Abstract
Biopsy is a method commonly used for early cancer diagnosis. However, bleeding complications of widely available biopsy are risky for patients. Safer biopsy will result in a more accurate cancer diagnosis and a decrease in the risk of complications. In this article, we propose a novel biopsy needle that can reduce bleeding during biopsy procedures and achieve stable hemostasis. The proposed biopsy needle features a compact structure and can be operated easily by left and right hands. A predictive model for puncture force and tip deflection based on coupled Eulerian–Lagrangian (CEL) method is developed. Experimental results show that the biopsy needle can smoothly deliver the gelatin sponge hemostatic plug into the tissue. Although the hemostatic plug bends, the overall delivery process is stable, and the hemostatic plug retains in the tissue without being affected by the withdrawal of the needle. Further experiments indicate that the specimens are well obtained and evenly distributed in the groove of the outer needle without scattering. Our proposed design of biopsy needle possesses strong ability of hemostasis, tissue cutting, and tissue retention. The CEL model accurately predicts the peak of puncture force and produces close estimation of the insertion force at the postpuncture stage and tip position.

Similar content being viewed by others
Abbreviations
- CEL:
-
Coupled Eulerian–Lagrangian
- FEA:
-
Finite element analysis
- ID:
-
Inner diameter
- OD:
-
Outer diameter
- C 10 :
-
Shear modulus of the tissue
- E n :
-
Young’s modulus of the needle
- f :
-
Frictional resistance
- g 1 g 2 :
-
Relaxation moduli of parts 1 and 2, respectively
- G 0 :
-
Relaxation modulus G(t) evaluated in t = 0
- G i :
-
Relaxation modulus G(t) evaluated in t = τi
- G(t):
-
Relaxation modulus
- J :
-
Elastic volume ratio
- k :
-
Bulk modulus
- K :
-
Stiffness coefficient of spring A
- m :
-
Mass of the slider and inner needle
- p :
-
Hydrostatic pressure
- t :
-
Cutting time
- v :
-
Cutting velocity
- W :
-
Strain energy density
- x :
-
Displacement of slider
- µ :
-
Shear modulus
- λ i :
-
Shield gravity
- σ :
-
Nominal stress
- σi :
-
Nominal stress component
- ε :
-
Principal stain
- ε i :
-
Principal stain component
- v n :
-
Poisson’s ratio of the needle
- ρ n :
-
Density of the needle
- ρ t :
-
Density of the tissue
- τ i (i = 1,2):
-
Relaxation time
References
Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, MacIntyre M F, Allen C, Hansen G, Woodbrook R, Wolfe C, Hamadeh R R, Moore A, Werdecker A, Gessner B D, Te Ao B, McMahon B, Karimkhani C, Yu C H, Cooke G S, Schwebel D C, Carpenter D O, Pereira D M, Nash D, Kazi D S, De Leo D, Plass D, Ukwaja K N, Thurston G D, Jin K Y, Simard E P, Mills E, Park E K, Catalá-López F, deVeber G, Gotay C, Khan G, Hosgood H D III, Santos I S, Leasher J L, Singh J, Leigh J, Jonas J B, Sanabria J, Beardsley J, Jacobsen K H, Takahashi K, Franklin R C, Ronfani L, Montico M, Naldi L, Tonelli M, Geleijnse J, Petzold M, Shrime M G, Younis M, Yonemoto N, Breitborde N, Yip P, Pourmalek F, Lotufo P A, Esteghamati A, Hankey G J, Ali R, Lunevicius R, Malekzadeh R, Dellavalle R, Weintraub R, Lucas R, Hay R, Rojas-Rueda D, Westerman R, Sepanlou S G, Nolte S, Patten S, Weichenthal S, Abera S F, Fereshtehnejad S M, Shiue I, Driscoll T, Vasankari T, Alsharif U, Rahimi-Movaghar V, Vlassov V V, Marcenes W S, Mekonnen W, Melaku Y A, Yano Y, Artaman A, Campos I, MacLachlan J, Mueller U, Kim D, Trillini M, Eshrati B, Williams H C, Shibuya K, Dandona R, Murthy K, Cowie B, Amare A T, Antonio C A, Castañeda-Orjuela C, van Gool C H, Violante F, Oh I H, Deribe K, Soreide K, Knibbs L, Kereselidze M, Green M, Cardenas R, Roy N, Tillmann T, Li Y M, Krueger H, Monasta L, Dey S, Sheikhbahaei S, Hafezi-Nejad N, Kumar G A, Sreeramareddy C T, Dandona L, Wang H D, Vollset S E, Mokdad A, Salomon J A, Lozano R, Vos T, Forouzanfar M, Lopez A, Murray C, Naghavi M. The global burden of cancer 2013. JAMA Oncology, 2015, 1(4): 505–527
