Abstract
This study used a natural experiment of a new metro line in Hong Kong to examine trade-offs between transit-related and non-transit-related physical activity (PA) among 104 older people (aged ≥ 65 years) based on longitudinal accelerometer data that distinguished transit-related and non-transit-related PA. Difference-in-difference (DID) analysis compared PA changes between treatment and control groups. We found that new metro stations have trade-off effects between transit and non-transit PA. After opening metro stations, transit-related PA increased by 12 min per day on average, but non-transit-related PA decreased by 18 min per day. In addition, the proportion of time spent in transit-related PA increased by 6%. The results suggested that new metro stations could generate transit-related PA, but it might shift from non-transit-related PA among older people. Our findings revealed trade-off effects of public transit interventions and have significant implications for transport and healthy ageing studies.
Similar content being viewed by others
Introduction
Research has shown that public transit use can promote physical activity (PA). Cross-sectional studies found that transit users were more likely to walk 30 min or more per day than those non-users [1], and light rail transit (LRT) ridership is associated with greater moderate to vigorous exercise [2]. Longitudinally, bus rapid transit (BRT) implementation enhances physical activity by walking in catchment areas [3]. As public transit use involves walking or bicycling between transit stops and destinations, public transit users may be more likely to reach the recommended level of PA than non-public transit users. Although these studies provided findings on PA effects of public transit, such approaches have failed to address the impacts of other confounding factors, such as population density, destination mix, and street design.
Natural experiments can infer the causal effects of built environment interventions on PA and other health-related outcomes [4, 5]. A few natural experiment studies used new public transit lines as interventions to assess their health effects. By comparing the changes in outcomes of the treatment and control groups, we may infer causal evidence regarding PA and health effects [6]. For example, a UK study investigated the effects of the opening of the Cambridgeshire Guided Busway on travel behaviour, PA, and wider health impacts [7]. Similarly, US studies examined the before-and-after effects of LRT implementation on walking and PA [8, 9]. A natural experiment of a new metro line investigated the impact of new public transit on modal shift and active travel in China [10].
More recently, researchers have turned to the effect of public transit on specific types of PA, testing if changes in a particular domain of PA directly relate to public transport use and if there is a substation in PA types. For example, a meta-analysis found differences between changes in transit-related PA and overall PA after a new BRT or LRT. They found overall PA decreased, but transit-related PA increased after the new transit [11]. Another meta-analysis suggests that new public transit is associated with a significant increase in walking and other light to moderate PA by about 30 min per week, but no such effects for the moderate to vigorous PA [12]. Further, overall walking decreased over time, but the proportion of walking around new stations increased, suggesting a shift in walking activity to the station areas of the new public transit [13].
Estimating substitution in PA types will assist in a fuller health impact assessment of public transit interventions. For example, if transit users decrease other walking but increase the time spent in transit-related walking, attempts to increase transit use would not increase PA but only shift from one domain to another [14]. A US survey showed that some substitutions might occur for individuals with long commutes who might engage in less recreational PA than those with short commutes [15]. However, studies with self-reported PA could be biased due to measurement errors [11]. So far, few studies that provided a precise estimate of PA related to public transit use have been investigated using accelerometer-assessed data [14]. Longitudinal accelerometer data before and after a new public transit could examine PA substitutions by objective measures of type-specific PA.
Recent initiatives in healthy ageing in Asian cities heightened the need for new public transit infrastructure to support active travel and PA [16]. However, most existing evidence is based on working age adults from low-density western cities. Metro is the major public transit system in Asian cities, and most older people use public transport for mobility (e.g. Tokyo, Seoul, and Hong Kong) [17]. For example, in Hong Kong, over five million trips are made on an average weekday. The public transport shares (bus and metro) among older adults are over 93% [16, 18].
This study examined the trade-off effects of the new metro on older adults’ PA through a natural experiment study in Hong Kong. We hypothesised that new metro stations generate transit-related PA, but they might be shifted from non-transit-related PA. Difference-in-difference (DID) models compared changes in type-specific PA between treatment–control groups for robust inference. The ability to objectively measure PA using accelerometers, and within it, to distinguish transit-related from non-transit-related PA allowed us to examine the trade-off effect.
