Abstract
Background
Myeloid-derived suppressor cells (MDSCs) were linked to pathologic stage in bladder urothelial carcinoma (UC). Neutrophil lymphocyte ratio (NLR) is an inflammatory biomarker with a prognostic role in metastatic (m)UC.
Objective
We hypothesized that MDSC levels correlate with NLR and overall survival (OS) in mUC.
Patients and methods
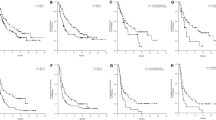
MDSCs were measured in blood samples from patients with mUC in fresh unfractionated whole blood (WB) and peripheral blood mononuclear cells (PBMC) by flow cytometry and defined as LinloCD33+/HLADR- (Total MDSC). MDSC subsets were defined as polymorphonuclear (PMN-MDSC: CD15+/CD14−), monocytic (M-MDSC: CD15−/CD14+), and uncommitted (UNC-MDSC: CD15−/CD14−). MDSC populations were presented as a percentage of live nucleated blood cells. Spearman’s rank correlation assessed correlations between MDSC and NLR. Kaplan–Meier curves and log-rank test estimated OS from the time of MDSC collection to last follow-up or date of death.
Results
Of the 76 patients, 78% were men and 43% were never smokers with a median age of 69 years (range 31–83); 72% had pure UC and 76% had lower tract UC. Prior therapies included intravesical therapy (22%), neoadjuvant chemotherapy (30%), cystectomy or nephroureterectomy (55%). Median follow-up for all patients was 12 months (0.6–36.5). PMN-MDSC was the predominant subset in WB and PBMC. There was significant correlation between individual MDSC subsets in WB and PBMC (p ≤ 0.001). Both WB UNC-MDSC/PMN-MDSC ratios (rho = − 0.27, p = 0.03) and PBMC UNC-MDSC/PMN-MDSC (rho = − 0.28, p = 0.02) were negatively correlated with NLR. Median OS was 17.7 months (95% CI: 11.0–NE). Overall 1-year and 3-year survival rates were 0.60 (95% CI 0.49–0.73) and 0.15 (95% CI 0.03–0.67), respectively. Higher WB UNC-MDSC levels (HR 3.78, p = 0.0022) and higher NLR (HR 2.6, p = 0.0179) were associated with shorter OS.
Conclusions
Specific MDSC subsets correlate with NLR. Higher WB UNC-MDSC levels and higher NLR were negative prognostic factors. Given the feasibility of serial blood draws, dynamic assessment of MDSC over time and further validation with longer follow-up are warranted.


Similar content being viewed by others
References
Key Statistics for Bladder Cancer [Internet]. [cited 2019 Jan 7]; https://www.cancer.org/cancer/bladder-cancer/about/key-statistics.html. Accessed 7 Jan 2019.
Andreassen BK, Aagnes B, Gislefoss R, Andreassen M, Wahlqvist R. Incidence and Survival of urothelial carcinoma of the urinary bladder in Norway 1981–2014. BMC Cancer. 2016;16:799.
Mari A, Campi R, Tellini R, et al. Patterns and predictors of recurrence after open radical cystectomy for bladder cancer: a comprehensive review of the literature. World J Urol. 2018;36(2):157–70.
Mitra AP, Quinn DI, Dorff TB, et al. Factors influencing post-recurrence survival in bladder cancer following radical cystectomy. BJU Int. 2012;109(6):846–54.
Bladder Cancer–Cancer Stat Facts [Internet]. SEER. [cited 2019 Jan 7]; https://seer.cancer.gov/statfacts/html/urinb.html.
Tang X, Du P, Yang Y. The clinical use of neutrophil-to-lymphocyte ratio in bladder cancer patients: a systematic review and meta-analysis. Int J Clin Oncol. 2017;22(5):817–25.
Wu S, Zhao X, Wang Y, et al. Pretreatment neutrophil-lymphocyte ratio as a predictor in bladder cancer and metastatic or unresectable urothelial carcinoma patients: a pooled analysis of comparative studies. Cell Physiol Biochem. 2018;46(4):1352–64.
Gabrilovich DI. Myeloid-derived suppressor cells. Cancer Immunol Res. 2017;5(1):3–8.
