Abstract
Hypertension affects a large proportion of urban African-American older adults. While there have been great strides in drug development, many older adults do not have access to such medicines or do not take them. Mindfulness-based stress reduction (MBSR) has been shown to decrease blood pressure in some populations. This has not been tested in low-income, urban African-American older adults. Therefore, the primary purpose of this pilot study was to test the feasibility and acceptability of a mindfulness-based program for low income, minority older adults provided in residence. The secondary purpose was to learn if the mindfulness-based program produced differences in blood pressure between the intervention and control groups. Participants were at least 62 years old and residents of a low-income senior residence. All participants were African-American, and one was male. Twenty participants were randomized to the mindfulness-based intervention or a social support control group of the same duration and dose. Blood pressure was measured with the Omron automatic blood pressure machine at baseline and at the end of the 8-week intervention. A multivariate regression analysis was performed on the difference in scores between baseline and post-intervention blood pressure measurements, controlling for age, education, smoking status, and anti-hypertensive medication use. Effect sizes were calculated to quantify the magnitude of the relationship between participation in the mindfulness-based intervention and the outcome variable, blood pressure. Attendance remained >80% in all 8 weeks of both the intervention and the control groups. The average systolic blood pressure decreased for both groups post-intervention. Individuals in the intervention group exhibited a 21.92-mmHg lower systolic blood pressure compared to the social support control group post-intervention and this value was statistically significant (p = 0.020). The average diastolic blood pressure decreased in the intervention group post-intervention, but increased in the social support group. Individuals in the intervention group exhibited a 16.70-mmHg lower diastolic blood pressure compared to the social support group post-intervention, and this value was statistically significant (p = 0.003). Older adults are at a time in life when a reflective, stationary intervention, delivered in residence, could be an appealing mechanism to improve blood pressure. Given our preliminary results, larger trials in this hypertensive study population are warranted.
Similar content being viewed by others
Introduction
Despite years of public health interventions, the development and widespread use of effective medications, and a public health emphasis on identifying the causes and consequences of hypertension, blood pressure continues to be elevated in 59.5% of African-Americans.1 Hypertension results in significant morbidity in the form of congestive heart failure2 and stroke,3 and increases the risk of premature mortality,4 suggesting the need to develop sustainable, low-cost, and effective interventions to engage participants at risk, such as African-American older adults. This paper reports the pilot study of just such an intervention.
Currently, there is evidence to suggest that mindfulness meditation can lower blood pressure;5–7 therefore, we elected the implementation of a mindfulness-based program in a Baltimore City senior housing facility. Rooted in Buddhist tradition and formally developed by Jon Kabat-Zinn8 in 1979, mindfulness-based stress reduction (MBSR) programs are founded upon an active awareness of physical and mental states and teach participants to concentrate on breathing, and to relax their minds and bodies. While there has been some research on meditation and blood pressure,5–7 there have been few randomized clinical trials. To our knowledge, there are no mindfulness-based trials targeting hypertension in older adults, who are at the highest risk and therefore, may have the greatest benefit.
Previous trials of mindfulness-based programs have demonstrated their efficacy in improving psychological and physiological health outcomes in both healthy and clinical populations. A meta-analysis of MBSR in patients with chronic medical diseases showed positive effects on depression, anxiety, and psychological distress in people with chronic somatic diseases.9 Additionally, a meta-analysis of healthy adults who participated in MBSR showed reduced self-reported stress levels in healthy young and middle-aged adults.10 In addition to improved psychosocial health, MBSR has also improved physiological outcomes. Using a heterogeneous patient sample, investigators found that patients who participated in an 8-week MBSR program showed significant improvements in the inflammatory marker, C-reactive protein (CRP), as well as anxiety and overall distress post-intervention.11 Furthermore, research has demonstrated that meditation practice counters the effect of physiologic stress responses by decreasing respiratory rates, total peripheral vascular resistance, and cortisol, the prototypical biological indicator of stress and aging.12 All of these effects led us to hypothesize that MBSR might lower blood pressure in low-income, older African-American adults.
