46 casi si è ricorsi alla RM per chiarimento o miglior definizione diagnostica del reperto ECD rilevando: 3 casi di ematoma intraparenchimale, 1 caso di rottura intrascrotale del corpo cavernoso, 1 caso di ascesso testicolare con fistola intrascrotale, 2 casi di infarto, 15 casi di eteroplasia. Inoltre ha permesso di escludere alterazioni focali in 10 pazienti affetti da microlitiasi testicolare (MT), in 3 con orchite cronica e in 4 con involuzione atrofica. In 3 casi ha confermato il reperto di ernia inguinale.
Conclusioni
Dalla nostra esperienza l’indagine ECD appare di insostituibile utilitá nel primo approccio ai pazienti con patologia scrotale e l’indagine RM rappresenta un ideale metodica di secondo livello. La RM è utile in casi selezionati, potendo rilevare situazioni complesse e precedentemente insospettabili, risultando in un miglioramento della gestione del paziente e in un contenimento globale dei costi.
Similar content being viewed by others
References/Bibliografia
Futterer JJ, Stijn H, Spermon J R (2008) Imaging the male reproductive tract: current trends and future directions. Radiol Clin N Am 46:133–147
Serra A, Hricak H, Coakley FV et al (1998) Inconclusive clinical and ultrasound evaluation of the scrotum: impact of magnetic resonance imaging on patient management and cost. Urology 51:1018–1021
Muglia V, Tucci S, Elias J et al (2002) Magnetic resonance imaging of scrotal diseases: when it makes the difference. Urology 59:419–423
Skoglund RW, Mc Roberts JW, Radge H (1970) Torsion of testicular appendage. Sonographic diagnosis. J Urol 104:598–600
Parenti GC, Montanari F, Baccarini P (1998) Utilità dell’ecografia nella diagnosi della torsione dell’Idatide del Morgagni: quattro casi. Radiol med 96:408–409
Kim W, Rosen MA, Langer EJ et al (2007) US-MR imaging correlation in pathologic conditions of the scrotum. RadioGraphics 267:1239–1253
Herbener TE (1996) Ultrasound in the assessment of the acute scrotum. J Clin Ultrasound 2424:405–421
Wittenberg AF, Tobias T, Rzeszotarski M, Minotti AJ (2006) Sonography of the acute scrotum: the four T’s of testicular imaging. Curr Probl Diagn Radiol 35:12–21
Bree RL, Hoang DT (1996) Scrotal ultrasound. Radiol Clin North Am 34:1183–1205
Parenti GC, Marri C, Calandra G et al (2000) La fascite necrotizzante dei tessuti molli: ruolo della diagnostica per immagini e revisione della letteratura. Radiol med 99:334–339
Boraschi P, Donati F, Auci A (2006) Patologia Splenica. In: Bartolozzi C, Lencioni R (eds) Risonanza magnetica dell’addome superiore. UTET, Milano, p 250
Fernandez-Perez GC, Tardaguila FM, Velasco M et al (2005) Radiologic findings of segmental testicular infarction. AJR Am J Roentgenol 184:1587–1593
Kodama K, Yotsuyanagi S, Fuse H et al (2000) Magnetic resonance imaging to diagnose segmental testicular infarction. J Urol 163:910–911
Parenti GC, Zago S, Lusa M et al (2007) Associazione tra microlitiasi e neoplasie testicolari maligne: nostra esperienza e revisione della letteratura. Radiol med 112:588–596
Thomas D, Vlachopapadopoulou E, Papadakis V et al (2008) Testicular microlithiasis in siblings: clinical implications. Pediatr Radiol 38:688–690
Dagash H, Mackinnon EA (2006) Testicular microlithiasis: what does it mean clinically? BJU Int 99:157–160
Lam DL, Gerscovich EO, Kuo MC, McGahan JP (2007) Testicular microlithiasis: our experience of 10 years. J Ultrasound Med 26:867–873
Coffey J, Huddart RA, Elliott F et al (2007) Testicular microlithiasis as a familial risk factor for testicular germ cell tumour. Br J Cancer 97:1701–1706
Major NM, Helms CA, Genant HK (1993) Calcification demonstrated as high signal intensity on T1-weighted MR images of the disks of the lumbar spine. Radiology 189:494–496
Bangert BA, Modic MT, Ross JS et al (1995) Hyperintense disks on T1-weighted MR images: correlation with calcification. Radiology 195:437–444
Kaplan PA (2004) Risonanza magnetica dell’apparato locomotore. Verduci Editore, Roma
Miller FN, Rosairo S, Clarke JL et al (2007) Testicular calcification and microlithiasis: association with primary intra-testicular malignancy in 3,477 patients. Eur Radiol 17:363–369
Heinemann V, Frey U, Linke J, Dieckmann KP (2003) Testicular microlithiasis—one case and four points to note. Scand J Urol Nephrol 37:515–518
Woodward PF, Sohaey R, O’Donogue MF, Green DE (2002) Tumors and tumorlike lesions of the testis: radiologic-patologic correlation. RadioGraphics 22:189–216
Dieckmann KP, Pichlmeier U (2004) Clinical epidemiology of testicular germ cell tumors. World J Urol 22:2–14
Pettersson A, Richiardi L, Nordenskjold A et al (2007) Age at surgery for undescended testis and risk of testicular cancer. N Engl J Med 356:1835–1841
Walsh TJ, Dall’Era MA, Croughan MS et al (2007) Prepubertal orchiopexy for cryptorchidism may be associated with lower risk of testicular cancer. J Urol 178:1440–1446
Guichard G, El Ammari J, Del Coro C et al (2008) Accuracy of ultrasonography in diagnosis of testicular rupture after blunt scrotal trauma. Urology 71:52–56
Buckley JC, McAninch JW (2006) Use of ultrasonography for the diagnosis of testicular injuries in blunt scrotal trauma. J Urol 175:175–178
Kim SH, Park S, Choi SH et al (2007) Significant predictors for determination of testicular rupture on sonography: a prospective study. J Ultrasound Med 26:1649–1655
Deurdulian C, Mittelstaedt CA, Chong WK, Fielding JR (2007) US of acute scrotal trauma: optimal technique, imaging findings, and management. RadioGraphics 27:357–369
Sarteschi LM, Morelli G, Menchini-Fabris GF (2003) Anatomia della borsa scrotale. In: Sarteschi LM, Morelli G, Menchini-Fabris GF (eds) Ecografia andrologica. Athena srl, Modena, pp 23–27
Pavlica P, Barozzi L, Branchini M (2006) Scroto. In: Rabbia C, Matricardi L (eds) Eco-Color-Doppler Vascolare. Minerva Medica, Torino, pp 1053–1063
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parenti, G., Feletti, F., Brandini, F. et al. Imaging of the scrotum: role of MRI. Radiol med 114, 414–424 (2009). https://doi.org/10.1007/s11547-009-0377-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-009-0377-7