Burgard C, Stahl R, de Figueiredo G N, Dinkel J, Liebig T, Cioni D, Neri E, Trumm C G. Percutaneous CT fluoroscopy-guided core needle biopsy of mediastinal masses: technical outcome and complications of 155 procedures during a 10-year period. Diagnostics, 2021, 11(5): 781
James T W, Baron T H. A comprehensive review of endoscopic ultrasound core biopsy needles. Expert Review of Medical Devices, 2018, 15(2): 127–135
Tanisaka Y, Mizuide M, Fujita A, Ogawa T, Araki R, Suzuki M, Katsuda H, Saito Y, Miyaguchi K, Tashima T, Mashimo Y, Yasuda M, Ryozawa S. Comparison of endoscopic ultrasound-guided fine-needle aspiration and biopsy device for lymphadenopathy. Gastroenterology Research and Practice, 2021, 6640862
Kurita A, Yasukawa S, Zen Y, Yoshimura K, Ogura T, Ozawa E, Okabe Y, Asada M, Nebiki H, Shigekawa M, Ikeura T, Eguchi T, Maruyama H, Ueki T, Itonaga M, Hashimoto S, Shiomi H, Minami R, Hoki N, Takenaka M, Itokawa Y, Uza N, Hashigo S, Yasuda H, Takada R, Kamada H, Kawamoto H, Kawakami H, Moriyama I, Fujita K, Matsumoto H, Hanada K, Takemura T, Yazumi S. Comparison of a 22-gauge franseen-tip needle with a 20-gauge forward-bevel needle for the diagnosis of type 1 autoimmune pancreatitis: a prospective, randomized, controlled, multicenter study (COMPAS study). Gastrointestinal Endoscopy, 2020, 91(2): 373–381
Ashat M, Klair J S, Rooney S L, Vishal S J, Jensen C, Sahar N, Murali A R, El-Abiad R, Gerke H. Randomized controlled trial comparing the franseen needle with the fork-tip needle for EUS-guided fine-needle biopsy. Gastrointestinal Endoscopy, 2021, 93(1): 140–150
Hedenström P, Demir A, Khodakaram K, Nilsson O, Sadik R. EUS-guided reverse bevel fine-needle biopsy sampling and open tip fine-needle aspiration in solid pancreatic lesions—a prospective, comparative study. Scandinavian Journal of Gastroenterology, 2018, 53(2): 231–237
de Jong T L, Pluymen L H, van Gerwen D J, Kleinrensink G J, Dankelman J, van den Dobbelsteen J J. PVA matches human liver in needle-tissue interaction. Journal of the Mechanical Behavior of Biomedical Materials, 2017, 69: 223–228
Mukai S, Itoi T, Yamaguchi H, Sofuni A, Tsuchiya T, Tanaka R, Tonozuka R, Honjo M, Fujita M, Yamamoto K, Matsunami Y, Asai Y, Kurosawa T, Nagakawa Y. A retrospective histological comparison of EUS-guided fine-needle biopsy using a novel franseen needle and a conventional end-cut type needle. Endoscopic Ultrasound, 2019, 8(1): 50–57
Eiro M, Katoh T, Watanabe T. Risk factors for bleeding complications in percutaneous renal biopsy. Clinical and Experimental Nephrology, 2005, 9(1): 40–45
Csukas D, Urbanics R, Moritz A, Ellis-Behnke R. AC5 Surgical Hemostat™ as an effective hemostatic agent in an anticoagulated rat liver punch biopsy model. Nanomedicine: Nanotechnology, Biology, and Medicine, 2015, 11(8): 2025–2031
Lyle M A, Dean D S. Ultrasound-guided fine-needle aspiration biopsy of thyroid nodules in patients taking novel oral anticoagulants. Thyroid, 2015, 25(4): 373–376