Method
Study Design
We examined the longitudinal accelerometer data from the Metro and Elderly Health in Hong Kong study, which is a natural experiment to investigate the effects of new metro stations on public transport use, PA, and wider health outcomes among older adults [19]. The study protocol was published elsewhere to describe the details of the study design [19]. In brief, the intervention was a new metro line with eight new stations in Hong Kong, of which half were newly built and the rest as modifications of the existing ones by adding new platforms, exits, and transfer connections. The treatment groups were from the affected areas with new metro stations, and control groups were from the areas the metro stations had been operated for more than 15 years. The new metro line went into operation in June 2021. The baseline survey was conducted in 2019, and a follow-up survey of the cohort of older people was conducted in December 2021.
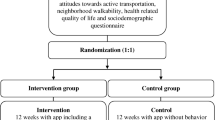
Our analysis for this paper was on the cohort data of 104 older adults. Figure 1 shows the treatment–control group assignment. Participants were recruited from older adults living within a 400-m pedestrian network buffer of two treatment groups and two control stations. They wore accelerometers for 7 days in both baseline and follow surveys to measure their PA before and after the new metro line.
Participants and Procedure
We recruited participants from neighbourhood elderly centres. The government-funded neighbourhood elderly centre in Hong Kong provides community support services for older people. Participants were aged 65 or above, living within four metro station areas in Hong Kong, and could walk unassisted for at least 15 min.
Trained interviewers administrated the face-to-face interview using questionnaires in the elderly neighbourhood centres. At the end of the interview, all participants were invited to participate in the study’s accelerometer component. The participants who agreed were instructed to wear a waist-worn accelerometer for 7 consecutive days during waking hours in both baseline and follow-up surveys before and after the new metro line. The participants were also asked to record the purpose, time, and destination of their trips involving public transit use in a travel diary over the study period. After completing the baseline survey, a modest incentive of HK$50 was provided to participants. To boost the retention rate for the longitudinal study, HK$100 was offered upon completing the follow-up accelerometer data.
Ethical approval for the study was obtained from the Human Research Ethics Committee of the University of Hong Kong (reference number: EA1710040), and written informed consent was provided by each participant.
Measures
Accelerometer-Assessed PA Outcomes
We used ActiGraph GT3X + accelerometers (Pensacola, FL, USA) to measure the participants’ PA for 7 consecutive days. All devices were initialized, and data were downloaded using ActiLife (v6.13.4). The accelerometer was programmed to record vertical acceleration in counts and PA data at a sampling frequency of 30 Hz [20].
Following the procedures specified in previous studies [21, 22], a wearing-time of ≥ 480 min/day was used as the criterion for a valid day, and ≥ 3 days per week was used as the criterion for a valid 7-day period of accumulated data. Participants who did not provide valid data were requested to re-wear the accelerometer for another 7 days. Intervals of at least 60 consecutive min with zero counts were defined as non-wear time and excluded from the analyses. We described older adults’ PA as a bout with a minimum duration of 5 min and a minimum of 25 counts per minute (cpm) [23]. Using a self-completed 7-day travel diary, PA is categorised into transit-related PA and non-transit-related PA.
-
Overall PA is PA regardless of its relationship with public transit (≥ 25 cpm, ≥ 5 min).
-
Transit-related PA is a PA within a trip involving public transport use. This threshold encompasses light to moderate PA (25–1013 cpm, ≥ 5 min) that corresponds with walking [8, 24]. Time was converted into transit-related PA if the travel diary reported walking involving public transit use.
-
Non-transit-related PA is PA that does not occur within a trip with public transit use. Time was converted into non-transit-related PA if the travel diary reported walking without public transit use (25–1013 cpm, ≥ 5 min), such as walking in the park. Non-transit-related PA also includes all moderate to vigorous PA minutes exceeding 1013 cpm [25].
