Abstract
Purpose
The objective of this study was to explore the feasibility of combined morphological magnetic resonance imaging (MRI), [1H]magnetic resonance spectroscopic imaging (MRSI) and quantitative dynamic contrast-enhanced MRI (DCE-MRI) of human prostate cancer at 3 Tesla using a pelvic phased-array coil.
Materials and methods
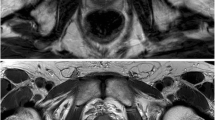
MRI, MRSI and DCE-MRI with a 3-Tesla whole-body scanner were performed in 30 patients with biopsy-proven prostate cancer before radical prostatectomy. High-resolution T2-weighted turbo spin echo (TSE) images were evaluated for visualisation of the peripheral zone, central gland, visibility of the cancer lesion, prostatic capsule delineation and overall image quality according to a five-point scale. Relative levels of the prostate metabolites citrate, choline and creatine were determined in cancer and in the normal peripheral zone (PZ) and central gland (CG). Spectra were also evaluated for the separation of the signal of citrate, choline and creatine and suppression of lipid and water signals. Time-intensity curves were obtained for prostatic cancer and healthy PZ and CG from DCE-MRI. Finally, time of arrival, time to peak, maximum enhancement and wash-in rate in cancer, normal PZ and CG were calculated.
Results
The high signal-to-noise ratio (SNR) at 3 Tesla provided T2-weighted TSE images with excellent anatomical detail (in-plane voxel size of 0.22×0.22 mm) and good T2 contrast. The increased spectral resolution was sufficient to separate the choline and creatine resonances and allow delineation of the four peaks of citrate resonance. The (choline + creatine)/citrate ratio was elevated in cancer in comparison with PZ and CG (p<0.001). Dynamic contrast-enhanced images showed good temporal resolution. All parameters obtained from DCE-MRI showed a statistically significant (P<0.05) difference between cancer tissue and normal PZ and CG. Wash-in rate and (choline+creatine)/citrate ratio were significantly correlated (r=0.713, P=0.001) in PZ cancer, whereas the correlation was not significant (r=0.617, P=0.06) in CG and in PZ (r=0.530, P=0.08).
Conclusions
It is possible to perform MRI of prostate cancer at 3 Tesla using a pelvic phased-array coil with high spatial, temporal and spectral resolution. The combination of vascular information from DCE-MRI and metabolic data from MRSI has excellent potential for improved accuracy in delineating and staging prostate carcinoma. These results suggest that high magnetic field strengths offer the possibility of studying prostate cancer without use of an endorectal coil.
Riassunto
Obiettivo
Esplorare la possibilità di effettuare uno studio combinato di risonanza magnetica del cancro prostatico di tipo morfologico (MRI), spettroscopico dell’idrogeno (MRSI) e dinamico postcontrastografico (DCE-MRI) a 3 Tesla utilizzando una bobina pelvica phased-array.
Materiali e metodi
Trenta pazienti con cancro prostatico dimostrato alla biopsia sono stati sottoposti a MRI, MRSI e DCE-MRI con apparecchiatura a 3 Tesla prima della prostatectomia radicale. Le immagini T2 pesate ad alta risoluzione sono state valutate in base ad una scala di 5 punti per la visualizzazione della zona periferica, della ghiandola centrale, della lesione tumorale, per la delineazione della capsula prostatica e per la qualità complessiva dell’immagine. Sono stati determinati i valori relativi dei metaboliti prostatici citrato, colina e creatina nel cancro, nella zona periferica normale (PZ) e nella ghiandola centrale (CG). Gli spettri sono stati anche valutati per la separazione del segnale del citrato, della colina e della creatina e la soppressione del segnale derivante dall’acqua e dai lipidi. Dai dati del DCE-MRI sono state generate curve intensità-tempo in corrispondenza del cancro, della PZ e della CG. Infine sono stati calcolati per il cancro, la PZ normale e la CG il time of arrival, time to peak, maximum enhancement e il wash in rate.
Risultati
L’elevato rapporto segnale-rumore (SNR) a 3 Tesla ha permesso di ottenere immagini TSE T2 pesate con un eccellente dettaglio anatomico (dimensioni in piano del voxel di 0,22×0,22 mm) e buon contrasto T2. L’incrementata risoluzione spettrale è risultata sufficiente a separare la risonanza della colina e della creatina e ha permesso di delineare i 4 picchi della risonanza del citrato. Il rapporto (colina+creatina)/citrato è risultato più elevato nel cancro rispetto a quello individuato nella PZ e nella CG (p<0,001). Le immagini dell’acquisizione dinamica post-contrastografica hanno mostrato una buona risoluzione temporale. Tutti i parametri ottenuti dal DCE-MRI hanno mostrato una differenza statisticamente significativa (p<0,05) tra tessuto neoplastico e PZ normale e CG. Il wash in rate e il rapporto (colina+creatina)/citrato sono risultati significativamente correlati (r=0,713, p=0,001) nel cancro nella zona periferica, mentre la correlazione non è risultata significativa nella CG (r=0,617, p=0,06) e nella PZ (r=0,530, p=0,08).
Conclusioni
È possibile effettuare uno studio di risonanza magnetica del cancro prostatico a 3 Tesla con elevata risoluzione spaziale, temporale e spettrale utilizzando una bobina pelvica phased-array. La combinazione delle informazioni derivanti dal DCE-MRI e dai dati spettroscopici ha eccellenti possibilità di incrementare l’accuratezza nella definizione e stadiazione del cancro prostatico. Questi risultati suggeriscono come campi i magnetici ad elevata intensità offrano la possibilità di studiare il cancro prostatico senza l’uso di una bobina endorettale.