Fujita M, Shiotani A, Murao T, Ishii M, Yamanaka Y, Nakato R, Matsumoto H, Tarumi K, Manabe N, Kamada T, Hata J, Haruma K. Safety of gastrointestinal endoscopic biopsy in patients taking antithrombotics. Digestive Endoscopy, 2015, 27(1): 25–29
Deng C X, Dogra V, Exner A A, Wang H S, Bhatt S, Zhou Y, Stowe N T, Haaga J R. A feasibility study of high intensity focused ultrasound for liver biopsy hemostasis. Ultrasound in Medicine & Biology, 2004, 30(11): 1531–1537
Viola F, Mauldin F W, Lin-Schmidt X, Haverstick D M, Lawrence M B, Walker W F. A novel ultrasound-based method to evaluate hemostatic function of whole blood. Clinica Chimica Acta, 2010, 411(1–2): 106–113
Alotaibi M, Shrouder-Henry J, Amaral J, Parra D, Temple M, John P, Connolly B. The positive color Doppler sign post biopsy: effectiveness of US-directed compression in achieving hemostasis. Pediatric Radiology, 2011, 41(3): 362–368
Abdulhak A H, Nichols C S. Stick and move: hemostasis for inpatient punch biopsies. Journal of the American Academy of Dermatology, 2021 (in press)
Rahal Junior A, Falsarella P M, Ferreira V T R, Mariotti G C, de Queiroz M R G, Garcia R G. Injecting hemostatic matrix in the path of biopsies: efficacy, potential complications, and the management of such complications. Radiologia Brasileira, 2018, 51(2): 102–105
Wong P, Johnson K J, Warner R L, Merz S I, Kruger G H, Weitzel W F. Performance of biopsy needle with therapeutic injection system to prevent bleeding complications. Journal of Medical Devices, 2013, 7(1): 011002
Su B Q, Yu S, Yan H, Hu Y D, Buzurovic I, Liu D Y, Liu L L, Teng Y L, Tang J, Wang J C, Liu W Y. Biopsy needle system with a steerable concentric tube and online monitoring of electrical resistivity and insertion forces. IEEE Transactions on Biomedical Engineering, 2021, 68(5): 1702–1713
Lapouge G, Poignet P, Troccaz J. Towards 3D ultrasound guided needle steering robust to uncertainties, noise, and tissue heterogeneity. IEEE Transactions on Biomedical Engineering, 2021, 68(4): 1166–1177
Misra S, Reed K B, Schafer B W, Ramesh K T, Okamura A M. Mechanics of flexible needles robotically steered through soft tissue. International Journal of Robotics Research, 2010, 29(13): 1640–1660
Jushiddi M G, Mani A, Silien C, Tofail S A M, Tiernan P, Mulvihill J J E. A computational multilayer model to simulate hollow needle insertion into biological porcine liver tissue. Acta Biomaterialia, 2021, 136: 389–401
Konh B, Honarvar M, Darvish K, Hutapea P. Simulation and experimental studies in needle–tissue interactions. Journal of Clinical Monitoring and Computing, 2017, 31(4): 861–872
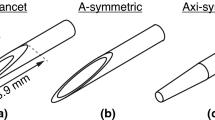
Jiang S, Li P, Yu Y, Liu J, Yang Z Y. Experimental study of needle–tissue interaction forces: effect of needle geometries, insertion methods and tissue characteristics. Journal of Biomechanics, 2014, 47(13): 3344–3353
de la Torre R A, Bachman S L, Wheeler A A, Bartow K N, Scott J S. Hemostasis and hemostatic agents in minimally invasive surgery. Surgery, 2007, 142(4): S39–S45
Balakrishnan B, Soman D, Payanam U, Laurent A, Labarre D, Jayakrishnan A. A novel injectable tissue adhesive based on oxidized dextran and chitosan. Acta Biomaterialia, 2017, 53: 343–354
Tompeck A J, Gajdhar A U R, Dowling M, Johnson S B, Barie P S, Winchell R J, King D, Scalea T M, Britt L D, Narayan M. A comprehensive review of topical hemostatic agents: the good, the bad, and the novel. Journal of Trauma and Acute Care Surgery, 2020, 88(1): e1–e21