-
The proportion of time spent on transit-related PA was applied as the outcome measure. Due to varying lengths of wear times among participants, we calculated the proportion (%) of the total amount of time spent on transit-related PA.
Covariates
Covariates included built environment characteristics and individual variables. We used a 400-m pedestrian network buffer from each participant’s residential address to create the built environment variables. The 400 m is a widely used criterion to define the neighbourhood area in Hong Kong due to the high-density built environment [26]. It delineates older people’s activity space by a 10-min walking distance from their residential places. A geographic information system (ArcGIS 10.7, Esri) was used to create the built environment variables. We calculated population density based on covered blocks of the network buffer. Street connectivity was measured as a link-node ratio within the buffer. The number of bus stops was measured, with a higher number indicating higher public transport accessibility. Destination mix was an entropy index based on fourteen categories of points of interest (e.g. commercial, industrial, recreational facilities, healthcare services, government and institutions, schools, restaurants), ranging from 0 (homogeneous destination) to 1 (equal mix of destinations) [27]. Individual variables were extracted from interviewer-administered questionnaires with questions regarding age, gender, monthly income (below HK$4,000 vs above), education level (primary vs secondary level and above), and chronic diseases (yes vs no).
Statistical Analysis
We used descriptive statistics and paired t-tests to compare changes in type-specific PA between baseline and follow-up data. For the main analyses, difference-in-difference (DID) analyses were performed to examine the treatment effects of metro interventions on the changes in different types of PA [28]. DID is a statistical approach that uses longitudinal data from treatment and control groups to obtain an appropriate counterfactual to estimate a causal effect [28]. It is a standard statistical tool for analysing natural experiment studies [29, 30]. We first included intervention-related variables for the physical activity in model 1, and we then added individual and built environment covariates in model 2 to reduce the error variance. The estimates held if the interaction term (e.g. treatment × time) remained statistically significant after adding covariates. The model specification was as follows:
where PAit is type-specific PA of participant i in time t; β1 captures the net difference between participants with or without exposure to new metro stations (treatment vs. control); β2 captures the net PA difference between participants at baseline and follow-up; and β3 is an interaction term estimating the treatment effects of the metro intervention. Covariatesi includes individual and built environment variables, and μi is the error term. If β3 is statistically significant, it means that new metro stations have significantly affected the type-specific PA of the participants.
In addition, we tested the effect of new metro stations on the proportion of time spent on transit-related PA using the same procedure as above.
Results
Descriptive Statistics
Table 1 shows the descriptive statistics of individual and built environment characteristics of the treatment and control groups with cohort data of 104 participants. The average age of the participants in the treatment and control groups was 73.38 and 76.28 years old, respectively. There was more female than male in both groups (75.40% and 74.40%). Less than 10% of the participants attained secondary-level education. Notably, most of the participants had chronic diseases, and the ratio in the treatment group was higher than that in the control group (86.20% vs 64.10%). In terms of the built environment characteristics, population density and destination mix were similar in both groups. The number of street intersections and link-node ratio in the treatment group were higher, while the number of bus stops was somewhat lower than those in the control group.
Table 2 shows the differences in average minutes per day of type-specific PA between baseline and follow-up. There was a non-significant increase in overall PA in both groups. In terms of transit-related PA, there was a significant increase of 14.98 min on average in the treatment group and a non-significant reduction of 0.60 min in the control group. For non-transit-related PA, there was an average reduction of 3.91 min in the treatment group, and an average increase of 14.42 min in the control group, but these changes were not significant. There was a significant increase of 4.22% in the proportion of time spent on transit-related PA in the treatment group after the opening of new metro stations.
DID Results of Intervention on Different Physical Activities
Overall PA
Table 3 shows the results of DID analysis. The estimated interaction terms in model 1 revealed no significant effects of the metro intervention on overall PA. After adjusting for individual and built environmental covariates, the coefficients remained insignificant (model 2). Regarding the covariates, link node ratio and the number of bus stops were positively related to overall PA, but destination mix was negatively associated with overall PA. Age was negatively associated with overall PA.
