Abstract
Infectious diseases cause tremendous costs of both human and economy annually. Previously, we have studied the bacterial, fungal, and allergen aerosol inactivation by direct microwave irradiation. Here, we further investigated its effects on airborne viruses. MS2 coliphage used as a human model virus was aerosolized and exposed to the direct microwave irradiation for ~2 min at three different power levels (700, 385, and 119 W). In addition to the survival rate, the viral genes before and after the microwave treatments were also examined using PCR and gel electrophoresis. Direct exposure of airborne MS2 viruses to the microwave irradiation at 700 W for less than 2 min was shown to result in more than 90 % inactivation efficiency, about 65 % at medium power level (385 W), and 50 % at the lowest level (119 W). The aerosol inactivation rate followed a linear relationship with the microwave exposure time (R 2 = 0.9889). Scanning electron images revealed visible damages to the viral surface after the exposure. Damages were also observed to the viral RNA genes coding for coat proteins, among which the A protein gene was completely destroyed. This study demonstrated that even without the filtration the direct microwave irradiation could also achieve rapid inactivation of viral aerosols. The information obtained can provide useful guidance on the development of microwave-based viral threat mitigation solutions in a closed or semi-closed space.
Similar content being viewed by others
1 Introduction
Every year, respiratory infections result in a tremendous cost of both human life and economy throughout the world [1]. As well known with the seasonal influenza, numerous studies also support that the large scale respiratory disease pandemics, e.g., SARS and H1N1 outbreaks in 2003 and 2009, respectively, are facilitated through airborne transmission of the viral agents [2–5]. Recent evidences also suggest that genetically modified H5N1 strain can be also efficiently transmitted through air among ferrets [6, 7]. The airborne transmission of infectious virus is further strengthened by the fact that exhaled breath from a person with flu symptoms was found to contain large amount influenza viruses [8–10]. Recently, SARS alike virus emerges, and it already claimed five lives [11]. In April, 2013, bird flu virus H7N9 was first found to infect humans with total 91 confirmed cases including close to 20 deaths as of this writing in several provinces of China [12]. Worldwide scientists are now afraid that the virus could further mutate to cause human-to-human transmission, triggering another deadly influenza pandemic. Such a situation is further complicated by the potential threat from bioterrorism.
Accordingly, effective inhalation protective measure or inactivation of airborne viruses plays an important role in mitigating the human-to-human infectious disease threat. In general practice, a mask is used for a person to shield from virus infection or to protect those healthy ones. To some extent, this is the easiest approach that can help among those existing technologies. However, the practice does have its limitations. For example, the repelled viruses are attached to the outer surface of the mask, and might remain infective for a prolonged time period, thus presenting a source of infection. Even for the professional grade, the medical masks might not completely filter out the viruses of around 100 nm in diameter. In a recent study, the percentage of infection for nurses wearing surgical mask or N95 respirator when providing health care was found more than 20 % [13]. In addition to the medical risk, the use of a respirator, especially a professional grade, is costly because it is less likely to be re-used due to the concern of cross infection. In an influenza pandemic, the respirator mask might be out of supply, leaving millions unprotected. Another disadvantage of using a respirator is the breathability of the mask while protecting against viral pathogens. Recent studies suggest that use of carbon nanotube membrane as a potential mask could not only filter out the biologic agents, but is also able to kill those trapped [14, 15]. Importantly, a carbon nanotube fabric respirator has a high breathability, however, such a real application is many years away.
On the other hand, numerous studies were carried out to inactivate airborne biologic agents, thus providing safe air. Among other technologies including UV, electrostatic means [16, 17], and ozone [18], microwave irradiation also recently attracts attention in inactivating bioaerosols including airborne MS2 viruses [19–22]. Some of these studies combined the filtration with the microwave irradiation to achieve airborne virus inactivation [21], while our recent studies demonstrated that even without the filtration direct microwave irradiation on the airborne bacterial and fungal aerosols can result in their significant inactivation as a result of damages of membrane and internal structures [19, 20]. The microwave oven is widely used in a household throughout the world, thus potential applications of microwave irradiation as a disinfection method can be easily introduced. Effective sterilization of re-circulated air can greatly reduce the airborne transmission of infectious agents especially in an air confined space such as a submarine.
