Abstract
Substance use disorder treatment faces challenges such as dropout, relapse, and readmission. This study aims to identify factors associated with readmission and those influencing dropout among dual diagnosis (DD) patients (those with both a substance use disorder and another psychiatric disorder) attending outpatient addiction centers. Retrospective cohort study using the electronic health records of 8383 outpatients diagnosed with DD. Bivariate analysis and regression analysis were applied to control for the variables. Age, incarceration for 30 days prior to admission, and specific patterns of consumption increased the likelihood of readmission. Specifically, individuals who reported no substance use in the 30 days before admission or those diagnosed with an opioid or cocaine use disorder were particularly susceptible to readmission. Of the dual diagnoses, patients with personality disorders were more likely to be readmitted. In relation to dropout, opioid dependence and frequency of use were associated with a higher probability of dropout. Patients with poorer adherence to treatment and previous readmissions were also more likely to drop out. Enhancing treatment adherence and reducing dropout and readmission rates poses a challenge in managing patients with DD. Leveraging electronic health records offers enhanced ecological validity concerning the outpatient treatment requirements for such patients. Therapeutic adherence, alongside specific sociodemographic variables and consumption patterns, emerges as pivotal factors in this context. Identifying and understanding these variables facilitates the customization of outpatient treatment strategies to better meet the needs of patients with comorbidities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Dropout (Krawczyk et al., 2017), relapse to drug use (Ambrosio-Flores & Alguacil-Merino, 2023), and readmission to treatment (Lorine et al., 2015; Ramadan et al., 2022) present challenges for managing substance use disorders (SUDs). In epidemiology, “dropout” and “relapse” are related terms with different clinical connotations. Dropout refers to abandoning the treatment being undertaken (Melville et al., 2010), while relapse can be defined as returning to drug use after a period of abstinence (Department of Health, 2004). Readmission involves the initiation of a new treatment. Patients who are readmitted to treatment may do so after a period of successful treatment or after abandoning previous treatment, with the latter being more common (Dacosta-Sánchez et al., 2023). In either case, these patients perceive a clinical deterioration resulting from their addiction, which prompts them to seek additional professional support beyond what they received after their initial treatment. According to a systematic review conducted by Brorson et al. (2013), outpatient addiction treatment centers were found to have dropout rates ranging from 23 to 50%. It has been noted that these dropout rates tend to increase among patients with both a mental health disorder and a substance use disorder, commonly referred to as dual diagnosis (DD) or dual pathology. A reported prevalence of 60% in the first month (Pennay et al., 2011) and 80% in the first year of treatment (Dixon et al., 2016) has been documented. Reports from the European Monitoring Center for Drugs and Drug Addiction (EMCDDA, 2023) and the Substance Abuse and Mental Health Services Administration (SAMHSA, 2022) have shown that more than 50% of treatment admissions are for patients who have received previous treatment. As a consequence of patient dropout, relapse, and readmission to treatment, administrative, legal, and healthcare costs increase. Furthermore, they have the potential to significantly impact the quality of life for those affected (Blackwood et al., 2021; Wade et al., 2006).
Extensive research has been conducted on several variables that may affect the likelihood of readmission (Durbin et al., 2007). However, the findings show a lack of consistency in their influence. While some studies suggest certain variables can lower the probability of readmission, others indicate an increase. Additionally, other variables are suggested to have no significant influence on future readmission. For example, concerning sociodemographic variables, among the variables that produce inconclusive results are age (Becker & Shafer, 2007; Geniş et al., 2020; Kim et al., 2011; Smith et al., 2015) and gender (Hutchison et al., 2019; McHugh et al., 2018; Smith et al., 2015). Nevertheless, readmission rates tend to be higher for individuals residing in urban areas (Ghosh et al., 2022; Hutchison et al., 2019) and those with physical disabilities or medical conditions (Šprah et al., 2017). Other factors that influence the likelihood of readmission include the individual's employment status (Böckmann et al., 2019; Callaghan & Cunningham, 2002; Donisi et al., 2016; Ramadan et al., 2022). In this context, it can be observed that individuals who are retired or unemployed are more likely to be readmitted. Furthermore, the variable "marital status" has been observed to impact the probability of readmission. Single patients tend to experience a higher rate of readmission than those who are in a couple or married (Böckmann et al., 2019; Callaghan & Cunningham, 2002; Donisi et al., 2016). Another variable that appears to affect this probability is the individual's living situation (Donisi et al., 2016), particularly whether they reside alone or with others. Regarding treatment, some authors have revealed that discharge status significantly affects the likelihood of readmission in the future (Dacosta-Sánchez et al., 2024; Ghosh et al., 2022). According to this framework, the probability of readmission is higher for patients who have discontinued treatment and who have not been discharged by a healthcare professional. As suggested by Greenfield and Wolf-Branigin (2009), patients who prematurely terminated treatment were more susceptible to requiring further therapy, possibly explaining this association.
In terms of mental disorders, the presence of comorbid mental disorders (Ghosh et al., 2022; Hutchison et al., 2019) and previous psychiatric hospitalizations (Donisi et al., 2016) have been the most consistent predictor variables in this field. No agreement exists on which comorbid disorder has the most significant impact on readmission. However, according to the review by Donisi et al. (2016), the diagnoses that impact readmission are psychotic disorders, mood disorders, and personality disorders. Previous research has also indicated that the presence of impulse control disorders influences the likelihood of readmission (Smith et al., 2015). Nevertheless, an appropriate intervention model addressing SUD and other psychiatric comorbidities can promote the recovery of these patients and yield outcomes comparable to those of patients without comorbidities (Fantuzzi & Mezzina, 2020; Newton-Howes et al., 2017; Watkins et al., 2022).