Transit-Related PA
The treatment effect on transit-related PA was significant when unadjusted for covariates in model 3. The coefficients remained significant after adjusting for individual and built environment covariates (model 4); this indicates that new metro stations increased transit-related PA by 12 min (p < 0.05) for the treatment group. Regarding the covariates, the link node ratio and the presence of chronic diseases were positively associated with transit-related PA.
Non-Transit-Related PA
The treatment effect on non-transit-related PA was significant when unadjusted for covariates (model 5). After adjusting for individual and built environment covariates, the coefficients remained significant, indicating new metro stations decreased non-transit-related PA by 18 min (p < 0.10) for the treatment group (model 6). Regarding the covariates, link node ratio and the number of bus stops were positively associated with non-transit-related PA, while destination mix was negatively associated with non-transit-related PA. Age was negatively associated with non-transit-related PA.
The Proportion of Time Spent on Transit-Related PA
Table 4 shows the treatment effect on the proportion (%) of time spent on transit-related PA. The interaction was significant when unadjusted for covariates (model 7). After adjusting for individual and environmental covariates, the coefficients remained significant; this indicates that new metro stations increased the proportion of time spent on transit-related PA by 6% (p < 0.10) (Mode 8). Population density was negatively associated with the proportion of transit-related PA, and link node ratio was positively associated with the proportion of transit-related PA. In addition, the presence of chronic diseases was positively associated with the proportion of transit-related PA.
Discussion
We provided the first natural experiment study on causal inference in trade-off effects of new metro stations on transit and non-transit PA among older adults. Using longitudinal accelerometer data, our DID results found that new metro stations did not affect overall PA, but they increased transit PA while reducing non-transit PA among older adults in Hong Kong.
We found transit-related PA increased after opening new metro stations, and there is a trade-off effect between transit and non-transit PA. Our results identified a 12-min per day increase in transit-related PA but an 18-min per day decrease in non-transit-related PA. In addition, we found an increase in transit-related PA by 6% for the treatment group after the opening of new metro stations. The new metro increased public transit use and physical activity among older adults in Hong Kong. The finding is consistent with previous studies that showed a significant increase in transit-related PA after new public transit [31]. Notably, they combined walking and cycling activities into one measure [6, 10]. Our study identified walking (25–1013 cpm, ≥ 5 min) as part of transit-related PA. Using accelerometer-assessed data, we provide precise information on whether the increase in PA is causally attributed to the use of new metro stations.
The finding in trade-offs between transit and non-transit PA corroborated the concept of ‘ActivityStat’ hypothesis [32, 33], which suggests that when PA is increased or decreased in one domain, there will be a compensatory change in another domain to maintain the levels of total PA or energy expenditure over time. Similarly, a US study examined individuals’ trade-offs between health-related activities and commuting time [15]. They found that such substitution happened to individuals with longer commutes, often characteristic of public transit use, engaged in less recreational PA than those with shorter commutes. Another cohort study also showed that a given level of transit-related PA would partially be compensated by reductions in non-transit PA (e.g. occupational or leisure) or spontaneous PA among older adults [34]. Furthermore, older adults are more likely to compensate PA than younger adults [35]. Older people’s energy expenditure or physical activity levels may be biologically regulated, thereby limiting the effectiveness of PA interventions. The trade-off effects on PA in different types should be considered when developing and evaluating interventions aimed at PA promotion among older people.
We found non-significant effects on overall PA among older people from new metro stations. The result differs from the findings of a previous review paper that highlighted that individual’s total physical activity would decrease after new public transit [8, 11, 13]. Our findings on trade-off effects on transit and non-transit PA did not lead to changes in overall PA in our study cohort. Our results based on accelerometer data also differ from the new metro’s treatment effects on self-reported moderate-to-vigorous physical activity (MVPA) [36]. The overall PA in this study included walking as light physical activity, while MVPA referred to PA exceeding the moderate metabolic level that does not involve walking. We surveyed four stations to collect fine-scale accelerator data from the 104 participants, while in He et al. (2022)’s study, they covered eight metro stations with 449 cohort data. This shows the self-reported and validated PA scale (e.g. IPAQ [37]) can survey a large and representative sample size, while it might easily have inconsistent findings with accelerometer-assessed PA data. Our results call for more endeavours to collect rigorous evidence on overall PA.
