Abstract
Mothers of children with autism spectrum disorders (ASD) typically report lower overall family functioning and worse mental health. Neighborhood conditions are found to positively influence family functioning and mental health in the general population. Employing a process-person-context model, this study extends these literatures to examine whether various neighborhood conditions – both positive and negative – affect mothers’ mental health and the overall functioning of families with a child with an ASD. Simultaneous equation path analysis of a nationally representative sample of children in the US finds neighborhood support to be positively and significantly associated with mothers’ mental health and the overall functioning of families with a child with an ASD. However, neighborhood amenities and neighborhood deficiencies were not significantly associated with either mothers’ mental health or family functioning. Neighborhood support can play a vital role in improved subjective quality of life for mothers with a child on the autism spectrum.

Similar content being viewed by others
Notes
The lower response rate for the 2011/2012 wave of the NSCH was primarily due to the inclusion of cell-phone interviews which “provided better coverage of the population of children at the expense of lower response rates” (Blumberg et al. 2013:10). The lower response rates for the cell-phone interviews were due to higher non-resolution rates for those interviews. Also, there is a higher risk of uncorrected coverage bias in the 2007 NSCH due to the lack of use of cell phones when collecting that sample. See Blumberg et al. 2013 for more information on response rates and analysis of nonresponse for the 2011/2012 NSCH.
It is important to note that the NSCH relies on the parent/guardian reporting whether their child has ever been diagnosed with an autism spectrum disorder. It does not verify each child’s diagnosis with medical professionals. As will be discussed later, the rates of the disorders found in the 2007 and 2011/2012 waves of the NSCH using parental reporting of diagnoses are found to be reliable compared to studies that utilize clinical validation (Kogan et al. 2009).
Concerning ASD specifically, diagnosis at age 2 or later is shown to be reliable, valid, and stable (Lord et al. 2006). Furthermore, research shows parents of children with ASD notice a developmental problem before the child’s first birthday, with some differences in communication, social, and fine motor skills evident at 6 months (Bolton et al. 2012; Kozlowski et al. 2011). By limiting the sample to those children aged 2 to 17, the NSCH increases the probability that parents have noticed signs of ASD and sought out professional help.
It is important to note that both waves of the National Survey of Children’s Health (NSCH) utilize a complex sampling design. Creating subsamples using listwise deletion for surveys that employ a complex sampling design can be problematic and thus subpopulation analysis is generally discouraged. However, as Bell et al. (2009) show, there is little to no difference in the standard errors generated using listwise deletion and subpopulation techniques on surveys with complex sampling designs. They conclude that it is reasonable to perform analyses on subgroups created using listwise deletion on a survey that utilized a complex sampling design.
Ancillary analyses demonstrate that there are statistically significant differences in the ratings of the mother’s mental and emotional health depending on whether the mother answered about herself or a father or other relative answered about the mother. Respondents who were not the mother consistently rated the mother as having a higher mental and emotional health than mothers rated themselves. Results available upon request.
The score for mental/emotional health for mothers with a child with an ASD is 10 % lower than mothers who do not have a child with an ASD (3.58/3.99 = 0.897; 1–0.897 = 0.103; 0.103 × 100 = 10.3 %).
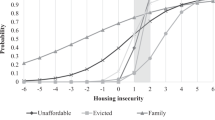
Families of children with an ASD report a score of −3.02; families without a child with an ASD report a score of −0.04. The mean value for family functioning in the overall sample is 0 and ranges from −15 to 4. See the Data section for more on this particular measure.
The perceived neighborhood support scores for mothers of children with an ASD are 18 % lower than for mothers without a child with an ASD (1.99/2.43 = 0.819; .1–.0819 = 0.181; 0.181 × 100 = 18.1 %).
Zhao et al. (2010) provide a corrective to Baron and Kenny (1986) much-cited procedure for establishing mediation. In their decision tree for establishing and understanding types of mediation and nonmediation, complementary mediation exists when a significant indirect effect (X → M → Y) and a significant direct effect (X → Y) are both present and are of the same sign. Zhao and colleagues argue that the persistence of a direct effect signals the possibility of an omitted mediator which serves to further the advancement of the theoretical framework. I return to this in the discussion section below.
Following Zhao et al. (2010), the relationship between neighborhood threats and neighborhood resources, family functioning, and mothers’ mental and emotional health can be classified as no-effect non mediation. The implications of this finding are discussed further in the discussion section below.
References
Asparouhov, T., & Muthén, B. (2010). Weighted least squares estimation with missing data. MplusTechnical Appendix.
Baron, R. M., & Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182.
Bayat, M. (2007). Evidence of resilience in families of children with autism. Journal of Intellectual Disability Research, 51, 9, 702–714.