The lack of conclusive results on the factors associated with patient readmission during treatment may be explained by the heterogeneity of the samples across studies. Understanding the context in which patients undergo treatment is crucial to identifying factors associated with unsatisfactory treatment outcomes. The specialized literature on readmissions focuses primarily on rehospitalization in psychiatric or inpatient facilities, as evidenced by the review by Donisi et al. (2016) and recent research (e.g., Genis et al., 2020; Ghosh et al., 2022; Ramadan et al., 2022; Soler et al., 2021), with minimal attention given to outpatient addiction treatment. Inpatient treatment is a structured 24-h care program focused on recovery activities. Residential and inpatient treatment aims to stabilize patient recovery before patients become involved in outpatient settings and transition to an unsupervised environment. Outpatient facilities provide addiction treatment that is compatible with carrying out their daily activities. However, this comes at the cost of not having daily therapeutic supervision, which could be detrimental to their recovery process (National Institute on Drug Abuse [NIDA], 2018; Reif et al., 2014). Monitoring outpatient facilities, unlike inpatient facilities, is crucial because patients are responsible for maintaining their treatment, unlike inpatient facilities. In this context, previous studies have predominantly examined samples from individuals with either SUD or mental disorders, while studies involving individuals with dual diagnoses are scarce (Botha et al., 2018; Delayahu et al., 2014; Ghosh et al., 2022; Greenfield & Wolf-Branigin, 2009; Hutchison et al., 2019; Ramadan et al., 2022; Rømer Thomsen et al., 2018). For instance, Rømer Thomsen et al. (2018) conducted a study in a mental health unit with patients who had psychiatric comorbidities (schizophrenia and SUD) and found that comorbid diagnoses and psychiatric history were significant predictors of readmission. Additionally, they identified cannabis or amphetamine use as a strong predictor. However, it is important to note that this study was conducted within mental health units rather than outpatient centers.
On the other hand, sample sizes in clinical research are relatively limited due to the complexity of involving numerous patients (e.g., Gryczynski et al., 2021). Consequently, it is difficult to detect potential confounding variables, making the generalizability of the results questionable. This justifies the need for further investigations with larger samples to help identify possible factors for an undesirable prognosis in patients with DD in outpatient centers.
In the last decade, research with real-world data (RWD) has become an area of growing interest (Makady et al., 2017) as a complement to the usual observational studies and clinical trials in the field. One form of RWD is electronic health records (EHR), which consist of a set of health-related data (medical history, diagnoses, and information on substance consumption) on patients or the health services they receive (Arlett et al., 2022; Liao et al., 2023). These data provide access to large amounts of data collected in clinical scenarios. These records improve the ecological validity of the analyzed information and allow for the statistical control of relevant variables that affect treatment response (Corrigan-Curay et al., 2018; Koch et al., 2024; Marsch et al., 2020). In this context, cohort studies emerge as an appropriate methodology (Levin, 2006) for employing EHR data, given the necessity of large sample sizes to facilitate a comprehensive understanding and analysis of the resulting outcomes.
The current study utilized the EHR of patients with dual pathology to achieve two objectives: 1) identify sociodemographic variables, consumption patterns, and mental disorder diagnoses associated with readmission to treatment and 2) determine which variables, prior to and associated with the therapeutic process, are related to treatment dropout versus those who achieve therapeutic goals.
Materials and Methods
Design
Retrospective cohort study.
Participants
Outpatients admitted between January 1, 2015 and September 1, 2020 to specialized addiction services. Inclusion criteria were (1) having a diagnosis of an addictive disorder and another mental disorder according to the International Classification of Diseases 10 (ICD-10), and (2) attending a minimum of three appointments at their treatment centers.
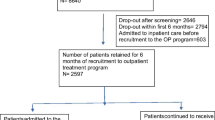
The study included 8383 patients who received treatment in one of the 121 outpatient drug abuse centers in the public network of Andalusia (a region of Spain with a population of more than 8,000,000 inhabitants). The majority of patients were male (79.6%) and had a mean age of 40.41 years (SD = 10.83). Most participants had completed primary (37.6%) or secondary (23.4%) education. In terms of employment status, 49.3% were unemployed, 19.5% were retired, 23.5% were employed, and 2.5% were studying. Concerning drug use, it is possible for patients to have multiple dependence disorders. Consequently, in the total sample, 64% of the patients were diagnosed with alcohol use disorder, 42.5% with cocaine use disorder, 36.1% with cannabis use disorder, and 21.8% with opioid use disorder. Among them, 2674 (31.9%) received coordinated care with mental health services. Out of all participants, 70.3% were readmitted to treatment (25.3% of those readmitted were for a different drug than the previous admission). These patients had not received treatment for at least six months, which aligns with the average duration recommended and used by most of the literature (Fischer et al., 2014; Rumball-Smith & Hider, 2009).
Procedure
The EHRs of the patients were used. The EHR included sociodemographic variables, drug use history, therapeutic adherence, and previous treatments. The variables are collected according to the EMCDDA protocol (EMCDDA, 2012). This protocol, known as the Treatment Demand Indicator (TDI) standard protocol 2.0, specifies a minimum set of items for national monitoring systems to record and report, ensuring data comparability across countries. The EHR is designed to avoid significant loss of information and to identify inaccuracies and inconsistencies in the responses during the review process.
Patients can also receive mental health treatment in a coordinated manner in mental health services.
Ethics and Approvals
The study received ethical approval from the Research Ethics Committee of the Ministry of Health in Andalusia, ensuring that it met the ethical standards for data management.
The storage and coding of the data adhered to the General Health Law of April 25, 1986 (Spain) and Law 41/2002 of November 14, which regulate the autonomy, rights, and obligations of patients regarding clinical information and documentation. Additionally, compliance with the Organic Law 3/2018 of December 5, 2018, governing the safeguarding of personal data and digital rights, adapted to European regulations, has been guaranteed.
The ethics protocol code for this study's project funding is "0661-N-22."
Measures
Sociodemographic variables, along with those related to consumption patterns and psychiatric comorbidities, were recorded at the beginning of treatment. Process variables were collected between the start and the end of treatment. Outcomes were recorded once the patient had completed treatment. These variables were coded as follows:
-
a)
Dropout was defined as a binary variable, where 1 represented dropout, and 0 represented patients who have completed therapy and were discharged.
-
b)
Readmission was defined as a patient re-entering treatment 6 months after discharge or dropping out. The variable is binary, with 0 indicating no readmission and 1 indicating at least one readmission.
Statistical Analysis
Initially, patients who did and did not experience readmission to treatment were compared. Differences between nominal and ordinal variables were analyzed using Pearson's chi-square test, and phi or Cramer's V statistic was used to calculate effect sizes (Cohen, 1988). The Mann‒Whitney U test was used to analyze continuous variables, and Hedges' g was used to determine the effect size, as this statistic considers different sample sizes (Hedges, 1981). Due to the large sample size, even minor differences between groups can result in statistically significant differences. Therefore, consideration was given to both the statistical significance and effect size. To enhance the statistical control between variables, multivariate analysis was used. This analysis included all covariates, even those that did not show statistical significance in the bivariate analysis, as they might still hold predictive value when included in the multivariate analysis. This comprehensive approach ensures that no potentially relevant information is overlooked.