Although trials of MBSR have shown that it is a successful health promotion program, existing trials have had substantial limitations. MBSR trials to date have primarily included only young and middle-aged working adults13 or adolescents.14 Minimal evidence exists for the efficacy of MBSR programs with older adults. The few MBSR studies that have included older adults are limited to older individuals with lower chronic back pain.15 MBSR interventions have been most commonly implemented in specific clinical populations, such as cancer patients,16 individuals with chronic pain,17 transplant patients,18 or individuals with rheumatoid arthritis;19 however, these studies did not evaluate the impact of the age of the participants, or biological markers that may predict healthier aging. In addition, most of these studies were also conducted outside of the patient’s home. One MBSR interventional study did report an improvement in the quality of life and reduction in symptoms of depression among nursing home residents; however, this study was conducted in nursing home residents residing in Germany, and did not examine the impact of the intervention on hypertension risks.20 To address previous gaps in mindfulness-based research, this study was undertaken in a sample of in-residence, low-income African-American older adults, who are at high risk for hypertension and in need of low-cost interventions, but have not been systematically studied with regards to the effect of mindful-based interventions.
The primary aim of this pilot study was to test the feasibility of a mindfulness-based intervention, based on the principles and practices of the MBSR program, to develop mindfulness and social and emotional skills, and to decrease blood pressure in a sample of low-income, urban African-American older adults.
Methods
Design
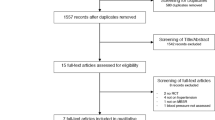
This pilot study was a prospective randomizedc ontrolled trial of an adaptation of a mindfulness-based intervention, called ELDERSHINE. Participants were recruited to participate from a low-income senior housing facility in Baltimore City. This site had not previously been exposed to any mindfulness programs. Inclusion into the study was restricted to African-Americans aged 62 years or older who were living in the building at the time of the baseline interview and had no plans to move. All participants enrolled in the study spoke English. We did not exclude individuals on anti-hypertensive medications but did account for medication use in the analyses. Participants who met these inclusion/exclusion criteria and who completed the consent form and baseline questionnaires were randomized to either the 8-week ELDERSHINE intervention or a social support control group. All subjects were followed-up through the 8-week program and re-evaluated post-intervention using the same questionnaires administered at the baseline interview.
Sample
This study was approved by the Johns Hopkins University Institutional Review Board. African-American older adults aged 62 years or older were recruited from a Baltimore City senior housing facility to be a part of the mindfulness-based ELDERSHINE program. Participants were informed about the study through informational sessions, flyers, and tabling at the facility. Interested participants were first fully informed of the study and the process of randomization in which they would have an equal chance of being selected into the mindfulness-based intervention or social support control group. Once informed consent was received, those choosing to participate underwent a baseline assessment. Subsequently, participants were randomized to either the mindfulness-based intervention or social support control group. All participants were compensated for their time with a $25 gift card upon completion of each survey time point (baseline and 8 weeks).
Twenty subjects consented and enrolled in the study. Of the 20 subjects, 12 were randomized to the intervention group and eight were randomized to the social support group. The groups were not expected to be balanced due to the small pilot sample size (Table 1).
Measures
Basic demographic information including birth date, race, number of years of education completed, and smoking history was collected at baseline. Perceived stress was also collected at baseline.21 Outcome measurements were obtained before randomization and after completion of the 8-week group sessions. All outcome measures were assessed for both the mindfulness-based intervention and social support control groups. The outcome assessment included blood pressure measurements.
Blood Pressure
To measure their blood pressure, participants were instructed to sit quietly for 5 minutes while three blood pressure measurements were taken on their right arm, each separated by 1 minute. All blood pressure measurements were recorded and the mean of the three measurements was calculated. Participant’s blood pressures were measured using the OMRON HEM-907XL electronic blood pressure machine with four available cuffs sizes (from small adult to morbidly obese).22 Participants were instructed to sit quietly, with their arm in a still position, and both feet uncrossed and on the floor to ensure an accurate measurement.