Bell, Bethany A., Jeffrey D. Kromrey, and John M. Ferron. (2009). Missing data and complex samples: The impact of listwise deletion vs. subpopulation analysis on statistical bias and hypothesis test results when data are MCAR and MAR. In Proceedings of the Joint Statistical Meetings, Survey Research Methods Section, 2009.
Benjak, T., Vuletić, G., & Kolarić, B. (2011). Subjective quality of life for parents of children with autism spectrum disorders in Croatia. Applied Research in Quality of Life, 6, 91–102.
Bishop, S. L., Richler, J., Cain, A. C., Lord, C., & Floyd, F. (2007). Predictors of perceived negative impact in mothers of children with autism spectrum disorder. American Journal on Mental Retardation, 112(6), 450–461.
Blanchflower, D. G., & Oswald, A. J. (2008). Is well-being U-shaped over the life cycle? Social Science & Medicine, 66(8), 1733–1749.
Blumberg, S. J., Foster, E. B., Frasier, A. M., Satorius, J., Skalland, B. J., Nysse-Carris, K. L., et al. (2012). Design and operation of the national survey of children's health. 2007 Vital and Health Statistics.Ser.1. Programs and Collection Procedures, 55, 1–149.
Blumberg, S. J., Bramlett, M. D., Kogan, M. D., Schieve, L. A., Jones, J. R., & Lu, M. C. (2013). Changes in prevalence of parent-reported autism spectrum disorder in school-aged US children: 2007 to 2011–2012. National Health Statistics Reports, 65(20), 1–7.
Bolton, P. F., Golding, J., Emond, A., & Steer, C. D. (2012). Autism spectrum disorder and autistic traits in the Avon longitudinal study of parents and children: Precursors and early signs. Journal of the American Academy of Child and Adolescent Psychiatry, 51, 249–260 e25.
Bowling, A. (2005). Just one question: if one question works, why ask several? Journal of Epidemiology and Community Health, 59, 5, 342–345.
Boyd, B. A. (2002). Examining the relationship between stress and lack of social support in mothers of children with autism. Focus on Autism and Other Developmental Disabilities, 17, 4, 208–215.
Bromley, J., Hare, D. J., Davison, K., & Emerson, E. (2004). Mothers supporting children with autistic spectrum disorders: Social support, mental health status and satisfaction with services. Autism: The International Journal of Research and Practice, 8(4), 409–423.
Bronfenbrenner, U. (1977). Toward an experimental ecology of human development. American Psychologist, 32, 515–531.
Bronfenbrenner, U. (1986). Ecology of the family as a context for human development: research perspectives. Developmental Psychology, 22(6), 723–742.
Bronfenbrenner, U. (1994). Ecological models of human development. In T. Husten & T.N. Postlethewaite (Eds.), International Encyclopedia of Education (2nd Ed., Vol. 3) pp. 1643–1657, NY: Freeman.
Bronfenbrenner, U. (1999). Environments in developmental perspective: Theoretical and operational models. In S. L. Friedman & T. D. Wachs (Eds.), Measuring environment across the life span: Emerging methods and concepts (pp. 3–28). Washington, DC: American Psychological Press.
Cattell, V. (2001). Poor people, poor places, and poor health: The mediating role of social networks and social capital. Social Science & Medicine, 52(10), 1501–1516.
Centers for Disease Control and Prevention (CDC). (2014). Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, D.C.: 2002), 63(2), 1–21.
Chiri, G., & Warfield, M. E. (2012). Unmet need and problems accessing core health care services for children with autism spectrum disorder. Maternal and Child Health Journal, 16(5), 1081–1091.
Chu, A., Thorne, A., & Guite, H. (2004). The impact on mental well-being of the urban and physical environment: An assessment of the evidence. Journal of Public Mental Health, 3(2), 17–32.
Coulthard, P., & Fitzgerald, M. (1999). In god we trust? Organized religion and personal beliefs as resources and coping strategies, and their implications for health in parents with a child on the autistic spectrum. Mental Health, Religion & Culture, 2, 1, 19.
Dabrowska, A., & Pisula, E. (2010). Parenting stress and coping styles in mothers and fathers of pre-school children with autism and Down syndrome. Journal of Intellectual Disability Research, 54, 266–280.
Ekas, N. V., Whitman, T. L., & Shivers, C. (2009). Religiosity, spirituality, and socioemotional functioning in mothers of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 39(5), 706–719.
Ekas, N. V., Lickenbrock, D. M., & Whitman, T. L. (2010). Optimism, social support, and well-being in mothers of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 40(10), 1274–1284.