To achieve the second objective, contingency tables were created to compare patients who received therapeutic discharge with patients who discontinued treatment. This analysis excluded patients who were in treatment, had died during treatment, or had been referred to other health resources. The same statistics were used. Finally, the study conducted a multivariate analysis to determine the variables associated with treatment abandonment using the same criteria.
All analyses were conducted using IBM SPSS Statistics software, version 29.0.1.0 (Chicago, IL, USA).
Results
Differences Between Patients with and Without Readmission to Treatment and Prediction of Readmitted Patient
Table 1 presents the sociodemographic features, substance use patterns, and psychiatric comorbidities of the patients. The data indicate a significantly higher percentage of women without readmission than of men but with a small effect size (24.9% vs. 18.5%; p < 0.001; Φ = -0.073). Significant differences and effect sizes greater than 0.1 were found in employment status between the two groups (p < 0.001; V = 0.174). A higher proportion of patients who were readmitted were either unemployed or retired. Conversely, a greater number of patients who were admitted only once were employed. Most patients in both groups cohabited with their families within 30 days before admission. It is significant to highlight that a percentage of patients who were readmitted were in prison during the 30 previous days to the onset of treatment (2.3% vs. 8.7%). A pronounced difference in the leading source of referral to treatment was found (p < 0.001; V = 0.373). Almost 65% of the readmitted patients came by their initiative. Most patients who were not readmitted were referred for treatment by health services. However, 28.5% sought treatment on their initiative. Opiate (12.4% vs. 25.8%; p < 0.001; Φ = 0.148) and cocaine (37.90% vs. 44.1%; p < 0.001; Φ = 0.060) use disorders were more prevalent among patients who were readmitted to treatment. Moreover, a higher percentage of individuals with polysubstance dependence were readmitted. Patients with a single admission exhibited superior daily use of drugs (55.4% vs. 38.0%) compared with those who were readmitted. Additionally, patients readmitted were more likely to have not consumed in the last 30 days (12.1% vs. 24.6%). Notably, individuals who were readmitted started using their primary drug at a younger age.
Regarding comorbid disorders, anxiety disorders were more prevalent among patients who had a single admission to treatment (35.1% vs. 29.0%). However, among the readmitted patients, personality disorders (19.3% vs. 29.6%; p < 0.001; Φ = 0.107), specifically Cluster B, were significantly more prevalent.
Table 2 presents the results of the multivariate analysis. The fit indicators demonstrated adequate values, with a concordance percentage of 77.9% and a concordance index (C) of 0.778.
The regression analysis indicated that older individuals were more likely to be readmitted (OR = 1.019; 95% CI: 1.012 – 1.025). Additionally, being male increased the likelihood of readmission (OR = 1.255; 95% CI: 1.088 – 1.448). It was found that individuals with jobs were less likely to be readmitted (OR = 0.579; 95% CI: 0.505 – 0.664) than those unemployed. Patients living with their families of origin, in prison (OR = 3.435; 95% CI: 2.414 – 4.887), or in other residential institutions (OR = 2.537; 95% CI: 1.603 – 4.015) were found to be more likely to experience readmission than those living alone. It has been observed that the patients referred by medical, legal, or social services were less likely to be readmitted than those who sought treatment on their own initiative. Regarding consumption patterns, patients diagnosed with opiate dependence (OR = 1.706; 95% CI: 1.424 – 2.045) or polydrug dependence (OR = 1.550; 95% CI: 1.369 – 1.755) were found to be more likely to be readmitted. Additionally, patients who abstained from substance use in the 30 days before admission had a higher probability of readmission than those who continued to consume. Moreover, patients diagnosed with personality disorders were found to be 1.499 times more likely (95% CI: 1.303 – 1.724) to experience readmission.
Outcomes and Process Therapeutic Indicators According to Readmission Treatment for Patients with Dual Disorders and Predictors of Dropout
Table 3 presents the therapeutic outcomes for patients with dual disorders in terms of discharge, retention, and adherence based on their history of readmission to treatment.
Patients who were readmitted had a greater mean number of scheduled follow-up appointments (17.49 vs. 24.15; p < 0.001; g = 0.368) but a lower attendance rate (69.03% vs. 61.45%; p < 0.001; g = 0.370). This trend was also found in diagnostic appointments.
Patients who were not readmitted had a higher rate of therapeutic discharge (16.2% vs. 7.4%) but also a higher rate of treatment dropout (37.8% vs. 33.2%).
In terms of retention, patients who have not been readmitted exhibit a significantly longer mean duration of treatment (over two months) than those who have been readmitted.
Table 4 displays a multivariate analysis exploring the factors that impact patient discharge or dropout (represented by 0 and 1, respectively). The model showed an adequate fit, the indicator of monotonic association showed a concordance percentage of 72.2%, and the concordance (C) index was 0.724.
The results of the regression analysis indicate that outpatients diagnosed with opioid dependence have twice the probability (OR = 2.183; CI: 1.186 – 4.017) of dropping out of treatment compared to those without dependence. Furthermore, more frequent substance users (OR = 1.570; CI: 1.113 – 2.215) and outpatients with previous readmissions (OR = 1.606; CI: 1.189 – 2.170) are more likely to discontinue treatment. Conversely, a lower probability of dropout was observed in older patients (OR = 0.976; CI: 0.960 – 0.992). The probability of dropping out of treatment also depends on specific variables related to the therapeutic process. In particular, patients who attend follow-up appointments more frequently (OR = 0.979; CI: 0.972 – 0.985) and those who are in treatment for a longer duration (OR = 0.978; CI: 0.969 – 0.987) are less likely to discontinue treatment.
Discussion
This study aims to add to the growing body of knowledge on outpatient addiction treatment outcomes for individuals with DD. EHRs offer valuable insights into patient and treatment-related variables affecting readmission and dropout rates. However, caution is warranted when analyzing EHRs to avoid false positive errors (Kim & Kim, 2019) and to account for the high variability in data recording (Grzenda & Widge, 2024), which can pose limitations. Consequently, in this study, the importance of the variables was determined by considering both effect size and statistical significance to mitigate this issue as much as possible. Furthermore, as a retrospective cohort study, it is not feasible to definitively establish causality (Hernán & Robins, 2020) due to the inherent limitations of the study design. Nevertheless, the data enable the generation of correlational associations and the formation of hypotheses regarding causality. This is facilitated by the collection of information on certain predictor variables at the onset of treatment or during its course, including indicators of the therapeutic process, such as adherence. Therefore, cohort studies allow for a deeper understanding of the progression of treatment up to the outcomes (Grimes & Schulz, 2002; Levin, 2006). As Brorson et al. (2013) and Grover et al. (2021) have observed, there remains a limited understanding of the factors influencing outcomes such as dropout or readmission in the substance use disorder literature, particularly in relation to therapeutic process indicators. This study aims to address this gap by examining how these outcomes manifest in dual patients, a group whose comorbidity, as documented in the literature, negatively impacts the therapeutic process and outcomes.