While inactivation efficiency about virus inactivation using microwave irradiation coupled with filtration is available, however, the use of direct microwave irradiation on viruses in airborne state has not been reported. Viruses are generally very small with a size of 100 nm or so, thus they might not be captured by the filter. In addition, the relevant virus inactivation mechanisms remain un-investigated either. Here, we used MS2 virus as a model virus for humans, and subjected the airborne viruses to direct microwave irradiation with three different power levels (700, 385, and 119 W) for about 2 min. The inactivation rate of the virus was studied using plaque forming unit (PFU) method which utilizes the Escherichia coli as the viral host. To study the mechanisms, water-borne MS2 viruses were also subjected to the microwave irradiation, and RNA genes codling for the viral surface proteins such as the A protein, the capsid protein, the replicase protein, and the lysis protein before and after the microwave irradiation were studied using PCR and gel electrophoresis.
2 Materials and methods
2.1 Preparation of MS2
In this work, MS2 bacteriophage (ATCC15597-B1) was chosen as a human model virus. The MS2 genome is one of the smallest known, totaling 3,569 nucleotides [23]. The genome encodes just four proteins: the maturation protein (A-protein), the lysis protein, the capsid protein, and the replicase protein [24]. Here, the double-top agar layer plaque technique described previously [25] was employed for MS2 propagation using Escherichia coli (ATCC 15597) as the host. E. coli was first cultured for 18–24 h in a tryptic soy broth (TSB; Difco, Detroit, MI, USA) and then transferred to fresh TSB and grown to a mid-log phase for 6 h at 37 °C. Stock MS2 was diluted in freshly purified water (Milli-Q, Millipore, Billerica, and MA, USA) to a final concentration of around 106 PFU/mL. Next, the E. coli suspension (0.9 mL) and phage dilution (0.1 mL) were mixed in 3 mL of soft overlay agar and poured onto pre-solidified trypticase soy agar (TSA, 0.5 % agar; Difco, Detroit, MI, USA) Petri dishes. Sterile water (Milli-Q, Millipore, Billerica, and MA, USA) was then added to the Petri dishes, which resulted in confluent plaques after incubation for 24 h at 37 °C. The purified water containing the MS2 phages was then decanted into a sterile tube (Corning, USA) and centrifuged at 5,000 g for 30 min to remove bacterial and agar debris. The phage pellet was resuspended in sterile water and stored at 4 °C. Fresh phage stock was prepared in this manner prior to each experiment.
2.2 Sampler used
In this study, we used the BioSampler (SKC Inc., Eighty-Four, PA, USA) to collect airborne MS2 virus. The BioSampler, collecting bioaerosols directly into liquids through both impaction and centrifugation forces, has been widely used as a standard liquid sampler for bioaerosol sampling. In this study, 20 mL deionized (DI) water (Millipore) and a sampling flow rate of 12.5 L/min (an optimal flow rate) (SKC) were used for the BioSampler to collect airborne MS2 viruses. The flow rate for the sampler was calibrated using a mini-Buck calibrator (A.P. Buck, Inc., Orlando, FL, USA) before use. For the BioSampler, the sampling time is suggested to be limited to 15–30 min, above which the collection efficiency decreases [26]. Accordingly, 20 min sampling time was used in this study.
