Abstract
Mandible subcondylar fractures have very high complication rate, yet there is no consensus on suitable plate design for optimal patient outcomes. Our study is aimed at comparing single mini, trapezoid, lambda, strut and double mini plates. A finite-element (FE) model of intact mandible was developed based on healthy CT-scan data, which was further virtually osteotomized and fixated with plates. The cortical and cancellous bones were assigned region-specific orthotropic and heterogenous isotropic material properties respectively. The models were subjected to six load cases representing the mastication cycle. Under opposite lateralities, the tensile and compressive mandibular strain distributions were found as the opposite, with tensile strains at the posterior border under ipsilateral molar clenching (RMOL) resulting in lesser mandibular strain in reconstructed mandible with single mini plate under RMOL but highest mandibular strain under the contralateral molar clenching (LMOL). Owing to the reduced mandibular strains under LMOL than RMOL, the contralateral chewing is preferred during the immediate post-surgery period for patients. Under LMOL, the peak von Mises stresses in the plate decreased with increase in the number of screws. Furthermore, the presence of two arms in double mini and trapezoid plates seems beneficial to neutralise the tensile and compressive strains across load cases.
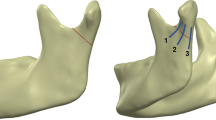
Graphical Abstract










Similar content being viewed by others
References
Gomez Rosello E, QuilesGranado AM, Artajona Garcia M, Juanpere Marti S, Laguillo Sala G, Beltran Marmol B, Pedraza Gutierrez S (2020) Facial fractures: classification and highlights for a useful report. Insights Imaging 11:49
Sukegawa S, Kanno T, Masui M, Sukegawa-Takahashi Y, Kishimoto T, Sato A, Furuki Y (2019) Which fixation methods are better between three-dimensional anatomical plate and two miniplates for the mandibular subcondylar fracture open treatment? J Craniomaxillofac Surg 47:771
Abdel-Galil K, Loukota R (2010) Fractures of the mandibular condyle: evidence base and current concepts of management. Br J Oral Maxillofac Surg 48:520
Nasser M, Pandis N, Fleming PS, Fedorowicz Z, Ellis E, Ali K (2013) Interventions for the management of mandibular fractures. Cochrane Database Syst Rev 7:CD006087
Hijazi L, Hejazi W, Darwich MA, Darwich K (2016) Finite element analysis of stress distribution on the mandible and condylar fracture osteosynthesis during various clenching tasks. Oral Maxillofac Surg 20:359
Adhikari M, Bhatt K, Yadav R, Mandal J, Bhutia O, Roychoudhury A (2021) Fixation of subcondylar fractures of the mandible: a randomized clinical trial comparing one trapezoidal plate with two miniplates. Int J Oral Maxillofac Surg 50:756
Choi BH, Kim KN, Kim HJ, Kim MK (1999) Evaluation of condylar neck fracture plating techniques. J Craniomaxillofac Surg 27:109
Tominaga K, Habu M, Khanal A, Mimori Y, Yoshioka I, Fukuda J (2006) Biomechanical evaluation of different types of rigid internal fixation techniques for subcondylar fractures. J Oral Maxillofac Surg 64:1510
Wagner A, Krach W, Schicho K, Undt G, Ploder O, Ewers R (2002) A 3-dimensional finite-element analysis investigating the biomechanical behavior of the mandible and plate osteosynthesis in cases of fractures of the condylar process. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94:678
Hammer B, Schier P, Prein J (1997) Osteosynthesis of condylar neck fractures: a review of 30 patients. Br J Oral Maxillofac Surg 35:288
Choi BH, Yi CK, Yoo JH (2001) Clinical evaluation of 3 types of plate osteosynthesis for fixation of condylar neck fractures. J Oral Maxillofac Surg 59:734
Meyer C, Serhir L, Boutemi P (2006) Experimental evaluation of three osteosynthesis devices used for stabilizing condylar fractures of the mandible. J Craniomaxillofac Surg 34:173
Murakami K, Yamamoto K, Sugiura T, Horita S, Matsusue Y, Kirita T (2017) Computed tomography-based 3-dimensional finite element analyses of various types of plates placed for a virtually reduced unilateral condylar fracture of the mandible of a patient. J Oral Maxillofac Surg 75:1239 e1
Darwich MA, Albogha MH, Abdelmajeed A, Darwich K (2016) Assessment of the biomechanical performance of 5 plating techniques in fixation of mandibular subcondylar fracture using finite element analysis. J Oral Maxillofac Surg 74:794 e1
Conci RA, Tomazi FH, Noritomi PY, da Silva JV, Fritscher GG, Heitz C (2015) Comparison of neck screw and conventional fixation techniques in mandibular condyle fractures using 3-dimensional finite element analysis. J Oral Maxillofac Surg 73:1321