In line with our first objective, we observed differences in the analysis of admission profiles between the two groups of patients, enabling us to identify some variables associated with treatment readmission. The literature on SUD and gender has yielded inconsistent findings regarding its impact on readmission and therapeutic outcomes (McHugh et al., 2018). Similar to our study, some authors have reported that women have a lower likelihood of readmission (Hutchison et al., 2019) and relapse (Logan et al., 2020). Meanwhile, Maturana et al. (2023) and Smith et al. (2015) reported that women had a greater likelihood of readmission. The reasons for the variations in outcomes of SUD treatment remain unclear. Some authors (Agabio et al., 2016; McHugh et al., 2018; Ribeiro & Marinho, 2012) suggest that women experience higher unemployment rates, poverty, and social problems, which may contribute to worse outcomes. However, women also tend to seek help from doctors and health professionals more frequently than men (Callaghan & Cunningham, 2002), which may act as a factor in avoiding readmission. It is imperative to acknowledge the complexity of gender differences in treatment and the need for further research to understand the relationships among them. Consistent with most related literature (Donisi et al., 2016), more than 70% of the readmitted patients were unemployed or retired. Other studies have reported that nearly 50% of readmitted patients fall into these categories since having a SUD and a psychiatric comorbidity tend to be stigmatized and therefore associated with losing jobs (Böckmann et al., 2019; Ramadan et al., 2022). Previous studies (Böckmann et al., 2019; Carrier et al., 2011; Donisi et al., 2016) have suggested that living with children, a partner, or relatives may enhance the likelihood of reducing readmission. In our study, it appears that those patients living with their families of origin were more likely to be in the readmitted group. Family support can protect against readmission (Lorine et al., 2015), but it may also encourage individuals to seek treatment on their own when they need it. On the other hand, residing in prison within 30 days before treatment admission appears to be a significant predictor of readmission. This may be attributed to the high prevalence of individuals who suffer from SUDs in prisons (Bronson et al., 2017; Fazel et al., 2017). Additionally, SUDs may be at risk of readmission to both prisons and addiction treatment (Sadeh & McNiel, 2015), as mandated by judges and correctional facilities. The likelihood of this occurrence tends to increase when a comorbid mental disorder is present. Kopak and Raggio's (2023) study suggested that in certain areas, particularly rural ones, prisons have taken on the role of primary care centers for specific populations. Therefore, some jails have been tasked with providing or referring medical attention or addiction treatment to inmates who require it. On the other hand, according to the results, patients with multiple admissions appear to seek treatment voluntarily more frequently. It is worth noting that not consuming within the previous 30 days was a significant factor among those who were readmitted. In some cases, patients who have undergone or dropped out of treatment may have reverted to consumption and recognized a problematic pattern. In such instances, individuals may have attempted to remain abstinent and considered the need to either return to treatment or continue receiving care (Bernstein & D'Onofrio, 2017). This finding may also help explain the high percentage of patients who seek help on their own when experiencing a possible relapse in their habitual consumption. In their 2019 publication, Böckmann and colleagues suggested that early readmission could aid in preventing relapse and averting the exacerbation of psychiatric comorbidities. Within this framework, other professionals in healthcare, social, or legal services may view outpatient center treatment as the most effective approach for maintaining substance abstinence. It is necessary to consider this information when developing treatment plans for these individuals. Patients referred by the health system had a lower readmission rate. These findings are consistent with those reported by Dacosta-Sánchez et al. (2024). The authors suggest that this may be due to the authority of clinicians in promoting the benefits of starting treatment.
The results imply that readmitted patients often have an opioid or cocaine use disorder. The findings of other authors, such as Ramadan et al. (2022) and San et al. (2013), have suggested that these SUDs may act as potential triggers for readmission. Furthermore, the present study identified the presence of personality disorders, specifically Cluster B (antisocial, borderline, histrionic, and narcissistic), among readmitted patients. According to the literature, personality disorders are commonly observed in patients diagnosed with substance use and are linked to both cocaine use (Cavalera et al., 2020; Oliva et al., 2021) and opioid use (Santo et al., 2022).
Regarding the second objective, the strongest predictors of dropout seem to be opioid use disorder, substance consumption in the 30 days prior to admission, and the therapeutic process indicators, specifically non-adherence to follow-up appointments and less time spent in treatment. In addition, having previous readmissions also predicts subsequent abandonment. However, there are a few variables that need to be considered. In contrast to readmission rates, dropout rates are more likely to occur among younger patients. This is supported by the results of the review conducted by Brorson et al. (2013), which identified patient youth as one of the predictors of dropout. Previously, it has been reported that opioid use disorder is a more prevalent condition among readmitted patients than single-admission patients. It is important to note that opioid use disorder also seems to increase the likelihood of treatment abandonment, potentially perpetuating a self-defeating cycle. Therefore, the disorder may result in dropping out and needing new treatment. The relationships between opioid use and both treatment dropout (Basu et al., 2017; Brorson et al., 2013; Marcovitz et al., 2016) and readmission (Ramadan et al., 2022; Santo et al., 2022) have previously been documented in specialized literature, both in the context of the disorder itself and the consumption of the substance.
Moreover, as per previous literature (Ghosh et al., 2022), the discharge status of patients, whether they received a therapeutic discharge from their clinicians or dropped out before receiving it, affects readmission. Similarly, the study showed that a greater proportion of patients who had a single admission were successfully discharged. However, it is worth noting that they also tend to drop out of treatment more frequently than those who are readmitted (Donisi et al., 2016), despite being in therapy for a lengthier average number of months. Nevertheless, it has been observed that a longer duration of treatment can protect against dropout in dual patients (Daigre et al., 2019, 2021; González-Saiz et al., 2014). Therefore, it is imperative to strive for good treatment retention to avoid dropout and relapse. In terms of adherence, patients with more than one treatment admission had a greater number of scheduled appointments but a lower percentage of visits. Both retention and adherence have previously been shown to play principal roles in treatment success (Dacosta-Sánchez et al., 2022; NIDA, 2018; Viera et al., 2020).