Bronte V, Dmitry I. Poster : Myeloid-derived suppressor cells. Nat. Rev. Immunol. [cited 2019 Apr 17]; https://www.nature.com/nri/posters/mdscs/index.html.
Tannenbaum CS, Rayman PA, Pavicic PG, et al. Mediators of inflammation-driven expansion, trafficking, and function of tumor-infiltrating MDSCs. Cancer Immunol Res. 2019. https://doi.org/10.1158/2326-6066.CIR-18-0578.
Allavena P, Mantovani A. Immunology in the clinic review series; focus on cancer: tumour-associated macrophages: undisputed stars of the inflammatory tumour microenvironment. Clin Exp Immunol. 2012;167(2):195–205.
Gabrilovich DI, Ostrand-Rosenberg S, Bronte V. Coordinated regulation of myeloid cells by tumours. Nat Rev Immunol. 2012;12(4):253–68.
Umansky V, Blattner C, Gebhardt C, Utikal J. The role of myeloid-derived suppressor cells (MDSC) in cancer progression. Vaccines. 2016;4(4):36.
Fleming V, Hu X, Weber R, et al. Targeting myeloid-derived suppressor cells to bypass tumor-induced immunosuppression. Front Immunol. 2018;9:398.
Mantovani A. The growing diversity and spectrum of action of myeloid-derived suppressor cells. Eur J Immunol. 2010;40(12):3317–20.
Diaz-Montero CM, Salem ML, Nishimura MI, Garrett-Mayer E, Cole DJ, Montero AJ. Increased circulating myeloid-derived suppressor cells correlate with clinical cancer stage, metastatic tumor burden, and doxorubicin–cyclophosphamide chemotherapy. Cancer Immunol Immunother. 2009;58(1):49–59.
Veglia F, Perego M, Gabrilovich D. Myeloid-derived suppressor cells coming of age. Nat Immunol. 2018;19(2):108.
Yang G, Shen W, Zhang Y, et al. Accumulation of myeloid-derived suppressor cells (MDSCs) induced by low levels of IL-6 correlates with poor prognosis in bladder cancer. Oncotarget. 2017;8(24):38378–88.
Ornstein MC, Diaz-Montero CM, Rayman PA, et al. Serial measurements of myeloid derived suppressor cells (MDSC) in metastatic urothelial carcinoma (mUC) patients (pts) treated with immune checkpoint inhibitors (CI). J Clin Oncol. 2017;35(15_suppl):e16005.
Tzeng A, Diaz-Montero CM, Rayman PA, et al. Immunological correlates of response to immune checkpoint inhibitors in metastatic urothelial carcinoma. Target Oncol. 2018;13(5):599–609.
Formica V, Luccchetti J, Cunningham D, et al. Systemic inflammation, as measured by the neutrophil/lymphocyte ratio, may have differential prognostic impact before and during treatment with fluorouracil, irinotecan and bevacizumab in metastatic colorectal cancer patients. Med Oncol. 2014;31(9):166.
Zhu Z, Shen Z, Xu C. Inflammatory pathways as promising targets to increase chemotherapy response in bladder cancer. Mediat Inflamm. 2012;2012:528690.
Marchioni M, Primiceri G, Ingrosso M, et al. The clinical use of the neutrophil to lymphocyte ratio (NLR) in urothelial cancer: a systematic review. Clin Genitourin Cancer. 2016;14(6):473–84.
Meyer C, Cagnon L, Costa-Nunes CM, et al. Frequencies of circulating MDSC correlate with clinical outcome of melanoma patients treated with ipilimumab. Cancer Immunol Immunother. 2014;63(3):247–57.
Wu K, Tan M-Y, Jiang J-T, et al. Cisplatin inhibits the progression of bladder cancer by selectively depleting G-MDSCs: a novel chemoimmunomodulating strategy. Clin Immunol. 2018;193:60–9.
Ornstein MC, Diaz-Montero CM, Rayman P, et al. Myeloid-derived suppressors cells (MDSC) correlate with clinicopathologic factors and pathologic complete response (pCR) in patients with urothelial carcinoma (UC) undergoing cystectomy. Urol Oncol Semin Orig Investig. 2018;36(9):405–12.