de Jesus GP, Vaz LG, Gabrielli MF, Passeri LA (2014) T VO, Noritomi PY, Jurgens P: Finite element evaluation of three methods of stable fixation of condyle base fractures. Int J Oral Maxillofac Surg 43:1251
Albogha MH, Mori Y, Takahashi I (2018) Three-dimensional titanium miniplates for fixation of subcondylar mandibular fractures: comparison of five designs using patient-specific finite element analysis. J Craniomaxillofac Surg 46:391
Liokatis P, Tzortzinis G, Gerasimidis S, Smolka W (2022) Finite element analysis of different titanium miniplates: evaluation of three-dimensional designs applied on condylar neck fractures. J Stomatol Oral Maxillofac Surg 123:184
Ergezen E, Akdeniz SS (2020) Evaluation of stress distribution of four different fixation systems at high- and low-level subcondylar fractures on a nonhomogenous finite element model. J Oral Maxillofac Surg 78:1596 e1
Dutta A, Mukherjee K, Dhara S, Gupta S (2019) Design of porous titanium scaffold for complete mandibular reconstruction: the influence of pore architecture parameters. Comput Biol Med 108:31
Dutta A, Mukherjee K, Seesala VS, Dutta K, Paul RR, Dhara S, Gupta S (2020) Load transfer across a mandible during a mastication cycle: the effects of odontogenic tumour. Proc Inst Mech Eng H 234:486
Ichim I, Swain MV, Kieser JA (2006) Mandibular stiffness in humans: numerical predictions. J Biomech 39:1903
MehariAbraha H, Iriarte-Diaz J, Ross CF, Taylor AB, Panagiotopoulou O (2019) The mechanical effect of the periodontal ligament on bone strain regimes in a validated finite element model of a macaque mandible. Front Bioeng Biotechnol 7:269
Korioth TW, Romilly DP, Hannam AG (1992) Three-dimensional finite element stress analysis of the dentate human mandible. Am J Phys Anthropol 88:69
Polgar K, Viceconti M, O’Connor JJ (2001) A comparison between automatically generated linear and parabolic tetrahedra when used to mesh a human femur. Proc Inst Mech Eng H 215:85
Mukherjee K, Gupta S (2017) Mechanobiological simulations of peri-acetabular bone ingrowth: a comparative analysis of cell-phenotype specific and phenomenological algorithms. Med Biol Eng Comput 55:449
Mukherjee K, Gupta S (2016) The effects of musculoskeletal loading regimes on numerical evaluations of acetabular component. Proc Inst Mech Eng H 230:918
Mukherjee K, Gupta S (2016) Bone ingrowth around porous-coated acetabular implant: a three-dimensional finite element study using mechanoregulatory algorithm. Biomech Model Mechanobiol 15:389
Dalstra M, Huiskes R, Odgaard A, van Erning L (1993) Mechanical and textural properties of pelvic trabecular bone. J Biomech 26:523
Mukherjee K, Gupta S (2017) Combined bone ingrowth and remodeling around uncemented acetabular component: a multiscale mechanobiology-based finite element analysis. J Biomech Eng 139(9):091007
Reina JM, Garcia-Aznar JM, Dominguez J, Doblare M (2007) Numerical estimation of bone density and elastic constants distribution in a human mandible. J Biomech 40:828
Manns A, Dias G (1988) Sistema estomatognático. Facultad de Odontología, Universidad de Chile, Santiago
Shockey JS, von Fraunhofer JA, Seligson D (1985) A measurement of the coefficient of static friction of human long bones. Surface Technol 25:167
O’Connor CF, Franciscus RG, Holton NE (2005) Bite force production capability and efficiency in Neandertals and modern humans. Am J Phys Anthropol 127:129
Glatt V, Evans CH, Tetsworth K (2017) A concert between biology and biomechanics: the influence of the mechanical environment on bone healing. Front Physiol 7:678
Niinomi M (1998) Mechanical properties of biomedical titanium alloys. Mater Sci Eng, A 243:231
Ji B, Wang C, Song F, Chen M, Wang H (2012) A new biomechanical model for evaluation of fixation systems of maxillofacial fractures. J Craniomaxillofac Surg 40:405
Hjorth T, Melsen B, Moller E (1997) Masticatory muscle function after unilateral condylar fractures: a prospective and quantitative electromyographic study. Eur J Oral Sci 105:298
Perren SM (1979) Physical and biological aspects of fracture healing with special reference to internal fixation. Clin Orthop Relat Res 175
Soballe K (1993) Hydroxyapatite ceramic coating for bone implant fixation. Mechanical and histological studies in dogs. Acta Orthop Scand Suppl 255:1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gupta, A., Dutta, A., Dutta, K. et al. Biomechanical influence of plate configurations on mandible subcondylar fracture fixation: a finite element study. Med Biol Eng Comput 61, 2581–2591 (2023). https://doi.org/10.1007/s11517-023-02854-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-023-02854-7