2.3 Experimental procedures
2.3.1 Inactivation of airborne MS2
The experimental setup used in this work is shown in Fig. 1. Using the system, MS2 viruses were continuously being aerosolized and exposed to microwave irradiation at different power levels. As observed in the figure, the experimental setup is composed of three major parts: an aerosol generator (Collison nebulizer, BGI Inc., Waltham, MA, USA), a modified microwave oven, and a bioaerosol collector (BioSampler, SKC Inc., Eighty Four, PA). A commercial microwave oven (Midea Inc., Foshan, Guangdong Province, China) was modified to operate with one bioaerosol inlet and one sampling outlet of 1.5 cm in diameter. As described in our previous study [19], the inlet and outlet were drilled from the thin back of the microwave oven, and it has a total of 21 Liter air space inside. Before the experiments, the MS2 bacteriophages were suspended in water and continuously being aerosolized by a Collision nebulizer (BGI) which was operated at a flow rate of Q neb = 2.5 L/min with an operating pressure of about 50 psi. The viral suspensions in the aerosolization vessel of the Collison nebulizer were from the same microbial suspensions both for the control and exposed experiments. The resulting viral aerosols were dried and diluted by an additional pure N2 airflow, Q dry, about 13 L/min. The bioaerosol flow was further drawn into the exposure chamber with the modified microwave oven, where MS2 virus aerosols were exposed to the microwave irradiation (2,450 MHz) at different output powers (700, 385, and 119 W), which are pre-set on the modified microwave oven aforementioned. The control and exposed viral aerosol samples were collected using the BioSampler continuously for 20 min at a sampling flow rate of 12.5 L/min. The travel speed of MS2 coliphage aerosol entering and leaving the microwave exposure chamber can be estimated based on the sampling flow rate (12.5 L/min) and the diameter of the inlet or outlet. By calculation, the entering or leaving speed was 118 cm/s, and the residence time or exposure time inside the microwave exposure chamber (total 21 L) was about 1.7 min. If assuming the microwave chamber is a standard cube, the travel speed of MS2 virus aerosol inside the chamber was about 16.4 cm/s. The viral aerosol air samples with and without the microwave irradiation treatment were cultured for 24 h at 37 °C using the double-top agar layer plaque technique mentioned above. At least three independent experiments and each with three replicates were performed for each experimental condition in this study.
PFUs were manually counted and MS2 viral aerosol concentrations were then calculated as PFU/m3, and the survival rate was calculated using the equation below
where S is the survival rate, PFUExposed is the culturable viral aerosol concentration after the microwave irradiation treatment, and PFUControl is the culturable viral aerosol concentration without the microwave treatment under the same conditions.
2.3.2 Inactivation of waterborne MS2
In this work, to investigate the inactivation mechanisms, liquid-borne MS2 bacteriophage (airborne concentration level was too low to be used for studying inactivation mechanisms using SEM) was also exposed to the microwave irradiation. The prepared MS2 bacteriophage was serially diluted, and 10−1 and 10−2 dilution factors were used in this study. When performing the experiments, 200 μL of microbial suspension of different dilutions was added into the wells of a 96-well plate with three replicates. The wells were sealed by parafilm (Pechiney, Plastic Packaging, Menasha, WI, 54952) to minimize the liquid evaporation. The microbial liquid suspensions were then exposed to the microwave irradiation at varying output powers (700, 385, and 119 W) for different exposure time: 2, 3, and 5 min. Similar to airborne exposure, for each experimental condition, the experiments with both exposed and control were independently conducted three times with total nine replicates.
2.3.3 Analysis of effects of microwave irradiation on water-borne viral surface protein genes
In this work, amplifications for viral RNA genes coding for the four proteins such as the A protein, the capsid protein, the lysis protein, and the replicase protein before and after the microwave exposure in liquid phase were also conducted in this study. Gel electrophoresis combined with reverse transcription polymerase chain reaction (RT-PCR) was applied to analyze the effects of microwave irradiation on these RNA genes. The bacteriophage MS2 was extracted for RNA. The whole process was performed according to the manufacturer’s guidelines specified in the virus RNA Extraction Kit (Tiangen Biotech, Inc., Beijing, China). First, 140 μL of sample suspension was added to 1.5 mL tube in which 560 μL carrier RNA solution was added in advance. The suspension was vortexed for 15 s to release the RNA, and then incubated at room temperature for 5 min. The 560 μL absolute ethyl alcohol was added to the solution after centrifugation for several seconds. Second, the solution was transferred to RNase-free adsorption column which was placed in a collection tube and then centrifuged at 8,000 r/min for 1 min. After the liquid in the collection tube was removed, 500 μL buffer solution was added to the suspension and mixed well, in order to completely remove the remaining protein. The samples were again centrifuged at 12,000 r/min for 3 min. Finally, 60 μL supernatant of each sample was saved and stored at −20 °C for RT-PCR. All manipulations of the samples were performed in the biologic safety cabinet as discussed in our previous study [19].