It is worth noting that despite the limitations inherent to using EHRs, this study includes one of the largest samples of dual patients in outpatient centers to date. A sample of this size enhances the representativeness of the studied population, thereby increasing the external validity of the findings. The extensive data collected allows for more robust analyses and more reliable conclusions regarding trends and outcomes within this specific population. Additionally, this study included comprehensive data on patient admissions and outcomes, offering a detailed overview of their clinical trajectory. Such information is crucial for gaining a deeper understanding of the factors influencing the care and outcomes of dual patients and can help identify areas for improvement in clinical practice and health management. Furthermore, it is important to highlight that most previous studies have been conducted in hospitals or inpatient facilities. In contrast, this study focused on outpatient centers, providing a unique perspective on the care of dual patients in a less intensive setting. The results of this study could help clinicians keep better track of DD patients who drop out of treatment and re-enter the system later.
Data Availability
References
Agabio, R., Campesi, I., Pisanu, C., Gessa, G. L., & Franconi, F. (2016). Sex differences in substance use disorders: Focus on side effects. Addiction Biology, 21(5), 1030–1042. https://doi.org/10.1111/adb.12395
Ambrosio-Flores, E., & Alguacil-Merino, L. F. (2023). Conceptos fundamentales en drogodependencias. In M. I. Colado, M. Farré, J. C. Leza, & I. Lizasoain (Eds.), Drogodependencias (pp. 3–11). Editorial Médica Panamericana.
Arlett, P., Kjaer, J., Broich, K., & Cooke, E. (2022). Real-world evidence in EU medicines regulation: Enabling use and establishing value. Clinical Pharmacology and Therapeutics, 111(1), 21–23. https://doi.org/10.1002/cpt.2479
Basu, D., Ghosh, A., Sarkar, S., Patra, B., Subodh, B., & Mattoo, S. (2017). Initial treatment dropout in patients with substance use disorders attending a tertiary care de-addiction centre in north India. Indian Journal of Medical Research, 146(8), 77. https://doi.org/10.4103/ijmr.IJMR_1309_15
Becker, E. A., & Shafer, A. (2007). Voluntary readmission among schizophrenic patients in the Texas state psychiatric hospital system. Texas Medicine, 103(9), 54–59.
Bernstein, S. L., & D’Onofrio, G. (2017). Screening, treatment initiation, and referral for substance use disorders. Addiction Science & Clinical Practice, 12(1), 18. https://doi.org/10.1186/s13722-017-0083-z
Blackwood, R., Lynskey, M., & Drummond, C. (2021). Prevalence and patterns of hospital use for people with frequent alcohol-related hospital admissions, compared to non-alcohol and non-frequent admissions: A cohort study using routine administrative hospital data. Addiction (abingdon, England), 116(7), 1700–1708. https://doi.org/10.1111/add.15354
Böckmann, V., Lay, B., Seifritz, E., Kawohl, W., Roser, P., & Habermeyer, B. (2019). Patient-level predictors of psychiatric readmission in substance use disorders. Frontiers in Psychiatry, 10, 828. https://doi.org/10.3389/fpsyt.2019.00828
Botha, U. A., Koen, L., Mazinu, M., Jordaan, E., & Niehaus, D. J. H. (2018). Brief report: A randomized control trial assessing the influence of a telephone-based intervention on readmissions for patients with severe mental illness in a developing country. Community Mental Health Journal, 54(2), 197–203. https://doi.org/10.1007/s10597-016-0069-4
Bronson, J., Stroop, J., Zimmer, S., & Berzofsky, M. (2017). Drug use, dependence, and abuse among state prisoners and jail inmates, 2007–2009: Special report. Bureau of Justice Statistics, U.S. Department of Justice. Retrieved May 22, 2024, from https://www.bjs.gov/content/pub/pdf/dudaspji0709.pdf
Brorson, H. H., Ajo Arnevik, E., Rand-Hendriksen, K., & Duckert, F. (2013). Drop-out from addiction treatment: A systematic review of risk factors. Clinical Psychology Review, 33(8), 1010–1024. https://doi.org/10.1016/j.cpr.2013.07.007
Callaghan, R. C., & Cunningham, J. A. (2002). Gender differences in detoxification: Predictors of completion and re-admission. Journal of Substance Abuse Treatment, 23(4), 399–407. https://doi.org/10.1016/s0740-5472(02)00302-1
Carrier, E., McNeely, J., Lobach, I., Tay, S., Gourevitch, M. N., & Raven, M. C. (2011). Factors associated with frequent utilization of crisis substance use detoxification services. Journal of Addictive Diseases, 30(2), 116–122. https://doi.org/10.1080/10550887.2011.554776
Cavalera, C., Ferrari, C., Bianconi, G., Bulgari, V., Candini, V., Carrà, G., Clerici, M., Conte, G., Cricelli, M., Ferla, M. T., Iozzino, L., Macis, A., Stefana, A., Ornaghi, A., de Girolamo, G., & VIORMED-2 Group. (2020). Substance use disorders and violent behavior in patients with severe mental disorders: A prospective, multicentre study. The Australian and New Zealand Journal of Psychiatry, 54(12), 1212–1223.https://doi.org/10.1177/0004867420963732.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Routledge.https://doi.org/10.4324/9780203771587.
Corrigan-Curay, J., Sacks, L., & Woodcock, J. (2018). Real-world evidence and real-world data for evaluating drug safety and effectiveness. JAMA: The Journal of the American Medical Association, 320(9), 867. https://doi.org/10.1001/jama.2018.10136.