This study has limitations. First, participants’ specific PA types (e.g. transit-related or non-transit-related PA) in this study were generated from a self-reported travel diary. Future studies could be supplemented using additional objective reference data, such as a global positioning system (GPS). Unfortunately, in the high-density city of Hong Kong, GPS would easily lose signals making the measure impractical. Second, the intervention exposure duration was around 6 months. Due to delays in the new metro line, observing long-term treatment effects was impossible in this study within a 3-year funding period. Further research could explore the long-term effects of the intervention. Third, the COVID-19 pandemic could have affected PA changes [38]. Nevertheless, there were no local COVID-19 cases in Hong Kong during the follow-up survey period because of the zero COVID policy at the time (December 2021). We mitigated its potential effect by the treatment–control group research design.
The study also has several strengths. First, this longitudinal study using a natural experiment design provided causal estimates of new public transit’s effects on different types of PA among older adults. Previous cross-sectional studies cannot infer causality on how new public transport infrastructure would change PA among older people. Another strength is that we provide objective measures of PA changes using longitudinal accelerometer-assessed data. Most existing studies relied on self-reported questionnaires or travel survey data which might suffer recall biases. Moreover, this study characterised PA as either transit or non-transit PA by accelerometer data with travel diary to distinguish the trade-off effects on type-specific PA.
Conclusion
This study used longitudinal accelerometer data to examine the treatment effects of new metro stations on different types of PA among older adults. Our results suggest that new metro stations could generate transit-related PA, but it might shift from non-transit-related PA among older adults. A possible compensation of transit-related PA during non-transit-related PA time should be considered in studies analysing PA promotion through active transport or other activities. This study expands our knowledge of the PA benefits of new public transit interventions and has significant implications for transport and healthy ageing studies.
Data availability
The data that support the findings of this study are available on request from the corresponding author, Guibo Sun. The data are not publicly available due to ethical resons (e.g. their containing information that could compromise the privacy of research participants).
Change history
06 March 2023
A Correction to this paper has been published: https://doi.org/10.1007/s11524-023-00722-1
References
Freeland AL, Banerjee SN, Dannenberg AL, Wendel AM. Walking associated with public transit: moving toward increased physical activity in the United States. Am J Public Health. 2013;103(3):536–42. https://doi.org/10.2105/AJPH.2012.300912.
MacDonald JM, Stokes RJ, Cohen DA, Kofner A, Ridgeway GK. The effect of light rail transit on body mass index and physical activity. Am J Prev Med. 2010;39(2):105–12. https://doi.org/10.1016/j.amepre.2010.03.016.
Chang A, Miranda-Moreno L, Cao J, Welle B. The effect of BRT implementation and streetscape redesign on physical activity: a case study of Mexico City. Transp Res Part A Policy Pract. 2017;100:337–47. https://doi.org/10.1016/j.tra.2017.04.032.
Craig P, Cooper C, Gunnell D, et al. Using natural experiments to evaluate population health interventions: new medical research council guidance. J Epidemiol Community Health (1978). 2012;66(12):1182–6. https://doi.org/10.1136/jech-2011-200375.
Sun G, Choe EY, Webster C. Natural experiments in healthy cities research: how can urban planning and design knowledge reinforce the causal inference? Town Planning Review. Published online 2022:1–33.
Craig P, Katikireddi V, Leyland A, Popham F. Natural experiments: an overview of methods, approaches, and contributions to public health intervention research. Published online. 2017. https://doi.org/10.1146/annurev-publhealth.