For amplifying viral surface protein genes, the cDNA, the forward primer, and the reverse primer shown in Table 1, which were designed in previous studies [27, 28], were used here. The RT-PCR cycle conditions were 50 °C for 30 min (reverse transcription), 94 °C for 2 min, 40 cycles of (94 °C for 60 s, 55 °C for 60 s and 65 °C for 2 min), and 65 °C for 10 min. DI water was used as the negative control in the RT-PCR experiments. Gel electrophoresis was performed with the Sub-Cell GT instruments (Bio-Rad, Hercules, CA, USA) according to the manufacturer’s instructions. In details, approximately 20 μL of PCR product was transferred to each well of 3 % agarose gels. The electrophoresis was performed for 100 min at a constant voltage of 60 V. After the electrophoresis, gels were stained with GelRed solution (10,000× diluted with DI water) (Biotium, Hayward, CA) and photographed (Molecular Imager Gel Doc XR System, Bio-Rad) under ultraviolet lamp at the wavelength of 254 nm.
3 Statistical analysis
The experimental data were analyzed statistically by one-way ANOVA tests and linear regression analysis. P values less than 0.05 indicated a statistically significant difference.
4 Results
In our study, we used a duty cycle microwave oven (being used in many households in China), and the unit works for different times at different power levels: full cycle of 30 s for high power (700 W), 16.5 s per cycle for medium power (385 W), and 5.1 s per cycle for low power (119 W). For our experiments, we operated the microwave unit continuously, however, when low and medium power levels were applied the microwave unit irradiates periodically per a duty cycle. Based on its duty time per cycle for different power levels, the microwave exposure time can be calculated. For high power, the microwave unit works at full cycle without a break, thus the exposure time of bioaerosols was their residence time in the exposure chamber, which was 100.8 s (3.36 duty cycles). The situation was different for medium and low power since the unit works periodically under such conditions. For medium power (385 W), the exposure time was 16.5 s per duty cycle, so for a particular viral aerosol its microwave exposure time was 55.4 s. For low power (119 W), its microwave exposure time was 17.1 s. For high power, the average bioaerosol exposure time was 1.8 times medium power, and about 6 times of low power. The different exposure time was taken into account of the three power levels used in this work.
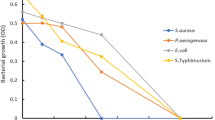
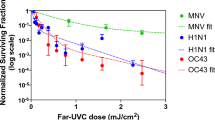
Our airborne exposure experiments shown in Fig. 2 indicated that the survival rates of MS2 virus aerosols decreased with increasing power levels. At high power, the survival rate was shown to be about 10 %, further increased to 35 % and 50 % at medium and low power levels, respectively. ANOVA analysis indicated that there was a statistically significant effect of the power level on the MS2 survival rates (P < 0.0001). Different from previous work with allergens [29], the virus aerosol inactivation rate observed here followed a linear relationship with the microwave exposure time (R 2 = 0.9889). To further investigate the microwave irradiation mechanism, the inactivation of liquid-borne MS2 viruses was also performed, and the results were shown in Fig. 3. As observed in the figure, for a particular exposure time increasing power level also resulted in higher inactivation rates of MS2 (P < 0.0084). For low and medium power levels, increasing exposure time was also found to lead to increasing inactivation rates of MS2 as observed in Fig. 3 (P = 0.000853 and P = 0.001181, respectively). However, for high power level (700 W), increasing exposure time did not significantly increase the inactivation efficiency (P = 0.619). Figure 4 shows the SEM images of microwave irradiated liquid-borne MS2 for 1 min and those of controls. As seen from the figures, compared to the controls after the microwave exposure the surfaces of MS2 viruses were found to be ruptured. Figure 5 shows the gel electrophoresis of viral genes coding for surface proteins of MS2 virus: the A protein, the capsid protein, the replicase protein, and the lysis protein with and without the microwave irradiation. As observed from the figure, for the A protein gene with a target band of 934 bp after the microwave exposure with the high power level the gel band disappeared, while for the medium and low power levels the bands become less visible or the band intensity decreased compared to that without the microwave exposure. For the capsid protein (160 bp), the lysis protein (114 bp), and the replicase protein genes (937 bp), the relevant gel bands were still visible regardless of the power levels, however, their intensities decreased with increasing power level as shown in Fig. 5. These results suggest that direct microwave irradiation not only caused viral surface rupture, but also damaged the RNA genes.
