Abstract
The modeling of breast deformations is of interest in medical applications such as image-guided biopsy, or image registration for diagnostic purposes. In order to have such information, it is needed to extract the mechanical properties of the tissues. In this work, we propose an iterative technique based on finite element analysis that estimates the elastic modulus of realistic breast phantoms, starting from MRI images acquired in different positions (prone and supine), when deformed only by the gravity force. We validated the method using both a single-modality evaluation in which we simulated the effect of the gravity force to generate four different configurations (prone, supine, lateral, and vertical) and a multi-modality evaluation in which we simulated a series of changes in orientation (prone to supine). Validation is performed, respectively, on surface points and lesions using as ground-truth data from MRI images, and on target lesions inside the breast phantom compared with the actual target segmented from the US image. The use of pre-operative images is limited at the moment to diagnostic purposes. By using our method we can compute patient-specific mechanical properties that allow compensating deformations.

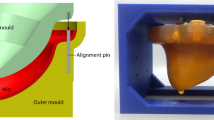
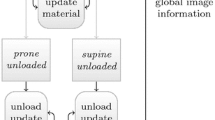
Workflow of the proposed method and comparative results of the prone-to-supine simulation (red volumes) validated using MRI data (blue volumes)









Similar content being viewed by others
References
Sree SV, Ng E Y-K, Acharya RU, Faust O (2011) Breast imaging: a survey. World J Clin Oncol 04(4):171–178
Samani A, Plewes D (2007) An inverse problem solution for measuring the elastic modulus of intact ex vivo breast tissue tumours. Phys Med Biol 52(5):1247
Gefen A, Dilmoney B (2007) Mechanics of the normal woman’s breast. Technol Health Care 15(4):259–271
Parker KJ, Doyley MM, Rubens DJ (2010) Imaging the elastic properties of tissue: the 20 year perspective. Phys Med Biol 56(1):R1
Sarvazyan A, Hall TJ, Urban MW, Fatemi M, Aglyamov SR, Garra BS (2011) An overview of elastography-an emerging branch of medical imaging. Curr Med Imaging Rev 7(4):255–282
Doyley MM (2012) Model-based elastography: a survey of approaches to the inverse elasticity problem. Phys Med Biol 57(3):R35
Han L, Hipwell JH, Tanner C, Taylor Z, Mertzanidou T, Cardoso J, Ourselin S, Hawkes DJ (2011) Development of patient-specific biomechanical models for predicting large breast deformation. Phys Med Biol 57(2):455
Han L, Hipwell J H, Eiben B, Barratt D, Modat M, Ourselin S, Hawkes D J (2014) A nonlinear biomechanical model based registration method for aligning prone and supine mr breast images. IEEE Trans Med Imaging 33(3):682–694
Eiben B, Han L, Hipwell J, Mertzanidou T, Kabus S, Bülow T, Lorenz C, Newstead GM, Abe H, Keshtgar M (2013) Biomechanically guided prone-to-supine image registration of breast mri using an estimated reference state. In: 2013 IEEE 10th international symposium on biomedical imaging (ISBI). IEEE, pp 214–217
Eiben B, Vavourakis V, Hipwell JH, Kabus S, Lorenz C, Buelow T, Hawkes DJ (2014) Breast deformation modelling: comparison of methods to obtain a patient specific unloaded configuration, vol 9036, pp 903615–8
Conley RH, Meszoely IM, Weis JA, Pheiffer TS, Arlinghaus LR, Yankeelov TE, Miga MI (2015) Realization of a biomechanical model-assisted image guidance system for breast cancer surgery using supine mri. Int J Comput Assist Radiol Surg 10(12):1985–1996
Lee A, Schnabel J, Rajagopal V, Nielsen P, Nash M (2010) Breast image registration by combining finite elements and free-form deformations. In: Digital mammography, pp 736–743
Carter T, Tanner C, Beechey-Newman N, Barratt D, Hawkes D (2008) Mr navigated breast surgery: method and initial clinical experience. In: Medical image computing and computer-assisted intervention–MICCAI, vol 2008, pp 356–363
Han L, Hipwell J, Mertzanidou T, Carter T, Modat M, Ourselin S, Hawkes D (2011) A hybrid fem-based method for aligning prone and supine images for image guided breast surgery. In: 2011 IEEE international symposium on biomedical imaging: from Nano to Macro. IEEE, pp 1239–1242
Pathmanathan P, Gavaghan DJ, Whiteley JP, Chapman SJ, Brady JM (2008) Predicting tumor location by modeling the deformation of the breast. IEEE Trans Biomed Eng 55(10):2471– 2480
Patete P, Iacono MI, Spadea MF, Trecate G, Vergnaghi D, Mainardi LT, Baroni G (2013) A multi-tissue mass-spring model for computer assisted breast surgery. Med Eng Phys 35(1):47–53
Zerbato D, Baschirotto D, Baschirotto D, Botturi D, Fiorini P (2011) Gpu-based physical cut in interactive haptic simulations. Int J Comput Assist Radiol Surg 6(2):265–272
Pinto Pereira SM, Hipwell JH, McCormack VA, Tanner C, Moss SM, Wilkinson LS, Khoo LAL, Pagliari C, Skippage PL, Kliger CJ (2010) Automated registration of diagnostic to prediagnostic x-ray mammograms: evaluation and comparison to radiologists’ accuracy. Med Phys 37(9):4530–4539
van Engeland S, Snoeren P, Hendriks JHCL, Karssemeijer N (2003) A comparison of methods for mammogram registration. IEEE Trans Med Imaging 22(11):1436–1444
Lautrup B (2011) Physics of continuous matter, 2nd edn: exotic and everyday phenomena in the macroscopic world. CRC Press, Boca Raton
Maas SA, Ellis BJ, Ateshian GA, Weiss JA (2012) Febio: finite elements for biomechanics. J Biomech Eng 134(1):011005
Besl PJ, McKay ND (1992) A method for registration of 3-d shapes. IEEE Trans Pattern Anal Mach Intell 14(2):239–256
Rankin A, Pinter C, Ungi T, Lasso A, Heffter T, Fichtinger G (2014) Plus: open-source toolkit for ultrasound-guided intervention systems. In: IEEE transactions on biomedical engineering
Zerbato D, Forgione A, Fiorini P (2016) University of Verona Santorzo Vicenza D. Dall’Alba, F. Bovo. Towards an intra-operative calibration-preserving freehand ultrasound system. In: Computer Assisted Radiology and Surgery (CARS)
Funding
This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement no.688188 as part of the MURAB project.
Author information
Authors and Affiliations
Corresponding author
Additional information
F. Visentin and V. Groenhuis contributed equally to the paper.
Rights and permissions
About this article
Cite this article
Visentin, F., Groenhuis, V., Maris, B. et al. Iterative simulations to estimate the elastic properties from a series of MRI images followed by MRI-US validation. Med Biol Eng Comput 57, 913–924 (2019). https://doi.org/10.1007/s11517-018-1931-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-018-1931-z