Dacosta-Sánchez, D., Díaz-Batanero, C., Fernandez-Calderon, F., & Lozano, Ó. M. (2021). Impact of Cluster B personality disorders in drugs therapeutic community treatment outcomes: A study based on real-world data. Journal of Clinical Medicine, 10(12), 2572. https://doi.org/10.3390/jcm10122572
Dacosta-Sánchez, D., Fernández-Calderón, F., Blanc-Molina, A., Díaz-batanero, C., & Lozano, O. M. (2023). Monitoring adherence and abstinence of cannabis use disorder patients: Profile identification and relationship with long-term treatment outcomes. Journal of Substance Abuse Treatment, 148, 209019. https://doi.org/10.1016/j.josat.2023.209019
Dacosta-Sánchez, D., González-Ponce, B. M., Fernández-Calderón, F., Sánchez-García, M., & Lozano, O. M. (2022). Retention in treatment and therapeutic adherence: How are these associated with therapeutic success? An analysis using real‐world data. International Journal of Methods in Psychiatric Research, 31(4), e1929. https://doi.org/10.1002/mpr.1929
Dacosta-Sánchez, D., Fernández-Calderón, F., Díaz-Batanero, C., Mancheño-Velasco, C., & Lozano, Ó. M. (2024). Modeling the therapeutic process of patients with cocaine use disorders: A guide for predicting readmission. European Addiction Research, 30(2), 80–93. https://doi.org/10.1159/000535689
Daigre, C., Perea-Ortueta, M., Berenguer, M., Esculies, O., Sorribes-Puertas, M., Palma-Alvarez, R., Martínez-Luna, N., Ramos-Quiroga, J. A., & Grau-López, L. (2019). Psychiatric factors affecting recovery after a long-term treatment program for substance use disorder. Psychiatry Research, 276, 283–289. https://doi.org/10.1016/j.psychres.2019.05.026
Daigre, C., Rodríguez, L., Roncero, C., Palma-Álvarez, R. F., Perea-Ortueta, M., Sorribes-Puertas, M., Martínez-Luna, N., Ros-Cucurull, E., Ramos-Quiroga, J. A., & Grau-López, L. (2021). Treatment retention and abstinence of patients with substance use disorders according to addiction severity and psychiatry comorbidity: A six-month follow-up study in an outpatient unit. Addictive Behaviors, 117(106832), 106832. https://doi.org/10.1016/j.addbeh.2021.106832
Delayahu, Y., Nehama, Y., Sagi, A., Baruch, Y., & Blass, M. D. (2014). Evaluating the clinical impact of involuntary admission to a specialized dual diagnosis ward. The Israel Journal of Psychiatry and Related Sciences, 51(4), 290–295.
Department of Health (2004). Relapse prevention and management. From Working with young people on AOD issues: learner’s workbook. Canberra: Australian Government Department of Health.
Dixon, L. B., Holoshitz, Y., & Nossel, I. (2016). Treatment engagement of individuals experiencing mental illness: Review and update. World Psychiatry, 15(1), 13–20. https://doi.org/10.1002/wps.20306
Donisi, V., Tedeschi, F., Wahlbeck, K., Haaramo, P., & Amaddeo, F. (2016). Pre-discharge factors predicting readmissions of psychiatric patients: A systematic review of the literature. BMC Psychiatry, 16(1), 449. https://doi.org/10.1186/s12888-016-1114-0
Durbin, J., Lin, E., Layne, C., & Teed, M. (2007). Is readmission a valid indicator of the quality of inpatient psychiatric care? The Journal of Behavioral Health Services & Research, 34(2), 137–150. https://doi.org/10.1007/s11414-007-9055-5
European Monitoring Centre for Drugs and Drug Addiction. (2012). Treatment demand indicator (TDI) standard protocol 3.0: Guidelines for reporting data on people entering drug treatment in European countries. Publications Office of the European Union. https://doi.org/10.2810/5285
European Monitoring Centre for Drugs and Drug Addiction (2023). European drug report 2023: Trends and developments. Publications Office of the European Union. Retrieved May 22, 2024, from https://www.emcdda.europa.eu/publications/european-drug-report/2023_en
Fantuzzi, C., & Mezzina, R. (2020). Dual diagnosis: A systematic review of the organization of community health services. The International Journal of Social Psychiatry, 66(3), 300–310. https://doi.org/10.1177/0020764019899975
Fazel, S., Yoon, I. A., & Hayes, A. J. (2017). Substance use disorders in prisoners: An updated systematic review and meta-regression analysis in recently incarcerated men and women. Addiction, 112(10), 1725–1739. https://doi.org/10.1111/add.13877
Fischer, C., Lingsma, H. F., Marang-van De Mheen, P. J., Kringos, D. S., Klazinga, N. S., & Steyerberg, E. W. (2014). Is the readmission rate a valid quality indicator? A review of the evidence. PLoS ONE9(11), e112282. https://doi.org/10.1371/journal.pone.0112282
Geniş, B., Coşar, B., & Arikan, Z. (2020). Readmission rates and causes in alcohol addiction patients within the first six months after discharge. Noro Psikiyatri Arsivi, 58(1), 57–62. https://doi.org/10.29399/npa.25077
Ghosh, A., Sharma, N., Noble, D., Basu, D., Mattoo, S. K., Bn, S., & Pillai, R. R. (2022). Predictors of five-year readmission to an inpatient service among patients with alcohol use disorders: Report from a low-middle income country. Substance Use & Misuse, 57(1), 123–133. https://doi.org/10.1080/10826084.2021.1990341
González-Saiz, F., Vergara-Moragues, E., Verdejo-García, A., Fernández-Calderón, F., & Lozano, O. M. (2014). Impact of psychiatric comorbidity on the in-treatment outcomes of cocaine-dependent patients in therapeutic communities. Substance Abuse, 35(2), 133–140. https://doi.org/10.1080/08897077.2013.812544
Greenfield, L., & Wolf-Branigin, M. (2009). Mental health indicator interaction in predicting substance abuse treatment outcomes in Nevada. The American Journal of Drug and Alcohol Abuse, 35(5), 350–357. https://doi.org/10.1080/00952990903108223
Grimes, D. A., & Schulz, K. F. (2002). Cohort studies: Marching towards outcomes. The Lancet, 359(9303), 341–345. https://doi.org/10.1016/S0140-6736(02)07500-1
Grover, S., Mallnaik, S., Chakrabarti, S., & Mehra, A. (2021). Factors associated with dropout from treatment: An exploratory study. Indian Journal of Psychiatry, 63(1), 41. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_87_19
Gryczynski, J., Nordeck, C. D., Welsh, C., Mitchell, S. G., O’Grady, K. E., & Schwartz, R. P. (2021). Preventing hospital readmission for patients with comorbid substance use disorder: A randomized trial. Annals of Internal Medicine, 174(7), 899–909. https://doi.org/10.7326/m20-5475
Grzenda, A., & Widge, A. S. (2024). Electronic health records and stratified psychiatry: Bridge to precision treatment? Neuropsychopharmacology, 49, 285–290. https://doi.org/10.1038/s41386-023-01724-y
Hedges, L. V. (1981). Distribution theory for Glass’s estimator of effect size and related estimators. Journal of Educational Statistics, 6(2), 107–128. https://doi.org/10.3102/10769986006002107
Hernán, M. A., & Robins, J. M. (2020). Causal Inference: What If. Chapman & Hall/CRC.
