Abstract
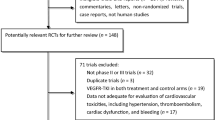
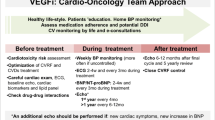
Anti-angiogenic targeted therapies are now major tools in the management of solid tumors. Briefly, one can distinguish between monoclonal antibodies such as bevacizumab directed against vascular endothelial growth factor (VEGF) and small molecules such as those targeted against receptors with tyrosine-kinase activity. Soon after they were marketed, these drugs showed cardiovascular toxicities, such as hypertension, left ventricular systolic dysfunction, heart failure and conduction abnormalities. The most frequent cardiovascular side effect of targeted therapies is hypertension, but the most life-threatening is QT prolongation with its risk of torsade de pointe and sudden cardiac death. Since the incidence of different types of cardiovascular side effects following targeted therapies varies across studies—and despite the fact that several meta-analyses attempted to summarize available information—those side effects are still not well identified. In addition, their reversibility is not precisely known. This review aims to present and discuss the various cardiovascular toxicities of anti-angiogenic targeted therapies for cancer.
Similar content being viewed by others
References
Folkman J (1971) Tumor angiogenesis: therapeutic implications. N Engl J Med 285:1182–1186
des Guetz G, Uzzan B, Nicolas P et al (2006) Microvessel density and VEGF expression are prognostic factors in colorectal cancer. Meta-analysis of the literature. Br J Cancer 94:1823–1832
Yang JC, Haworth L, Sherry RM et al (2003) A randomized trial of bevacizumab, an anti-vascular endothelial growth factor antibody, for metastatic renal cancer. N Engl J Med 349:427–434
Hurwitz H, Fehrenbacher L, Novotny W et al (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350:2335–2342
Yeh ETH, Tong AT, Lenihan DJ, Yusuf SW et al (2004) Cardiovascular complications of cancer therapy. Diagnosis, pathogenesis, and management. Circulation 109:3122–3131
Kabbinavar F, Hurwitz HI, Fehrenbacher L, Meropol NJ et al (2003) Phase II, randomized trial comparing bevacizumab plus fluorouracil (FU)/leucovorin (LV) with FU/LV alone in patients with metastatic colorectal cancer. J Clin Oncol 21:60–65
An MM, Zou Z, Shen H, Ping L et al (2010) Incidence and risk of significantly raised blood pressure in cancer patients treated with bevacizumab: an updated analysis. Eur J Clin Pharmacol 66:813–821
Chu TF, Rupnick MA, Kerkela R et al (2007) Cardiotoxicity associated with tyrosine kinase inhibitor sunitinib. Lancet 370:2011–2019
Veronese ML, Mosenkis A, Flaherty KT et al (2006) Mechanisms of hypertension associated with BAY 43–9006. J Clin Oncol 24:1363–1369
Wu S, Chen JJ, Kudelka A, Lu J et al (2008) Incidence and risk of hypertension with sorafenib in patients with cancer: a systematic review and meta-analysis. Lancet Oncol 9:117–123
Zhu X, Stergiopoulos K, Wu S (2009) Risk of hypertension and renal dysfunction with an angiogenesis inhibitor sunitinib: systematic review and meta-analysis. Acta Oncol 48:9–17
Nazer B, Humphreys BD, Moslehi J (2011) Effects of novel angiogenesis inhibitors for the treatment of cancer on the cardiovascular system. Focus on hypertension. Circulation 124:1687–1691
Mourad JJ, des Guetz G, Debbabi H, Levy BI (2008) Blood pressure rise following angiogenesis inhibition by bevacizumab. A crucial role for microcirculation. Ann Oncol 19:927–934
Zhu X, Wu S, Dahut WL, Parikh CR (2007) Risks of proteinuria and hypertension with bevacizumab, an antibody against vascular endothelial growth factor: systematic review and meta-analysis. Am J Kidney Dis 49:186–193
Eremina V, Quaggin SE (2010) Biology of anti-angiogenic therapy-induced thrombotic microangiopathy. Semin Nephrol 30:582–590
Eremina V, Jefferson JA, Kowalewska J, Hochster H et al (2008) VEGF inhibition and renal thrombotic microangiopathy. N Engl J Med 358:1129–1136