Previously, we have shown that use of microwave irradiation can achieve high inactivation efficiencies for bacterial and fungal aerosols, and microbial membrane and internal structural damages were observed [19, 20]. The results from this work further confirm that microwave irradiation based method can be also used to kill airborne viruses with high efficiency. The survival rate of MS2 virus upon microwave irradiation is a function of both exposure time and microwave power level. At high power (700 W), the inactivation efficiency for airborne MS2 viruses was shown up to 90 % for about 1.7 min exposure. From SEM images, we can see that the inactivation of MS2 viruses was in part due to the rupture of the viral surface. On the other hand, our data shown in Fig. 5 indicated at high power (700 W) the gene coding for the A protein present on the viral coat was completely destroyed. The main function of the A protein is to identify the host, thus allowing the virus to replicate itself and to cause an infection. Accordingly, any damages to the A protein gene would result in the loss of the viral ability to express the protein and thus its ability to identify the host and further replicate. Compared to the A protein gene, the capsid, the replicase, and the lysis protein genes were damaged to a lesser degree by the microwave irradiation as observed in Fig. 5. Nonetheless, these genes coding for the three proteins also suffered certain degree of damages as the band intensities generally decreased when microwave irradiation was applied. A previous study showed that the MS2 virus has only one copy of A protein gene and 180 copies of the coat protein [30]. The observed differences in related gene damages here are interesting, and it might be due to their different structures and arrangements which, however, merit further investigation. Compared to other studies, this work provided information about the effects of in situ microwave irradiation on airborne viral aerosols and investigated the relevant inactivation mechanisms.
5 Discussion
MS2 viruses were used as a viral model to test the inactivation efficiencies of proposed engineering solutions in many studies [18, 21, 30, 31], and was shown to be better than coliphage Qβ as a viral indicator [32]. Recently, microwave irradiation was applied to inactivate viruses including MS2 and H1N1 viruses manually spiked or collected on filtering facepiece respirators [33] and in-flight or offline filter [21, 22]. These microwave inactivation studies showed remarkable killing rates, sometimes up to 4 log for H1N1 viruses [33]. It was shown that the filter surface-borne MS2 virus inactivation by microwave irradiation depended on the power level, application time, and the relative humidity level under certain conditions [21]. Likewise, this work also found that the MS2 viral inactivation was a function of power level and irradiation time. SEM images also revealed visible damages to the MS2 viral surface. Different from previous investigations, this work presented the results about the MS2 virus inactivation by direct microwave irradiation in airborne state. Such information is important since filtration itself cannot filter out all viruses. Use of filtration would cause pressure drop in the exposure chamber, thus requiring more external power. Based on information obtained from this work and previous studies, microwave irradiation can find its applications to safeguard air in semi- or closed-indoor settings.