Stauffer P R, Rossetto F, Prakash M, Neuman D G, Lee T. Phantom and animal tissues for modelling the electrical properties of human liver. International Journal of Hyperthermia, 2003, 19(1): 89–101
Carter F J, Frank T G, Davies P J, McLean D, Cuschieri A. Measurements and modelling of the compliance of human and porcine organs. Medical Image Analysis, 2001, 5(4): 231–236
Wineman A. Nonlinear viscoelastic solids—a review. Mathematics and Mechanics of Solids, 2009, 14(3): 300–366
Yang J, Yu L T, Wang L, Wang W J, Cui J W. The estimation method of friction in unconfined compression tests of liver tissue. Proceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine, 2018, 232(6): 573–587
Estermann S J, Pahr D H, Reisinger A. Hyperelastic and viscoelastic characterization of hepatic tissue under uniaxial tension in time and frequency domain. Journal of the Mechanical Behavior of Biomedical Materials, 2020, 112: 104038
Li L, Maccabi A, Abiri A, Juo Y Y, Zhang W Y, Chang Y J, Saddik G N, Jin L H, Grundfest W S, Dutson E P, Eldredge J D, Benharash P, Candler R N. Characterization of perfused and sectioned liver tissue in a full indentation cycle using a visco-hyperelastic model. Journal of the Mechanical Behavior of Biomedical Materials, 2019, 90: 591–603
Liu D, Li G Y, Su C, Zheng Y, Jiang Y X, Qian L X, Cao Y P. Effect of ligation on the viscoelastic properties of liver tissues. Journal of Biomechanics, 2018, 76: 235–240
Zheng Y, Jiang Y X, Cao Y P. A porohyperviscoelastic model for the shear wave elastography of the liver. Journal of the Mechanics and Physics of Solids, 2021, 150: 104339
Nafo W, Al-Mayah A. Measuring the hyperelastic response of porcine liver tissues in-vitro using controlled cavitation rheology. Experimental Mechanics, 2021, 61(2): 445–458
Pasyar P, Masjoodi S, Montazeriani Z, Makkiabadi B. A digital viscoelastic liver phantom for investigation of elastographic measurements. Computers in Biology and Medicine, 2020, 127: 104078
Matin Z, Moghimi Zand M, Salmani Tehrani M, Wendland B R, Dargazany R. A visco-hyperelastic constitutive model of short-and long-term viscous effects on isotropic soft tissues. Proceedings of the Institution of Mechanical Engineers, Part C: Journal of Mechanical Engineering Science, 2020, 234(1): 3–17
Zhang Y D, Li B, Yuan L P. Study on the control method and optimization experiment of prostate soft tissue puncture. IEEE Access: Practical Innovations, Open Solutions, 2020, 8: 218621–218643
Roesthuis R J, van Veen Y R J, Jahya A, Misra S. Mechanics of needle-tissue interaction. In: Proceedings of 2011 IEEE/RSJ International Conference on Intelligent Robots and Systems. San Francisco: IEEE, 2011, 2557–2563
Li A D R, Plott J, Chen L, Montgomery J S, Shih A. Needle deflection and tissue sampling length in needle biopsy. Journal of the Mechanical Behavior of Biomedical Materials, 2020, 104: 103632
Acknowledgements
This work was partially supported by Shenzhen Key Laboratory of Robotics Perception and Intelligence (Southern University of Science and Technology, China) (Grant No. ZDSYS20200810171800001).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Conflict of Interest
Authors declare no conflict of interest regarding the submitted manuscript.
Rights and permissions
About this article
Cite this article
Zhu, X., Ma, Y., Xiao, X. et al. Design and evaluation of a novel biopsy needle with hemostatic function. Front. Mech. Eng. 18, 22 (2023). https://doi.org/10.1007/s11465-022-0738-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11465-022-0738-7