Scappaticci FA, Skillings JR, Holden SN et al (2007) Arterial thromboembolic events in patients with metastatic carcinoma treated with chemotherapy and bevacizumab. J Natl Cancer Inst 99:1232–1239
Ranpura V, Hapani S, Chuang J, Wu S (2010) Risk of cardiac ischemia and arterial thromboembolic events with the angiogenesis inhibitor bevacizumab in cancer patients: A meta-analysis of randomized controlled trials. Acta Oncol 49:287–297
Hurwitz HI, Saltz LB, van Cutsem E et al (2011) Venous thromboembolic events with chemotherapy plus bevacizumab: A pooled analysis of patients in randomized phase II and III studies. J Clin Oncol 29:1757–1754
Nalluri SR, Chu D, Keresztes R, Zhu X, Wu S (2008) Risk of venous thromboembolism with the angiogenesis inhibitor bevacizumab in cancer patients: a meta-analysis. JAMA 300:2277–2285
Hapani S, Sher A, Chu D, Wu S (2010) Increased risk of serious hemorrhage with bevacizumab in cancer patients: a meta-analysis. Oncology 79:27–38
Hang XF, Xu WS, Wang JX, Xin H et al (2011) Risk of high-grade bleeding in patients with cancer treated with bevacizumab: a meta-analysis of randomized controlled trials. Eur J Clin Pharmacol 67:613–623
Franco TH, Khan A, Joshi V, Thomas B (2008) Takotsubo cardiomyopathy in two men receiving bevacizumab for metastatic cancer. Ther Clin Risk Manag 4:1367–1370
Choueiri TK, Mayer EL, Je Y, Rosenberg JE et al (2011) Congestive heart failure risk in patients with breast cancer treated with bevacizumab. J Clin Oncol 29:632–638
Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM et al (2007) Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med 356:115–124
Motzer RJ, Rini BI, Bukowski RM, Curti BD et al (2006) Sunitinib in patients with metastatic renal cell carcinoma. JAMA 295:2516–2524
Escudier B, Eisen T, Stadler WM, Szczylik C et al (2007) Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med 356:125–134
Schmidinger M, Zielinski CC, Vogl UM, Bojic A et al (2008) Cardiac toxicity of sunitinib and sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol 26:5204–5212
Popat S, Smith IE (2008) Therapy insight: anthracyclines and trastuzumab-the optimal management of cardiotoxic side effects. Nature Clin Pract 5:324–335
Suter TM, Cook-Bruns N, Barton C (2004) Cardiotoxicity associated with trastuzumab (Herceptin) therapy in the treatment of metastatic breast cancer. The Breast 13:173–183
Kiura K, Nakagawa K, Shinkai T et al (2008) A randomized, double-blind, phase IIa dose-finding study of vandetanib (ZD6474) in Japanese patients with non-small cell lung cancer. J Thorac Oncol 3:386–393
Maitland ML, Bakris GL, Black HR et al (2010) Initial Assessment, Surveillance, and Management of Blood Pressure in Patients Receiving Vascular Endothelial Growth Factor Signaling Pathway Inhibitors. JNCI 102:596–604
Galfrascoli E, Piva S, Cinquini M et al (2011) Risk/benefit profile of bevacizumab in metastatic colon cancer: a systematic review and meta-analysis. Dig Liver Dis 43:286–294
Ranpura V, Hapani S, Wu S (2011) Treatment-related mortality with bevacizumab in cancer patients. A meta-analysis. JAMA 305:487–494
Boehm S, Rothermundt C, Hess D, Joerger M (2010) Antiangiogenic drugs in oncology: A focus on drug safety and the elderly-A mini-review. Gerontology 56:303–309
Ederhy S, Izzedine H, Massard C, Dufaitre G, Spano JP, et al (2011) Cardiac side effects of molecular targeted therapies: Towards a better dialogue between oncologists and cardiologists. Crit Rev Oncol Hematol 2011 Feb 15 [Epub ahead of print]
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
des Guetz, G., Uzzan, B., Chouahnia, K. et al. Cardiovascular toxicity of anti-angiogenic drugs. Targ Oncol 6, 197–202 (2011). https://doi.org/10.1007/s11523-011-0204-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-011-0204-7