Similar content being viewed by others
References/Bibliografia
Haacke EM (1999) Signal contrast and noise. In: Haacke EM (ed) Magnetic resonance imaging: physical principles and sequence design. John Wiley and Sons, New York, pp 378–379
Robitaille PM, Abduljalil AM, Kangarlu A (2000) Ultra high resolution imaging of the human head at 8Tesla: 2K × 2K for Y2K. J Comput Assist Tomogr 24:2–8
Tempany CM, Rahmouni AD, Epstein JI et al (1991) Invasion of the neurovascular bundle by prostate cancer: evaluation with MR imaging. Radiology 181:107–112
Huch Boni RA, Boner JA, Lutolf UM et al (1995) Contrast-enhanced endorectal coil MRI in local staging of prostate carcinoma. J Comput Assist Tomogr 19:232–237
Engelbrecht MR, Huisman HJ, Laheij RJ et al (2003) Discrimination of prostate cancer from normal peripheral zone and central gland tissue by using dynamic contrast-enhanced MR imaging. Radiology 229:248–254
Padhani AR, Gapinski CJ, Macvicar DA et al (2000) Dynamic contrast enhanced MRI of prostate cancer: correlation with morphology and tumour stage, histological grade and PSA. Clin Radiol 55:99–109
Scheidler J, Hricak H, Vigneron DB et al (1999) Prostate cancer: localization with three-dimensional proton MR spectroscopic imaging-clinicopathologic study. Radiology 213:473–480
Bottomley PA, Foster TH, Argersinger RE et al (1984) A review of normal tissue hydrogen NMR relaxation times and relaxation mechanisms from 1–100 MHz: dependence on tissue type, NMR frequency, temperature, species, excision, and age. Med Phys 11:425–448
Bernstein MA, Huston J 3rd, Lin C et al (2001) Highresolution intracranial and cervical MRA at 3.0T: technical considerations and initial experience. Magn Reson Med 46:955–962
Greenman RL, Shirosky JE, Mulkern RV et al (2003) Double inversion black-blood fast spin-echo imaging of the human heart: a comparison between 1.5T and 3.0T. J Magn Reson Imaging 17:648–655
Star-Lack J, Nelson SJ, Kurhanewicz J et al (1997) Improved water and lipid suppression for 3D PRESS CSI using RF band-selective inversion with gradient dephasing (BASING). Magn Reson Med 8:311–321
Hricak H, Dooms GC, McNeal JE et al (1987) MR imaging of prostate gland: normal anatomy. AJR Am J Roentgenol 148:51–55
Bloch BN, Rofsky NM, Baroni RH et al (2004) 3 Tesla magnetic resonance imaging of the prostate with combined pelvic phased-array and endorectal coils: initial experience. Acad Radiol 11:863–867
Fütterer, JJ, Scheenen TWJ, Huisman HJ et al (2004) Initial experience of 3 Tesla endorectal coil magnetic resonance imaging and 1H-spectroscopic imaging of the prostate. Invest Radiol 39:671–680
Cunningham CH, Vigneron DB, Marjanska M et al (2005) Sequence design for magnetic resonance spectroscopic imaging of prostate cancer at 3 T. Magn Reson Med 53:1033–1039
Jager GJ, Ruijter ET, van de Kaa CA et al (1997) Dynamic TurboFLASH subtraction technique for contrastenhanced MR imaging of the prostate: correlation with histopathologic results. Radiology 203:645–652
Preziosi P, Orlacchio A, Giambattista G et al (2003) Enhancement pattern of prostate cancer in dynamic MRI. Eur Radiol 13:925–930
Kiessling F, Lichy M, Grobholz R et al (2004) Simple models improve the discrimination of prostate cancers from the peripheral gland by T1-weighted dynamic MRI Eur Radiol 14:1793–1801
Barentsz JO, Engelbrecht M, Jager GJ et al (1999) A Fast dynamic gadoliniumenhanced MR imaging of urinary bladder and prostate cancer. J Magn Reson Imaging 10:295–304
Rouviere O, Raudrant A, Ecochard R et al (2003) Characterization of time-enhancement curves of benign and malignant prostate tissue at dynamic MR imaging. Eur Radiol 13:931–942
Heerschap A, Jager GJ, van der Graaf M et al (1997) In vivo proton MR spectroscopy reveals altered metabolite content in malignant prostate tissue. Anticancer Res 17:1455–1460
Kurhanewicz J, Vigneron DB, Hricak H et al (1996) Three-dimensional H-1 MR spectroscopic imaging of the in situ human prostate with high (0.24–0.7-cm3) spatial resolution. Radiology 198:795–805
Liney GP, Turnbull LW, Knowles AJ (1999) In vivo magnetic resonance spectroscopy and dynamic contrast enhanced imaging of the prostate gland. NMR Biomed 12:39–44
Mueller-Lisse UG, Vigneron DB, Hricak H et al (2001) Localized prostate cancer: effect of hormone deprivation therapy measured by using combined three-dimensional 1H MR spectroscopy and MR imaging: clinicopathologic case-controlled study. Radiology 221:380–390
Padhani AR, MacVicar AD, Gapinski CJ et al (2001) Effects of androgen deprivation on prostatic morphology and vascular permeability evaluated with MR imaging. Radiology 218:365–374
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carlani, M., Mancino, S., Bonanno, E. et al. Combined morphological, [1H]-MR spectroscopic and contrast-enhanced imaging of human prostate cancer with a 3-Tesla scanner: preliminary experience. Radiol med 113, 670–688 (2008). https://doi.org/10.1007/s11547-008-0271-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-008-0271-8
Keywords
- Prostate cancer
- Dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI)
- Magnetic resonance spectroscopic imaging (MRSI)
- High-field strength (3-T) MR imaging