Intervention
The intervention, a mindfulness-based program called ELDERSHINE, was an 8-week curriculum designed to teach older adults how to manage their mental and physical health through mindfulness meditation and social and emotional skills development. All sessions were developed and implemented by an interventionist trained in MBSR through the Center for Mindfulness at the University of Massachusetts. The sessions were held once a week for 90 minutes and consisted of an opening meditation, sharing of successes, a review of home practices, a lesson to practice and apply mindfulness skills to self-care and interpersonal relationships, a guided breath meditation, a closing meditation, an invitation to do specific home practices, and a healthy fruit-and-vegetable snack. All activities were done in a group setting to allow individuals to learn and benefit from the experiences of others. The sessions took place in a group room on the first floor of the senior housing facility. Participants were seated in comfortable chairs during the meetings. Participants were called the night before as an attendance reminder and attendance was noted on the day of each session. A list of topics covered at the weekly sessions is displayed in Table 2.
Control Group
The control group was a social support group. Designed to match the time frame and attention received by the intervention group, the social support control group also convened for 90 minutes each week for 8 weeks. Two research assistants guided the group by recording attendance and introducing the topic to be discussed by members of the group, but no mindfulness teaching or practices were offered during these meetings. To initiate communication among participants, the research assistants provided pre-planned conversation starters that mirrored the topics in the intervention group. Following the session, participants were offered a fruit-and-vegetable snack identical to the foods served to the intervention group. The sessions took place in a group room on the first floor of the senior housing facility. Participants were seated comfortably during the meetings. Participants were called the night before as an attendance reminder and attendance was noted on the day of each session.
Fidelity
A research fidelity plan was developed for this study based on the NIH behavior change consortium.23 The design of the study included interventions that were distinct and based on theory. Group training was conducted using an intervention manual and separate interventionists for each group. To ensure a successful delivery of the intervention, subjects were given reminder calls the night before and just prior to the intervention, and attendance was recorded by date and amount of time per session. Participant reception to the intervention was evaluated through observation by an additional member of the study team, and a checklist completed weekly to observe participant engagement in the group.
Analysis
Descriptive statistics were compared for individuals in the intervention and social support groups. Frequencies and percentages were used to summarize categorical data, and means, medians, and standard deviations were used to summarize continuous data.
We first conducted an unadjusted model comparing the changes in blood pressure measurements from baseline to post-intervention between the intervention and social support groups. This was followed by a multivariate regression analysis comparing the difference in blood pressure measurements from baseline to post-intervention between the intervention and social support groups, adjusting for age, education, smoking status, and anti-hypertensive medication use.
Effect sizes were calculated to quantify the magnitude of the relationship between participation in the mindfulness-based intervention and the outcome variable, blood pressure.
Results
Subject Characteristics
As shown in Table 1, there were no differences between the intervention and social support groups in demographic and clinical measures at baseline, including age, race, systolic blood pressure, heart rate, years of education, perceived stress and ever smoking status (all p > 0.1). At baseline, individuals in the intervention group exhibited a higher average diastolic blood pressure (p = 0.049).Three participants were normotensive, and four participants were pre-hypertensive at baseline. Thirteen participants had hypertension, stage I (n = 7) or stage II (n = 6), at baseline. Eighteen participants were on an antihypertensive medication from one or more of the following classes of antihypertensive agents: ACE Inhibitors, Angiotensin II Receptor Blockers, Beta Blockers, Calcium Channel Blockers, and Diuretics. Two participants were on no medications and 18 were on an average of six medications. In addition to hypertension, the most common comorbid conditions included gastroesophageal reflux disease (GERD) (45%), high cholesterol (40%), diabetes (35%), and asthma/COPD (25%). Other less common conditions include gout, osteoporosis, and hypothyroidism.
At the end of the 8-week intervention and social support group programs, 12 subjects remained in the intervention group and eight subjects remained in the social support group. Attendance at weekly group sessions remained >80% for all 8 weeks of both the intervention and the social support control groups.