Weide B, Martens A, Zelba H, et al. Myeloid-derived suppressor cells predict survival of patients with advanced melanoma: comparison with regulatory T cells and NY-ESO-1- or melan-A-specific T cells. Clin Cancer Res. 2014;20(6):1601–9.
Lucca I, Jichlinski P, Shariat SF, et al. The neutrophil-to-lymphocyte ratio as a prognostic factor for patients with urothelial carcinoma of the bladder following radical cystectomy: validation and meta-analysis. Eur Urol Focus. 2016;2(1):79–85.
Dumitru CA, Moses K, Trellakis S, Lang S, Brandau S. Neutrophils and granulocytic myeloid-derived suppressor cells: immunophenotyping, cell biology and clinical relevance in human oncology. Cancer Immunol Immunother. 2012;61(8):1155–67.
Chen M-F, Tsai M-S, Chen W-C, Chen P-T. Predictive Value of the pretreatment neutrophil-to-lymphocyte ratio in head and neck squamous cell carcinoma. J Clin Med 2018;7(10):294. https://doi.org/10.3390/jcm7100294.
Tesi RJ. MDSC; the most important cell you have never heard of. Trends Pharmacol Sci. 2019;40(1):4–7.
Ma P, Beatty PL, McKolanis J, Brand R, Schoen RE, Finn OJ. Circulating myeloid derived suppressor cells (MDSC) that accumulate in premalignancy share phenotypic and functional characteristics with MDSC in cancer. Front Immunol. 2019;10:1401.
Bruger AM, Dorhoi A, Esendagli G, et al. How to measure the immunosuppressive activity of MDSC: assays, problems and potential solutions. Cancer Immunol Immunother. 2019;68(4):631–44.
Blidner AG, Salatino M, Mascanfroni ID, et al. Differential response of myeloid-derived suppressor cells to the nonsteroidal anti-inflammatory agent indomethacin in tumor-associated and tumor-free microenvironments. J Immunol. 2015;194(7):3452–62.
Cassetta L, Baekkevold ES, Brandau S, et al. Deciphering myeloid-derived suppressor cells: isolation and markers in humans, mice and non-human primates. Cancer Immunol Immunother. 2019;68(4):687–97.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
No external funding was used in the preparation of this article.
Conflict of interest
Brian I. Rini declares research funding and consulting for Merck, BMS, Pfizer, Roche, Aveo. Jorge A. Garcia declares consulting for Merck, Janssen, Eisai, Astella, Seattle Genetics and speaking/education for Merck, Janssen and Bayer. Petros Grivas declares prior unrelated consulting for: AstraZeneca; Bayer; Biocept; Bristol-Myers Squibb; Clovis Oncology; Driver; EMD Serono; Exelixis; Foundation Medicine; Genentech; Genzyme; GlaxoSmithKline; Heron Therapeutics; Janssen; Merck & Co.; Mirati Therapeutics; Pfizer; Seattle Genetics; QED Therapeutics; Roche; research funding to institution: AstraZeneca, Bayer; Genentech/Roche; Merck & Co.; Mirati Therapeutics; Oncogenex; Pfizer, Clovis Oncology, Bavarian Nordic, Immunomedics, Debiopharm, Bristol-Myers Squibb. Moshe C. Ornstein declares grant support from Pfizer, BMS; speaking: BMS, Exelixis; education support: Pfizer; consulting: BMS, Pfizer, Exelixis. Iris Y. Sheng, Claudia Marcela Diaz-Montero, Patricia Rayman, Wei Wei, James H. Finke, Jin S. Kim, Paul G Pavicic Jr, Marcelo Lamenza, Donna Company, Andrew Stephenson, Steven Campbell, George Haber, Byron Lee, Omar Mian, and Timothy D. Gilligan declare that they have no conflicts of interest that might be relevant to the contents of this article.
Rights and permissions
About this article
Cite this article
Sheng, I.Y., Diaz-Montero, C.M., Rayman, P. et al. Blood Myeloid-Derived Suppressor Cells Correlate with Neutrophil-to-Lymphocyte Ratio and Overall Survival in Metastatic Urothelial Carcinoma. Targ Oncol 15, 211–220 (2020). https://doi.org/10.1007/s11523-020-00707-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-020-00707-z