Panter J, Heinen E, Mackett R, Ogilvie D. Impact of new transport infrastructure on walking, cycling, and physical activity. Am J Prev Med. 2016;50(2):e45–53.
Miller HJ, Tribby CP, Brown BB, et al. Public transit generates new physical activity: evidence from individual GPS and accelerometer data before and after light rail construction in a neighborhood of Salt Lake City, Utah, USA. Health Place. 2015;36:8–17. https://doi.org/10.1016/j.healthplace.2015.08.005.
Hong A, Boarnet MG, Houston D. New light rail transit and active travel: a longitudinal study. Transp Res Part A Policy Pract. 2016;92:131–44. https://doi.org/10.1016/j.tra.2016.07.005.
Sun G, Zhao J, Webster C, Lin H. New metro system and active travel: a natural experiment. Environ Int. 2020;138:105605. https://doi.org/10.1016/j.envint.2020.105605.
Hirsch JA, DeVries DN, Brauer M, Frank LD, Winters M. Impact of new rapid transit on physical activity: a meta-analysis. Prev Med Rep. 2018;10(January):184–90. https://doi.org/10.1016/j.pmedr.2018.03.008.
Xiao C, Goryakin Y, Cecchini M. Physical activity levels and new public transit: a systematic review and meta-analysis. Am J Prev Med. 2019;56(3):464–73. https://doi.org/10.1016/j.amepre.2018.10.022.
Huang R, Moudon AV, Zhou C, Stewart OT, Saelens BE. Light rail leads to more walking around station areas. J Transp Health. 2017;6:201–8. https://doi.org/10.1016/j.jth.2017.02.002.
Saelens BE, Moudon AV, Kang B, Hurvitz PM, Zhou C. Relation between higher physical activity and public transit use. Am J Public Health. 2014;104(5):854–9. https://doi.org/10.2105/AJPH.2013.301696.
Christian TJ. Trade-offs between commuting time and health-related activities. J Urban Health. 2012;89(5):746–57. https://doi.org/10.1007/s11524-012-9678-6.
Laverty AA, Webb E, Vamos EP, Millett C. Associations of increases in public transport use with physical activity and adiposity in older adults. International Journal of Behavioral Nutrition and Physical Activity. 2018;15(1). https://doi.org/10.1186/s12966-018-0660-x
Sun G, Webster C, Zhang X. Connecting the city: a three-dimensional pedestrian network of Hong Kong. Environ Plan B Urban Anal City Sci. 2021;48(1):60–75. https://doi.org/10.1177/2399808319847204.
Szeto WY, Yang L, Wong RCP, Li YC, Wong SC. Spatio-temporal travel characteristics of the elderly in an ageing society. Travel Behav Soc. 2017;9:10–20. https://doi.org/10.1016/j.tbs.2017.07.005.
Sun G, Du Y, Ni MY, Zhao J, Webster C. Metro and elderly health in Hong Kong: protocol for a natural experiment study in a high-density city. BMJ Open. 2021;11(3):1–8. https://doi.org/10.1136/bmjopen-2020-043983.
Lohne-Seiler H, Hansen BH, Kolle E, Anderssen SA. Accelerometer-determined physical activity and self-reported health in a population of older adults (65–85 years): a cross-sectional study. BMC Public Health. 2014;14(1):1–10. https://doi.org/10.1186/1471-2458-14-284.
Aadland E, Ylvisåker E. Reliability of the actigraph GT3X+ accelerometer in adults under free-living conditions. PLoS ONE. 2015;10(8):1–11. https://doi.org/10.1371/journal.pone.0134606.
Trost SG, Mciver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(11 SUPPL.):531–43. https://doi.org/10.1249/01.mss.0000185657.86065.98.
Cerin E, van Dyck D, Zhang CJP, van Cauwenberg J, Lai PC, Barnett A. Urban environments and objectively-assessed physical activity and sedentary time in older Belgian and Chinese community dwellers: potential pathways of influence and the moderating role of physical function. Int J Behav Nutr Phys Act. 2020;17(1):1–15. https://doi.org/10.1186/s12966-020-00979-8.
