Abstract
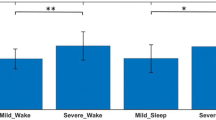
The upper airway (UA) is in general thicker and narrower in obstructive sleep apnea (OSA) population than in normal. Additionally, the UA changes during sleep are much more in the OSA population. The UA changes can alter the tracheal breathing sound (TBS) characteristics. Therefore, we hypothesize the TBS changes from wakefulness to sleep are significantly correlated to the OSA severity; thus, they may represent the physiological characteristics of the UA. To investigate our hypothesis, we recorded TBS of 18 mild-OSA (AHI < 15) and 22 moderate/severe-OSA (AHI > 15) during daytime (wakefulness) and then during sleep. The power spectral density (PSD) of the TBS was calculated and compared within the two OSA groups and between wakefulness and sleep. The average PSD of the mild-OSA group in the low-frequency range (< 280 Hz) was found to be decreased significantly from wakefulness to sleep (p-value < 10−4). On the other hand, the average PSD of the moderate/severe-OSA group in the high-frequency range (> 900 Hz) increased marginally significantly from wakefulness to sleep (p-value < 9 × 10−3). Our findings show that the changes in spectral characteristics of TBS from wakefulness to sleep correlate with the severity of OSA and can represent physiological variations of UA. Therefore, TBS analysis has the potentials to assist with diagnosis and clinical management decisions in OSA patients based on their OSA severity stratification; thus, obviating the need for more expensive and time-consuming sleep studies.

Tracheal breathing sound (TBS) changes from wakefulness to sleep and their correlation with Obstructive sleep apnea (OSA) were investigated in individuals with different levels of OSA severity. We also assessed the classification power of the spectral characteristics of these TBS for screening purposes. Consequently, we analyzed and compared spectral characteristics of TBS recorded during wakefulness (a combination of mouth and nasal TBS) to those during sleep for mild and moderate/severe OSA groups.



Similar content being viewed by others
Abbreviations
- AHI:
-
Apnea/hypopnea index
- ANOVA:
-
analysis of variance
- BMI:
-
Body mass index
- HSS:
-
Home sleep study
- MRI:
-
Magnetic resonance imaging
- NC:
-
Neck circumference
- OSA:
-
Obstructive sleep apnea
- PSD:
-
Power spectrum density
- PSDavg :
-
Average power spectrum density
- PSG:
-
Polysomnography
- SE:
-
Standard error
- SVM:
-
Support vector machine
- TBS:
-
Tracheal breathing sounds
- UA:
-
Upper airway
References
Bilston LE, Gandevia SC (2013) Biomechanical properties of the human upper airway and their effect on its behavior during breathing and in obstructive sleep apnea. J Appl Physiol 116:314–324. https://doi.org/10.1152/japplphysiol.00539.2013
Malhotra A, White DP (2002) Obstructive sleep apnoea. Lancet 360:237–245. https://doi.org/10.1016/S0140-6736(02)09464-3
Berry RB, Brooks R, Gamaldo CE, Harding SM, et al (2018) The AASM manual for the scoring of sleep and associated events: rules, Terminology and Technical Specifications, Version 2.5
Park JG, Ramar K, Olson EJ (2011) Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc 86:549–555. https://doi.org/10.4065/mcp.2010.0810
Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, Hamilton GS, Dharmage SC (2017) Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev 34:70–81. https://doi.org/10.1016/j.smrv.2016.07.002
Memtsoudis SG, Besculides MC, Mazumdar M (2013) A rude awakening — the perioperative sleep apnea epidemic. N Engl J Med 368:2352–2353. https://doi.org/10.1056/NEJMp1302941
Young T, Palta M, Dempsey J et al (2010) Burden of sleep apnea: rationale, design, and major findings of the Wisconsin sleep cohort study. WMJ Off Publ State Med Soc Wisconsin 108:246–249
Kushida CA, Littner MR, Morgenthaler T, Alessi CA, Bailey D, Coleman J Jr, Friedman L, Hirshkowitz M, Kapen S, Kramer M, Lee-Chiong T, Loube DL, Owens J, Pancer JP, Wise M (2005) Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep 28:499–523. https://doi.org/10.1093/sleep/28.4.499
Deutsch PA, Simmons MS, Wallace JM (2006) Cost-effectiveness of split-night polysomnography and home studies in the evaluation of obstructive sleep apnea syndrome. J Clin Sleep Med 2:145–153
Priftis KN, Hadjileontiadis LJ, Everard ML (2018) Breath sounds from basic science to clinical practice. Springer International Publishing, Cham
Penzel T, Sabil A (2017) The use of tracheal sounds for the diagnosis of sleep apnoea. Breathe 13:e37–e45. https://doi.org/10.1183/20734735.008817
Ayappa I, Rapoport DM (2003) The upper airway in sleep: physiology of the pharynx. Sleep Med Rev 7:9–33. https://doi.org/10.1053/smrv.2002.0238
Lan Z, Itoi A, Takashima M, Oda M, Tomoda K (2006) Difference of pharyngeal morphology and mechanical property between OSAHS patients and normal subjects. Auris Nasus Larynx 33:433–439. https://doi.org/10.1016/j.anl.2006.03.009
Jordan AS, White DP, Lo Y et al (2009) Airway dilator muscle activity and lung volume during stable breathing in obstructive sleep apnea. Sleep 32:361–368. https://doi.org/10.1093/sleep/32.3.361