Ellen, I. G., Mijanovich, T., & Dillman, K. (2001). Neighborhood effects on health: Exploring the links and assessing the evidence. Journal of Urban Affairs, 23(3–4), 391–408.
Fan, Y., & Chen, Q. (2012). Family functioning as a mediator between neighborhood conditions and children's health: Evidence from a national survey in the United States. Social Science & Medicine, 74(12), 1939–1947.
Farrugia, D. (2009). Exploring stigma: Medical knowledge and the stigmatisation of parents of children diagnosed with autism spectrum disorder. Sociology of Health & Illness, 31(7), 1011–1027.
Francis, A. (2012). The dynamics of family trouble: middle-class parents whose children have problems. Journal of Contemporary Ethnography, 41(4), 371–401.
Gale, C. R., Dennison, E. M., Cooper, C., & Sayer, A. A. (2011). Neighbourhood environment and positive mental health in older people: The Hertfordshire cohort study. Health & Place, 17(4), 867–874.
Gonzalez, M. C., Hidalgo, C. A., & Barabasi, A. (2008). Understanding individual human mobility patterns. Nature, 453(7196), 779–782.
Gray, D. E. (1997). High functioning autistic children and the construction of “normal family life”. Social Science & Medicine, 44(8), 1097–1106.
Gray, D. E. (2001). Accommodation, resistance and transcendence: Three narratives of autism. Social Science & Medicine, 53(9), 1247–1257.
Gray, D. E. (2002). ‘Everybody just freezes. Everybody is just embarrassed’: Felt and enacted stigma among parents of children with high functioning autism. Sociology of Health & Illness, 24(6), 734–749.
Gray, D. E. (2003). Gender and coping: The parents of children with high functioning autism. Social Science & Medicine, 56(3), 631–642.
Gray, D. E. (2006). Coping over time: the parents of children with autism. Journal of Intellectual Disability Research, 50, 12, 970–976.
Guite, H., Clark, C., & Ackrill, G. (2006). The impact of the physical and urban environment on mental well-being. Public Health, 120(12), 1117–1126.
Hastings, R. P. (2003). Child behaviour problems and partner mental health as correlates of stress in mothers and fathers of children with autism. Journal of Intellectual Disability Research, 47, 4–5, 231–237.
Hastings, R. P. (2008). Stress in parents of children with autism. In E. McGregor, M. Nunez, D. Cebula, & J. C. Gomez (Eds.), Autism: An integrated view from neuroscience, clinical, and intervention research (pp. 303–324). London: Blackwell.
Hastings, R. P., Kovshoff, H., Brown, T., Ward, N. J., Espinosa, F. D., & Remington, B. (2005). Coping strategies in mothers and fathers of preschool and school-age children with autism. Autism: The International Journal of Research and Practice, 9(4), 377–391.
Hayes, S. A., & Watson, S. L. (2013). The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders, 43(3), 629–642.
Jones, L., Totsika, V., Hastings, R. P., & Petalas, M. A. (2013). Gender differences when parenting children with autism spectrum disorders: A multilevel modeling approach. Journal of Autism and Developmental Disorders, 43(9), 2090–2098.
Jones, R., Heim, D., Hunter, S., & Ellaway, A. (2014). The relative influence of neighbourhood incivilities, cognitive social capital, club membership and individual characteristics on positive mental health. Health & Place, 28, 187–193.
Jöreskog, K. G. (1993). Testing structural equation models. In K.A. Bollen & J. Scott Long (eds.), Testing Structural Equation Models (pp. 294–316). Sage Publications, Inc: Newbury Park, CA.
Khanna, R., Madhavan, S. S., Smith, M. J., Patrick, J. H., Tworek, C., & Becker-Cottrill, B. (2011). Assessment of health-related quality of life among primary caregivers of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 41(9), 1214–1227.
Kogan, M. D., Strickland, B. B., Blumberg, S. J., Singh, G. K., Perrin, J. M., & van Dyck, P. C. (2008). A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005–2006. Pediatrics, 122(6), e1149–e1158.
Kogan, M. D., Blumberg, S. J., Schieve, L. A., Boyle, C. A., Perrin, J. M., Ghandour, R. M., et al. (2009). Prevalence of parent-reported diagnosis of autism spectrum disorder among children in the US, 2007. Pediatrics, 124(5), 1395–1403.
Kozlowski, A. M., Matson, J. L., Horovitz, M., Worley, J. A., & Neal, D. (2011). Parents' first concerns of their child's development in toddlers with autism spectrum disorders. Developmental Neurorehabilitation, 14(2), 72–78.
Lai, W. W., & Oei, T. P. S. (2014). Coping in parents and caregivers of children with autism spectrum disorders (ASD): A review. Review Journal of Autism and Developmental Disorders, 207–224.