Hutchison, S. L., Flanagan, J. V., Karpov, I., Elliott, L., Holsinger, B., Edwards, J., & Loveland, D. (2019). Care management intervention to decrease psychiatric and substance use disorder readmissions in Medicaid-enrolled adults. The Journal of Behavioral Health Services & Research, 46(3), 533–543. https://doi.org/10.1007/s11414-018-9614-y
Kim, H. M., Pfeiffer, P., Ganoczy, D., & Valenstein, M. (2011). Intensity of outpatient monitoring after discharge and psychiatric rehospitalization of veterans with depression. Psychiatric Services (Washington, D.C.), 62(11), 1346–1352. https://doi.org/10.1176/ps.62.11.pss6211_1346.
Kim, H. S., & Kim, J. H. (2019). Proceed with caution when using real world data and real world evidence. Journal of Korean Medical Science, 34(4), e28. https://doi.org/10.3346/jkms.2019.34.e28
Koch, E., Pardiñas, A. F., O’Connell, K. S., Selvaggi, P., Collados, J. C., Babic, A., Marshall, S. E., Van der Eycken, E., Angulo, C., Lu, Y., Sullivan, P. F., Dale, A. M., Molden, E., Posthuma, D., White, N., Schubert, A., Djurovic, S., Heimer, H., Stefánsson, H., … Andreassen, O. A. (2024). How real-world data can facilitate the development of precision medicine treatment in psychiatry. Biological Psychiatry, S0006–3223(24)00003–9. https://doi.org/10.1016/j.biopsych.2024.01.001.
Kopak, A., & Raggio, A. (2023). Substance use disorder and rural detention center readmission: Results from a 3-year prospective cohort study. Rural Mental Health, 47(3), 129–138. https://doi.org/10.1037/rmh0000231
Krawczyk, N., Feder, K. A., Saloner, B., Crum, R. M., Kealhofer, M., & Mojtabai, R. (2017). The association of psychiatric comorbidity with treatment completion among clients admitted to substance use treatment programs in a U.S. national sample. Drug and Alcohol Dependence, 175, 157–163. https://doi.org/10.1016/j.drugalcdep.2017.02.006
Levin, K. A. (2006). Study design IV: Cohort studies. Evidence-Based Dentistry, 7(2), 51–52. https://doi.org/10.1038/sj.ebd.6400407
Liao, X., Yao, C., Zhang, J., & Liu, L. Z. (2023). Recent advancement in integrating artificial intelligence and information technology with real-world data for clinical decision-making in China: A scoping review. Journal of Evidence-Based Medicine, 16(4), 534–546. https://doi.org/10.1111/jebm.12549
Logan, T., Cole, J., & Walker, R. (2020). Examining recovery program participants by gender: program completion, relapse, and multidimensional status 12 months after program entry. Journal of Drug Issues, 50(4), 436–454. https://doi.org/10.1177/0022042620923985
Lorine, K., Goenjian, H., Kim, S., Steinberg, A. M., Schmidt, K., & Goenjian, A. K. (2015). Risk factors associated with psychiatric readmission. The Journal of Nervous and Mental Disease, 203(6), 425–430. https://doi.org/10.1097/NMD.0000000000000305
Makady, A., de Boer, A., Hillege, H., Klungel, O., & Goettsch, W. (2017). What is real-world data? A review of definitions based on literature and stakeholder interviews. Value in Health: The Journal of the International Society for Pharmacoeconomics and Outcomes Research, 20(7), 858–865. https://doi.org/10.1016/j.jval.2017.03.008
Marcovitz, D. E., McHugh, R. K., Volpe, J., Votaw, V., & Connery, H. S. (2016). Predictors of early dropout in outpatient buprenorphine/naloxone treatment. The American Journal on Addictions, 25(6), 472–477. https://doi.org/10.1111/ajad.12414
Marsch, L. A., Campbell, A., Campbell, C., Chen, C.-H., Ertin, E., Ghitza, U., Lambert-Harris, C., Hassanpour, S., Holtyn, A. F., Hser, Y.-I., Jacobs, P., Klausner, J. D., Lemley, S., Kotz, D., Meier, A., McLeman, B., McNeely, J., Mishra, V., Mooney, L., … Young, S. (2020). The application of digital health to the assessment and treatment of substance use disorders: The past, current, and future role of the National Drug Abuse Treatment Clinical Trials Network. Journal of Substance Abuse Treatment, 112, 4–11. https://doi.org/10.1016/j.jsat.2020.02.005.
Maturana, J.R.-T., Cruz, A.G.-S., Rocha-Jiménez, T., & Castillo-Carniglia, Á. (2023). Does substance use disorder treatment completion reduce the risk of treatment readmission in Chile? Drug and Alcohol Dependence, 248(109907), 109907. https://doi.org/10.1016/j.drugalcdep.2023.109907
McHugh, R. K., Votaw, V. R., Sugarman, D. E., & Greenfield, S. F. (2018). Sex and gender differences in substance use disorders. Clinical Psychology Review, 66, 12–23. https://doi.org/10.1016/j.cpr.2017.10.012
Melville, K. M., Casey, L. M., & Kavanagh, D. J. (2010). Dropout from Internet-based treatment for psychological disorders. The British Journal of Clinical Psychology, 49(4), 455–471. https://doi.org/10.1348/014466509X472138
National Institute on Drug Abuse (NIDA). (2018). Principles of drug addiction treatment: A research-based guide (3rd ed.). Retrieved May 22, 2024, from https://archives.nida.nih.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition
Newton-Howes, G. M., Foulds, J. A., Guy, N. H., Boden, J. M., & Mulder, R. T. (2017). Personality disorder and alcohol treatment outcome: Systematic review and meta-analysis. The British Journal of Psychiatry: The Journal of Mental Science, 211(1), 22–30. https://doi.org/10.1192/bjp.bp.116.194720
Oliva, F., Mangiapane, C., Nibbio, G., Berchialla, P., Colombi, N., & Vigna-Taglianti, F. D. (2021). Prevalence of cocaine use and cocaine use disorder among adult patients with attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Journal of Psychiatric Research, 143, 587–598. https://doi.org/10.1016/j.jpsychires.2020.11.021
Pennay, A., Cameron, J., Reichert, T., Strickland, H., Lee, N. K., Hall, K., & Lubman, D. I. (2011). A systematic review of interventions for co-occurring substance use disorder and borderline personality disorder. Journal of Substance Abuse Treatment, 41(4), 363–373. https://doi.org/10.1016/j.jsat.2011.05.004
Ramadan, M., Alharbi, A., Ahmad, R. G., Alkhalaf, A., Alhusseini, N., Algarni, A. S., & Mohamed, I. S. (2022). Evaluation of substance use disorder readmission and length of hospital stay in a major rehabilitation center in the Gulf States: A retrospective cohort study. International Journal of Mental Health and Addiction, 1–16. https://doi.org/10.1007/s11469-022-00920-z
Reif, S., George, P., Braude, L., Dougherty, R. H., Daniels, A. S., Ghose, S. S., & Delphin-Rittmon, M. E. (2014). Residential treatment for individuals with substance use disorders: Assessing the evidence. Psychiatric Services (Washington, D.C.), 65(3), 301–312. https://doi.org/10.1176/appi.ps.201300242.