Influenza viruses were detected from human exhaled breath in numerous studies [8–10]. When exhaled, viruses could remain airborne for a prolonged time period, yet its ability to cause further infections depends on many factors such as its infectivity, airborne transport, environmental matrix, and host immune system. Numerous studies support that airborne transmission of infectious agents among humans is certain, and mankind frequently faces the emerging infectious disease threats such as H1N1 and H7N9. Effective engineering solutions for protecting breathing air might go a long way toward human battle with emerging infectious disease threats such as SARS, H1N1, H5N7, and H7N9. Well-designed protocol could secure the safety of the recirculated air inside an office building or a confined air space, thus minimizing the biologic contamination and infectious disease spread. Many technologies are already there, and the important adaptation is to minimize the environmental impact and power consumption.
In this study, only human model virus was tested with microwave irradiation, and its efficacies for inactivation of human viruses such as H1N1 and H3N2 should be evaluated in the future. In this work, we did not intend to quantify the amount of genes; instead we wanted to qualitatively assess possible gene damages. In theory, one can use qPCR to quantify the amount of certain genes, however, when PCR products need to be further analyzed using gel electrophoresis as done in this work PCR is typically employed. In addition, the observed MS2 virus killing or damage by microwave exposure might be also attributed to the non-thermal effects of microwave irradiation as discussed for bacterial aerosol inactivation [19, 20]. Here, the microwave power density tested was about 900 mW/cm2, which is about 100 times that of a recommended safe exposure limit 10 mW/cm2 commonly described to allow a non-thermal effect to occur. Thus, the developed technique here might be only applicable for treating mechanically ventilated air in a closed or semi-closed enclosing, and cannot be applied to directly irradiate room air when occupants are present. This drawback has also been discussed in our previous work that used the microwave irradiation to treat airborne allergens [29].
6 Conclusions
This work provided an effective engineering solution for safeguarding breathing air by applying direct microwave irradiation to virus laden air. Results revealed that MS2 virus inactivation rate was more than 90 % after less than 2 min exposure at a microwave power level of 700 W. It was also found that for microwave irradiated MS2 viruses severe damages occurred to both viral surface and the viral RNA genes coding for surface proteins, especially the A protein. Damages to the protein genes could cause the viruses to lose the ability to express the related protein and thus the ability to identify the host and mount an infection. In response to rapid viral mutation and re-emerging infectious agents, better engineering solutions should be further developed.
References
World Health Organization (2013). Influenza (seasonal) 2009. http://www.who.int/mediacentre/factsheets/fs211/en/index.html. Accessed 19 Apr 2013
Yu ITS, Li Y, Wong TW et al (2004) Evidence of airborne transmission of the severe acute respiratory syndrome virus. N Engl J Med 351:1731–1739
Majic Z, Jukic I, Pavlin S (2009) Air transport and logistics in pandemic outbreak of influenza A (H1N1) virus. Promet Traffic Transp 21:425–434
Baker MG, Thornley CN, Mills C et al (2010) Transmission of pandemic A/H1N1 2009 influenza on passenger aircraft: retrospective cohort study. BMJ 340:c2424
Tellier R (2009) Aerosol transmission of influenza A virus: a review of new studies. J R Soc Interface 6:S783–S790
Herfst S, Schrauwen EJ, Linster M et al (2012) Airborne transmission of influenza A/H5N1 virus between ferrets. Science 336:1534–1541
Russell CA, Fonville JM, Brown AE et al (2012) The potential for respiratory droplet-transmissible A/H5N1 influenza virus to evolve in a mammalian host. Science 336:1541–1547
Xu Z, Shen F, Li X et al (2012) Molecular and microscopic analysis of bacteria and viruses in exhaled breath collected using a simple impaction and condensing method. PLoS ONE 7:e41137