Liu, K. Y., King, M., & Bearman, P. S. (2010). Social influence and the autism epidemic. American Journal of Sociology, 115(5), 1387–1434.
Lord, C., Risi, S., DiLavore, P. S., Shulman, C., Thurm, A., & Pickles, A. (2006). Autism from 2 to 9 years of age. Archives of General Psychiatry, 63(6), 694–701.
Mannon, S. E., & Brooks, W. T. (2006). Neighborhood family-friendliness and its effect on family relations: Evidence from Utah. Sociological Spectrum, 26(4), 405–421.
Miller, J. E., Nugent, C. N., & Russell, L. B. (2015). Risk factors for family time burdens arranging and providing health care for children with special health care needs: Lessons from nonproportional odds models. Social Science Research DOI. doi:10.1016/j.ssresearch.2015.04.003.
Muthén, L. K., & Muthén, B. O. (1998-2012). Mplus: Statistical analysis with latent variables: User's guide. Los Angeles, CA: Muthén & Muthén.
Nunnally, J. C. (1978). Psychometric Theory, 2nd edition. New York. NY: McGraw-Hill.
Park, J., Turnbull, A. P., & Turnbull, H. R. (2002). Impacts of poverty on quality of life in families of children with disabilities. Exceptional Children, 68(2), 151–170.
Parner, E. T., Schendel, D. E., & Thorsen, P. (2008). Autism prevalence trends over time in Denmark: Changes in prevalence and age at diagnosis. Archives of Pediatrics & Adolescent Medicine, 162(12), 1150–1156.
Sawyer, M. G., Bittman, M., La Greca, A. M., Crettenden, A. D., Harchak, T. F., & Martin, J. (2010). Time demands of caring for children with autism: What are the implications for maternal mental health? Journal of Autism and Developmental Disorders, 40(5), 620–628.
Sayer, L. C. (2005). Gender, time and inequality: Trends in women’s and men’s paid work, unpaid work and free time. Social Forces, 84(1), 285–303.
Schieve, L. A., Rice, C., Yeargin-Allsopp, M., Boyle, C. A., Kogan, M. D., Drews, C., & Devine, O. (2012). Parent-reported prevalence of autism spectrum disorders in US-born children: An assessment of changes within birth cohorts from the 2003 to the 2007 national survey of Children’s health. Maternal and Child Health Journal, 16(1), 151–157.
Sikora, D., Moran, E., Orlich, F., Hall, T. A., Kovacs, E. A., Delahaye, J., et al. (2013). The relationship between family functioning and behavior problems in children with autism spectrum disorders. Research in Autism Spectrum Disorders, 7, 2, 307–315.
South, S. J. (2001). The geographic context of divorce: do neighborhoods matter? Journal of Marriage and Family, 63, 3, 755–766.
South, S. J., & Crowder, K. D. (1999). Neighborhood effects on family formation: Concentrated poverty and beyond. American Sociological Review, 64(1), 113–132.
South, S. J., & Lloyd, K. M. (1995). Spousal alternatives and marital dissolution. American Sociological Review, 60(1), 21–35.
Tarakeshwar, N., & Pargament, K. I. (2001). Religious coping in families of children with autism. Focus on Autism and Other Developmental Disabilities, 16(4), 247–260.
Trent, K., & South, S. J. (2003). Spousal alternatives and marital relations. Journal of Family Issues, 24(6), 787–810.
Truong, K. D., & Ma, S. (2006). A systematic review of relations between neighborhoods and mental health. The Journal of Mental Health Policy and Economics, 9(3), 137–154.
Zablotsky, B., Bradshaw, C. P., & Stuart, E. A. (2013). The association between mental health, stress, and coping supports in mothers of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 43(6), 1380–1393.
Zablotsky, B., Bramlett, M., & Blumberg, S. J. (2015). Factors associated with parental ratings of condition severity for children with autism spectrum disorder. Disability and Health Journal 8(4), 626–34.
Zhao, X., Lynch Jr., J. G., & Qimei, C. (2010). Reconsidering Baron and Kenny: Myths and Truths about Mediation Analysis. Journal of Consumer Research, 37, 197–206.
Acknowledgments
The author would like to thank the editor and the anonymous reviewers for their constructive feedback on an earlier version of this manuscript. Any errors or omissions remain the author’s alone. Special thanks as well to Kelly, Joel, and Theodore Whitehead for embodying hope and strength in the face of countless obstacles.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Whitehead, A.L. Neighborhoods, Family Functioning, and Mothers’ Mental Health for Families with a Child with an Autism Spectrum Disorder. Applied Research Quality Life 12, 633–651 (2017). https://doi.org/10.1007/s11482-016-9480-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11482-016-9480-9