Finkelstein Y, Wolf L, Nachmani A, Lipowezky U, Rub M, Shemer S’, Berger G (2014) Velopharyngeal anatomy in patients with obstructive sleep apnea versus normal subjects. J Oral Maxillofac Surg 72:1350–1372. https://doi.org/10.1016/j.joms.2013.12.006
Schwab RJ, Pasirstein M, Pierson R, Mackley A, Hachadoorian R, Arens R, Maislin G, Pack AI (2003) Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am J Respir Crit Care Med 168:522–530. https://doi.org/10.1164/rccm.200208-866OC
Fogel RB, Trinder J, White DP, Malhotra A, Raneri J, Schory K, Kleverlaan D, Pierce RJ (2005) The effect of sleep onset on upper airway muscle activity in patients with sleep apnoea versus controls. J Physiol 564:549–562. https://doi.org/10.1113/jphysiol.2005.083659
Wu Z, Chen W, Khoo MCK, Davidson Ward SL, Nayak KS (2016) Evaluation of upper airway collapsibility using real-time MRI. J Magn Reson Imaging 44:158–167. https://doi.org/10.1002/jmri.25133
Nakano H, Furukawa T, Tanigawa T (2019) Tracheal sound analysis using a deep neural network to detect sleep apnea
Beck R, Rosenhouse G, Mahagnah M, Chow RM, Cugell DW, Gavriely N (2005) Measurements and theory of normal tracheal breath sounds. Ann Biomed Eng 33:1344–1351. https://doi.org/10.1007/s10439-005-5564-7
Kulkas A, Huupponen E, Virkkala J, Tenhunen M, Saastamoinen A, Rauhala E, Himanen SL (2009) New tracheal sound feature for apnoea analysis. Med Biol Eng Comput 47:405–412. https://doi.org/10.1007/s11517-009-0446-z
Hajipour F, Jafari Jozani M, Elwali A, Moussavi Z (2019) Regularized logistic regression for obstructive sleep apnea screening during wakefulness using daytime tracheal breathing sounds and anthropometric information. Med Biol Eng Comput 57:2641–2655. https://doi.org/10.1007/s11517-019-02052-4
Yadollahi A, Giannouli E, Moussavi Z (2010) Sleep apnea monitoring and diagnosis based on pulse oximetery and tracheal sound signals. Med Biol Eng Comput 48:1087–1097. https://doi.org/10.1007/s11517-010-0674-2
Younes M (2008) Role of respiratory control mechanisms in the pathogenesis of obstructive sleep disorders. J Appl Physiol 105:1389–1405. https://doi.org/10.1152/japplphysiol.90408.2008
Ryan CM, Bradley TD (2005) Pathogenesis of obstructive sleep apnea. J Appl Physiol 99:2440–2450
Rama AN, Tekwani SH, Kushida CA (2002) Sites of obstruction in obstructive sleep apnea. Chest 122:1139–1147. https://doi.org/10.1378/chest.122.4.1139
Hajipour F, Moussavi Z (2019) Spectral and higher order statistical characteristics of expiratory tracheal breathing sounds during wakefulness and sleep in people with different levels of obstructive sleep apnea. J Med Biol Eng 39:244–250. https://doi.org/10.1007/s40846-018-0409-7
Huq S, Moussavi Z (2012) Acoustic breath-phase detection using tracheal breath sounds. Med Biol Eng Comput 50:297–308. https://doi.org/10.1007/s11517-012-0869-9
Arvin F, Doraisamy S, Safar Khorasani E (2011) Frequency shifting approach towards textual transcription of heartbeat sounds. Biol Proced Online 13:1–7. https://doi.org/10.1186/1480-9222-13-7
Yadollahi A, Moussavi ZMK (2007) Acoustical flow estimation: review and validation. IEEE Eng Med Biol Mag 26:56–61. https://doi.org/10.1109/MEMB.2007.289122
Elwali A, Moussavi Z (2017) Obstructive sleep apnea screening and airway structure characterization during wakefulness using tracheal breathing sounds. Ann Biomed Eng 45:839–850. https://doi.org/10.1007/s10439-016-1720-5
Simes RJ (1986) An improved Bonferroni procedure for multiple tests of significance. Biometrika 73:751–754. https://doi.org/10.1093/biomet/73.3.751
Kalkbrenner C, Eichenlaub M, Rüdiger S, Kropf-Sanchen C, Rottbauer W, Brucher R (2018) Apnea and heart rate detection from tracheal body sounds for the diagnosis of sleep-related breathing disorders. Med Biol Eng Comput 56:671–681. https://doi.org/10.1007/s11517-017-1706-y
Kulkas A, Rauhala E, Huupponen E, Virkkala J, Tenhunen M, Saastamoinen A, Himanen SL (2008) Detection of compressed tracheal sound patterns with large amplitude variation during sleep. Med Biol Eng Comput 46:315–321. https://doi.org/10.1007/s11517-008-0317-z
Harper P, Kraman SS, Pasterkamp H, Wodicka GR (2001) An acoustic model of the respiratory tract. IEEE Trans Biomed Eng 48:543–550. https://doi.org/10.1109/10.918593
Seddeq HS (2009) Factors influencing acoustic performance of sound absorptive materials. Aust J Basic Appl Sci 3:4610–4617
Veldi, Vasar, Vain et al (2000) Computerized endopharyngeal myotonometry (CEM): a new method to evaluate the tissue tone of the soft palate in patients with obstructive sleep apnoea syndrome. J Sleep Res 9:279–284. https://doi.org/10.1046/j.1365-2869.2000.00208.x
Jensen OE (2002) Flows through deformable airways. In: Centre for Mathematical Medicine School of Mathematical Sciences University of Nottingham, UK. pp 27217–222
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hajipour, F., Giannouli, E. & Moussavi, Z. Acoustic characterization of upper airway variations from wakefulness to sleep with respect to obstructive sleep apnea. Med Biol Eng Comput 58, 2375–2385 (2020). https://doi.org/10.1007/s11517-020-02234-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-020-02234-5