Ribeiro, L. L., & Marinho, E. (2012). Time poverty in Brazil: Measurement and analysis of its determinants. Estudios De Economia, 42(2), 285–306. https://doi.org/10.1590/S0101-41612012000200003
Ries, R. K. (1992). Serial, parallel, and integrated models of dual-diagnosis treatment. Journal of Health Care for the Poor and Underserved, 3(1), 173–180. https://doi.org/10.1353/hpu.2010.0283
Rømer Thomsen, K., Thylstrup, B., Pedersen, M. M., Pedersen, M. U., Simonsen, E., & Hesse, M. (2018). Drug-related predictors of readmission for schizophrenia among patients admitted to treatment for drug use disorders. Schizophrenia Research, 195, 495–500. https://doi.org/10.1016/j.schres.2017.09.026
Rumball-Smith, J., & Hider, P. (2009). The validity of readmission rate as a marker of the quality of hospital care, and a recommendation for its definition. The New Zealand Medical Journal, 122(1289), 63–70.
Sadeh, N., & McNiel, D. E. (2015). Posttraumatic stress disorder increases risk of criminal recidivism among justice-involved persons with mental disorders. Criminal Justice and Behavior, 42(6), 573–586. https://doi.org/10.1177/0093854814556880
San, L., Bernardo, M., Gómez, A., & Peña, M. (2013). Factors associated with relapse in patients with schizophrenia. International Journal of Psychiatry in Clinical Practice, 17(1), 2–9. https://doi.org/10.3109/13651501.2012.687452
Santo, T., Jr., Campbell, G., Gisev, N., Martino-Burke, D., Wilson, J., Colledge-Frisby, S., Clark, B., Tran, L. T., & Degenhardt, L. (2022). Prevalence of mental disorders among people with opioid use disorder: A systematic review and meta-analysis. Drug and Alcohol Dependence, 238, 109551. https://doi.org/10.1016/j.drugalcdep.2022.109551
Smith, M. W., Stocks, C., & Santora, P. B. (2015). Hospital readmission rates and emergency department visits for mental health and substance abuse conditions. Community Mental Health Journal, 51(2), 190–197. https://doi.org/10.1007/s10597-014-9784-x
Soler, S., Montout, C., Pepin, B., Abbar, M., Mura, T., & Lopez-Castroman, J. (2021). Impact of cannabis use on outcomes of patients admitted to an involuntary psychiatric unit: A retrospective cohort study. Journal of Psychiatric Research, 138, 507–513. https://doi.org/10.1016/j.jpsychires.2021.04.024
Šprah, L., Dernovšek, M. Z., Wahlbeck, K., & Haaramo, P. (2017). Psychiatric readmissions and their association with physical comorbidity: A systematic literature review. BMC Psychiatry, 17(1), 2. https://doi.org/10.1186/s12888-016-1172-3
Substance Abuse and Mental Health Services Administration (SAMHSA). (2022). Treatment episode data set (TEDS): 2020 admissions to and discharges from publicly funded substance use treatment facilities. Substance Abuse and Mental Health Services Administration. Retrieved May 22, 2024, from https://www.samhsa.gov/data/report/treatment-episode-data-set-teds-2020-admissions
Viera, A., Bromberg, D. J., Whittaker, S., Refsland, B. M., Stanojlović, M., Nyhan, K., & Altice, F. L. (2020). Adherence to and retention in medications for opioid use disorder among adolescents and young adults. Epidemiologic Reviews, 42(1), 41–56. https://doi.org/10.1093/epirev/mxaa001
Wade, D., Harrigan, S., Edwards, J., Burgess, P. M., Whelan, G., & McGorry, P. D. (2006). Substance misuse in first-episode psychosis: 15-month prospective follow-up study. The British Journal of Psychiatry: The Journal of Mental Science, 189(3), 229–234. https://doi.org/10.1192/bjp.bp.105.017236
Watkins, L. E., Patton, S. C., Drexler, K., Rauch, S. A. M., & Rothbaum, B. O. (2022). Clinical effectiveness of an intensive outpatient program for integrated treatment of comorbid substance abuse and mental health disorders. Cognitive and Behavioral Practice, 30(3), 354–366.https://doi.org/10.1016/j.cbpra.2022.05.005
Acknowledgements
This study has been developed thanks to the transfer of data by the Department of Equality, Social Policies and Conciliation of the Junta de Andalucía.
Funding
Funding for open access publishing: Universidad de Huelva/CBUA This study was supported by the grant “COMPARA: Comorbilidad Psiquiátrica en Adicciones y Resultados en Andalucía. Modelización a través de Big Data”, project P20_00735 on Andalusian Research, Development and Innovation Plan, provided by Fondo Europeo de Desarrollo Regional (EU) and Junta de Andalucía (Spain).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics and Approvals
The study received ethical approval from the Research Ethics Committee of the Ministry of Health in Andalusia, ensuring that it met the ethical standards for data management. The storage and coding of the data adhered to the General Health Law of April 25, 1986 (Spain) and Law 41/2002 of November 14, which regulate the autonomy, rights, and obligations of patients regarding clinical information and documentation. Additionally, compliance with the Organic Law 3/2018 of December 5, 2018, governing the safeguarding of personal data and digital rights, adapted to European regulations, has been guaranteed.
Conflict of Interest
Authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mancheño-Velasco, C., Narváez-Camargo, M., Lozano-Rojas, Ó.M. et al. Readmission and Dropout in Outpatient Centers: An Analysis of Real-World Data in Patients with Dual-Diagnosis. Int J Ment Health Addiction (2024). https://doi.org/10.1007/s11469-024-01360-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s11469-024-01360-7