Saelens BE, Moudon AV, Kang B, Hurvitz PM, Zhou C. Relation between higher physical activity and public transit use. Am J Public Health. 2014;104(5):854–9. https://doi.org/10.2105/AJPH.2013.301696.
Barnett A, van den Hoek D, Barnett D, Cerin E. Measuring moderate-intensity walking in older adults using the ActiGraph accelerometer. BMC Geriatr. 2016;16(1):1–10. https://doi.org/10.1186/s12877-016-0380-5.
Zhao J, Sun G, Webster C. Walkability scoring: why and how a three-demensional pedestrian network matters? Environ Plan B Urban Anal City Sci. Published online 2020:1–20. https://doi.org/10.1177/2399808320977871
Sun G, Webster C, Ni MY, Zhang X. Measuring high-density built environment for public health research: uncertainty with respect to data, indicator design and spatial scale. Geospat Health. 2018;13(1):35–47. https://doi.org/10.4081/gh.2018.653.
Wing C, Simon K, Bello-Gomez RA. Designing difference in difference studies: best practices for public health policy research. Annu Rev Public Health. 2018;39:453–69. https://doi.org/10.1146/annurev-publhealth-040617-013507.
Craig P, Cooper C, Gunnell D, et al. 2012 Using natural experiments to evaluate population health interventions: new medical research council guidance. J Epidemiol Community Health. 1978;66(12):1182–6. https://doi.org/10.1136/jech-2011-200375.
Dunning T. Natural experiments in the social sciences: a design-based approach. Cambridge University Press; 2012. https://doi.org/10.1017/cbo9781139084444.
Hirsch JA, DeVries DN, Brauer M, Frank LD, Winters M. Impact of new rapid transit on physical activity: a meta-analysis. Prev Med Rep. 2018;10(January):184–90. https://doi.org/10.1016/j.pmedr.2018.03.008.
Gomersall SR, Rowlands AV, English C, Maher C, Olds TS. The activitystat hypothesis. Sports Med. 2013;43(2):135–49.
Rowland TW. The biological basis of physical activity. Med Sci Sports Exerc. 1998;30(3):392–9.
Brondeel R, Wasfi R, Perchoux C, et al. Is older adults’ physical activity during transport compensated during other activities? Comparing 4 study cohorts using GPS and accelerometer data. J Transp Health. 2019;12:229–36. https://doi.org/10.1016/j.jth.2019.02.006.
Melanson EL. The effect of exercise on non-exercise physical activity and sedentary behavior in adults. Obes Rev. 2017;18:40–9. https://doi.org/10.1111/obr.12507.
He D, Sun G, de Vos J, Webster C. The effects of metro interventions on physical activity and walking among older adults: a natural experiment in Hong Kong. Health Place. 2022;78:102939. https://doi.org/10.1016/j.healthplace.2022.102939.
Cerin E, Barnett A, Cheung M-C, Sit CHP, Macfarlane DJ, Chan W-M. Reliability and validity of the IPAQ-L in a sample of Hong Kong Urban older adults: does neighborhood of residence matter? J Aging Phys Act. 2012;20(4):402–20.
Choe EY, Du Y, Sun G. Decline in older adults’ daily mobility during the COVID-19 pandemic: the role of individual and built environment factors. BMC Public Health. 2022;22(1). https://doi.org/10.1186/s12889-022-14780-8
Acknowledgements
This study is funded by the Research Grants Council (RGC) of Hong Kong (17600818).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Guibo Sun is the corresponding author.
The original version of this article was revised: The equation in the Statistical Analysis section of the article has been corrected.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Choe, E.Y., He, D. & Sun, G. Trading-Off Transit and Non-Transit Physical Activity among Older People: Evidence from Longitudinal Accelerometer Data of a Natural Experiment Study. J Urban Health 100, 408–417 (2023). https://doi.org/10.1007/s11524-022-00709-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-022-00709-4