Comparison of Blood Pressure in the Intervention and Control Groups
Table 3 reflects the absolute changes in systolic and diastolic blood pressures from baseline to follow-up in both the intervention and social support groups. Table 4 presents the findings for the multivariate regression comparing blood pressure measurements between the intervention and social support control groups. The average systolic blood pressure decreased for both groups post-intervention. Comparing the differences between post-intervention and baseline measurements, individuals in the intervention group exhibited a 21.92-mmHg lower systolic blood pressure compared to the social support control group and this value was statistically significant (p = 0.020).At baseline, individuals in the intervention group had a higher average diastolic blood pressure compared to the social support group. The average diastolic blood pressure decreased in the intervention group post-intervention, but increased in the social support group. Comparing the differences between post-intervention and baseline measurements, individuals in the intervention group exhibited a 16.70-mmHg lower diastolic blood pressure compared to the social support control group and this value was statistically significant (p = 0.003).
Discussion
Results from this pilot study provide preliminary evidence to suggest that 8 weeks of the mindfulness-based ELDERSHINE program improves blood pressure outcomes in low-income, urban African-American older adults. Compared to individuals in the social support group, those who participated in the intervention program had a lower mean systolic and diastolic blood pressure post 8-week intervention.
These pilot results are consistent with previous studies that examined the effectiveness of mindfulness-based interventions. Although this study was undertaken in a different study population, it supports previous studies that show that mindfulness-based interventions result in reductions in blood pressure readings in samples of breast cancer survivors,5 type II diabetics,6 and breast and prostate cancer patients.7 In addition, our pilot results show that the mindfulness- based ELDERSHINE program is feasible to implement in a low-income housing residence center that serves older adults. Attendance at all eight weekly sessions was >80% with active participation from most participants. Participants in both groups had positive experiences to share about the study. Utilizing information from a short questionnaire asking participants about their overall study experience, participants stated, “I wait the whole week for ELDERSHINE,” and “ELDERSHINE is my safety net.”
Previous studies of mindfulness-based interventions have been primarily undertaken in specific populations of clinical patients. This is one of the first studies to test whether MBRS can decrease blood pressure in low-income African-American older adults with high hypertension prevalence but who are not a specific clinical population. Based on our findings, low-income individuals, who often suffer from chronic psychological stress, do benefit from participating in this mindfulness-based program. We have shown in this study that low-income African-American older adults with no specific clinical history can exhibit reduced blood pressure.
The results from this study provide evidence for the utilization of this low cost intervention to potentially improve blood pressure. All sessions were developed and implemented by an interventionist trained in MBSR through the Center for Mindfulness at the University of Massachusetts. The interventionist, who has more than 15 years experience with Mindfulness-based programs, has developed a train-the-trainer module that allows for cost-effective translation of this program.
Limitations
There is the possibility of contamination across study groups. Three factors indicate that this is not a problem in this study design. First, in the 3 years that this program was offered at another Baltimore senior housing facility (not for research purposes), no one outside the program initiated a meditation practice as a result of conversations with program members. Second, in the follow-up interviews with the social support-control group participants, no participants reported practicing aspects of the intervention. Third, if the social support group participants did practice aspects of the intervention and failed to report it at the follow-up interview, it would undermine our ability to detect a difference between groups. However, we did find a significant difference between the groups.
Conclusion
Given our preliminary results for the benefits of learning and practicing mindfulness, larger trials in this at risk study population are warranted. Even with a small sample size, this study provides evidence for improved blood pressure for low-income African-American older adults participating in a mindfulness-based intervention. These findings suggest that the large disparities in health outcomes between individuals of lower and higher socioeconomic strata may be narrowed with increased access to health promotion programs, such as ELDERSHINE, for low-income individuals.
References
Mujahid MS, Diez Roux AV, Cooper RC, Shea S, Williams DR. Neighborhood stressors and race/ethnic differences in hypertension prevalence (The Multi-Ethnic Study of Atherosclerosis). Am J Hypertens. 2011; 24(2): 187–193.
Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011; 8: 30–41.
Lenfant C, Chobanian AV, Jones DW, Roccella EJ. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension. 2003; 41(6): 1178–1179.
Levine RS, Foster JE, Fullilove RE, et al. Black-white inequalities in mortality and life expectancy, 1933–1999: implications for healthy people 2010. Public Health Rep. 2001; 116(5): 474–483.
Matchim Y, Armer JM, Stewart BR. Effects of Mindfulness-Based Stress Reduction (MBSR) on health among breast cancer survivors. West J Nurs Res. 2010; 33(8): 996–1016.
Rosenzweig S, Reibel DK, Greeson JM, et al. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Altern Ther Health Med. 2007; 13(5): 36–38.
Carlson LE, Speca M, Faris P, Patel KD. One year pre–post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. 2007; 21(8): 1038–1049.
Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982; 4(1): 33–47.
Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. J Psychosom Res. 2010; 68(6): 539–544.
Chiesa A, Serretti A. Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. J Altern Complement Med. 2009; 15(5): 593–600.
Fang CY, Reibel DK, Longacre ML, Rosenzweig S, Campbell DE, Douglas SD. Enhanced psychosocial well-being following participation in a mindfulness-based stress reduction program is associated with increased natural killer cell activity. J Altern Complement Med. 2010; 16(5): 531–538.
Curiati JA, Bocchi E, Freire JO, et al. Meditation reduces sympathetic activation and improves the quality of life in elderly patients with optimally treated heart failure: a prospective randomized study. J Altern Complement Med. 2005; 11(3): 465–472.
Klatt MD, Buckworth J, Malarkey WB. Effects of low-dose mindfulness-based stress reduction (MBSR-ld) on working adults. Health Educ Behav. 2009; 36(3): 601–614.
Biegel GM, Brown KW, Shapiro SL, Schubert CM. Mindfulness-based stress reduction for the treatment of adolescent psychiatric outpatients: a randomized clinical trial. J Consult Clin Psychol. 2009; 77(5): 855–866.
Morone NE, Rollman BL, Moore CG, Li Q, Weiner DK. A mind–body program for older adults with chronic low back pain: results of a pilot study. Pain Med. 2009; 10(8): 1395–1407.
Birnie K, Garland SN, Carlson LE. Psychological benefits for cancer patients and their partners participating in mindfulness-based stress reduction (MBSR). Psychooncology. 2009; 19(9): 1004–1009.
Rosenzweig S, Greeson JM, Reibel DK, Green JS, Jasser SA, Beasley D. Mindfulness-based stress reduction for chronic pain conditions: variation in treatment outcomes and role of home meditation practice. J Psychosom Res. 2010; 68(1): 29–36.
Gross CR, Kreitzer MJ, Reilly-Spong M, Winbush NY, Schomaker EK, Thomas W. Mindfulness meditation training to reduce symptom distress in transplant patients: rationale, design, and experience with a recycled waitlist. Clin Trials. 2009; 6(1): 76–89.
Pradhan EK, Baumgarten M, Langenberg P, et al. Effect of Mindfulness-Based Stress Reduction in rheumatoid arthritis patients. Arthritis Rheum. 2007; 57(7): 1134–1142.
Ernst S, Welke J, Heintze C, et al. Effects of mindfulness-based stress reduction on quality of life in nursing home residents: a feasibility study. Forsch Komplementmed. 2008; 15(2): 74–81.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983; 24(4): 385–396.
White WB, Anwar YA. Evaluation of the overall efficacy of the Omron office digital blood pressure HEM-907 monitor in adults. Blood Press Monit. 2001; 6(2): 107–110.
Bellg AJ, Borrelli B, Resnick B, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004; 23(5): 443–451.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Palta, P., Page, G., Piferi, R.L. et al. Evaluation of a Mindfulness-Based Intervention Program to Decrease Blood Pressure in Low-Income African-American Older Adults. J Urban Health 89, 308–316 (2012). https://doi.org/10.1007/s11524-011-9654-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-011-9654-6