Fabian P, McDevitt JJ, DeHaan WH et al (2008) Influenza virus in human exhaled breath: an observational study. PLoS ONE 3:e2691
Noti JD, Lindsley WG, Blachere FM et al (2012) Detection of infectious influenza virus in cough aerosols generated in a simulated patient examination room. Clin Infect Dis 54:1569–1577
Lightfoot N, Rweyemamu M, Heymann DL (2013) Preparing for the next pandemic. BMJ 346:f364
World Health Organization (2013) Human infection with avian influenza A (H7N9) virus in China: update, http://www.who.int/csr/don/2013_04_19/en/index.html. Accessed 19 Apr 2013
Loeb M, Dafoe N, Mahony J et al (2009) Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA 302:1865–1871
Guan T, Yao M (2010) Use of carbon nanotube filter in removing bioaerosols. J Aerosol Sci 6:611–620
Xu Z, Yao M (2011) Effects of carbon nanotube filter on the culturability and diversity of environmental bioaerosols. J Aerosol Sci 42:387–396
Jensen MM (1964) Inactivation of airborne viruses by ultraviolet irradiation. J Appl Microbiol 12:418–420
Yao M, Mainelis G, An HR (2005) Inactivation of microorganisms using electrostatic fields. Environ Sci Technol 39:3338–3344
Tseng CC, Li CS (2006) Ozone for inactivation of aerosolized bacteriophages. Aerosol Sci Technol 40:683–689
Wu Y, Yao M (2010) Inactivation of bacteria and fungus aerosols using microwave irradiation. J Aerosol Sci 41:682–693
Wu Y, Yao M (2011) Effects of microwave irradiation on concentration, diversity and gene mutation of culturable airborne microorganisms of inhalable sizes in different environments. J Aerosol Sci 42:800–810
Woo MH, Grippin A, Wu CY et al (2012) Microwave-irradiation-assisted HVAC filtration for inactivation of viral aerosols. Aerosol Air Qual Res 12:295–303
Zhang Q, Damit B, Welch J et al (2010) Microwave assisted nanofibrous air filtration for disinfection of bioaerosols. J Aerosol Sci 41:880–888
Fiers W, Contreras R, Duerinck F et al (1976) Complete nucleotide sequence of bacteriophage MS2 RNA: primary and secondary structure of the replicase gene. Nature 260:500–507
van Duin J, Tsareva N (2006) Single-stranded RNA phages Chapter 15. In: Calendar RL (ed) The Bacteriophages, 2nd edn. Oxford University Press, Oxford, pp 175–196
Adams MH (1959) Bacteriophages. Interscience Publishers Inc., New York
Lin X, Reponen TA, Willeke K et al (1999) Long-term sampling of airborne bacteria and fungi into a non-evaporating liquid. Atmos Environ 33:4291–4298
Sun W (2007) Preliminary study on inactivation mechanism and effectiveness of sodium dichlotoisocyanusale to bacteriophage MS2. Master degree thesis of Sichuan University, 2007 (in Chinese)
O’Connell KP, Bucher JR, Anderson PE et al (2006) Real-time fluorogenic reverse transcription-PCR assays for detection of bacteriophage MS2. Appl Environ Microbiol 72:478–483
Wu Y, Yao M (2013) Control of airborne and liquid-borne fungal and pet allergens using microwave irradiation. J Occup Environ Hyg 10:547–555
Valegård K, Lilias L, Fridborg K et al (1990) The three-dimensional structure of the bacterial virus MS2. Nature 345:36–41
Griffiths WD, Bennett A, Speight S et al (2005) Determining the performance of a commercial air purification system for reducing airborne contamination using model micro-organisms: a new test methodology. J Hosp Infect 61:242–247
Tseng C-C, Li C-S (2005) Inactivation of virus-containing aerosols by ultraviolet germicidal irradiation. Aerosol Sci Technol 39:1136–1142
Feng YY, Ong SL, Hu JY et al (2003) Effects of pH and temperature on the survival of coliphages MS2 and Qb. J Ind Microbiol Biotechnol 30:549–552
Heimbuch B, Wallace W, Kinney K et al (2010) A pandemic influenza preparedness study: use of energetic methods to decontaminate filtering facepiece respirators contaminated with H1N1 aerosols and droplets. Am J Infect Control 39:1–9
Acknowledgments
This work was supported by the National Natural Science Foundation of China (21077005, 41121004).
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Wu, Y., Yao, M. In situ airborne virus inactivation by microwave irradiation. Chin. Sci. Bull. 59, 1438–1445 (2014). https://doi.org/10.1007/s11434-014-0171-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11434-014-0171-3