Abstract
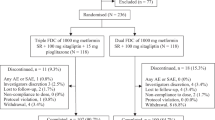
Despite the current guideline’s recommendation of a timely stepwise intensification therapy, the “clinical inertia”, termed as the delayed treatment intensification, commonly exists in the real world, which may be partly due to the relatively little substantial evidence and no clear consensus regarding the efficacy and safety of triple oral agents in patients inadequately controlled with dual therapy. In this clinical trial performed in 237 centers in China, 5,535 type 2 diabetic patients inadequately controlled by previous therapies were treated with a stable metformin/sitagliptin dual therapy for 20 weeks. The patients who did not reach the glycated hemoglobin A1c (HbA1c) goal were then further randomized into glimepiride, gliclazide, repaglinide, or acarbose group for an additional 24-week triple therapy. A mean HbA1c reduction of 0.85% was observed when sitagliptin was added to the patients inadequately controlled with metformin in 16 weeks. Further HbA1c reductions in the 24-week triple therapy stage were 0.65% in glimepiride group, 0.70% in gliclazide group, 0.61% in repaglinide group, and 0.45% in acarbose group. The non-inferiority criterion for primary hypotheses was met for gliclazide and repaglinide, but not for acarbose, compared with glimepiride, when added to metformin/sitagliptin dual therapy. The incidences of adverse events (AEs) were 29.2% in the dual therapy stage and 30.3% in the triple therapy stage. Metformin/sitagliptin as baseline therapy, with the addition of a third oral antihyperglycemic agent, including glimepiride, gliclazide, repaglinide, or acarbose, was effective, safe and well-tolerated for achieving an HbA1c <7.0% goal in type 2 diabetic patients inadequately controlled with previous therapies. The timely augmentation of up to three oral antihyperglycemic agents is valid and of important clinical benefit to prevent patients from exposure to unnecessarily prolonged hyperglycemia.
Similar content being viewed by others
References
American Diabetes Association, (2017). 8. Pharmacologic Approaches to Glycemic Treatment. Diabetes Care 40, S64–S74.
Barnett, A.H., Charbonnel, B., Moses, R.G., and Kalra, S. (2015). Dipeptidyl peptidase-4 inhibitors in triple oral therapy regimens in patients with type 2 diabetes mellitus. Curr Med Res Opin 31, 1919–1931.
Bi, Y., Zeng, L., Zhu, D., Yan, J., Zhang, Y., Tong, G., Mu, P., Shen, S., Hu, Y., Yu, Q., Liang, H., and Weng, J. (2012). Aßsociation of ß-cell function and insulin sensitivity with fasting and 2-h plasma glucose in a large Chinese population. Diabetes Obes Metab 14, 174–180.
Chan, J.C.N., Aschner, P., Owens, D.R., Picard, S., Vincent, M., Dain, M.P., Pilorget, V., Loizeau, V., Echtay, A., and Fonseca, V. (2015). Triple combination of insulin glargine, sitagliptin and metformin in type 2 diabetes: the EASIE post-hoc analysis and extension trial. J Diabetes Complications 29, 134–141.
Chan, S.P., and Colagiuri, S. (2015). Systematic review and meta-analysis of the efficacy and hypoglycemic safety of gliclazide versus other insulinotropic agents. Diabetes Res Clin Pract 110, 75–81.
DeFronzo, R.A., Barzilai, N., and Simonson, D.C. (1991). Mechanism of metformin action in obese and lean noninsulin-dependent diabetic subjects. J Clin Endocrinol Metab 73, 1294–1301.
Downes, M.J., Bettington, E.K., Gunton, J.E., and Turkstra, E. (2015). Triple therapy in type 2 diabetes; a systematic review and network meta-analysis. PeerJ 3, e1461.
Drucker, D.J., and Nauck, M.A. (2006). The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet 368, 1696–1705.
Global Burden of Disease Study 2013 Collaborators. (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386: 743–800.
Hampp, C., Borders-Hemphill, V., Moeny, D.G., and Wysowski, D.K. (2014). Use of antidiabetic drugs in the U.S., 2003–2012. Dia Care 37, 1367–1374.
Hermansen, K., Kipnes, M., Luo, E., Fanurik, D., Khatami, H., Stein, P., and Stein, P. (2007). Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, in patients with type 2 diabetes mellitus inadequately controlled on glimepiride alone or on glimepiride and metformin. Diabetes Obes Metab 9, 733–745.
Holman, R.R., Paul, S.K., Bethel, M.A., Matthews, D.R., and Neil, H.A.W. (2008). 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 359, 1577–1589.
Hong, J., Gu, W.Q., Zhang, Y.F., Yang, Y.S., Shen, C.F., Xu, M., Li, X.Y., Wang, W.Q., and Ning, G. (2007). The interplay of insulin resistance and ß-cell dysfunction involves the development of type 2 diabetes in Chinese obeses. Endocrine 31, 93–99.
International Diabetes Federation. (2015). International Diabetes Federation Diabetes Atlas, 7th ed. in press.
Inzucchi, S.E., Bergenstal, R.M., Buse, J.B., Diamant, M., Ferrannini, E., Nauck, M., Peters, A.L., Tsapas, A., Wender, R., and Matthews, D.R. (2015). Management of hyperglycaemia in type 2 diabetes, 2015: a patient- centred approach. Update to a Position Statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia 58, 429–442.
Ji, L., Hu, D., Pan, C., Weng, J., Huo, Y., Ma, C., Mu, Y., Hao, C., Ji, Q., Ran, X., Su, B., Zhuo, H., Fox, K.A.A., Weber, M., Zhang, D., Zhang, D., and Zhang, D. (2013). Primacy of the 3B approach to control risk factors for cardiovascular disease in type 2 diabetes patients.
Am J Med 126, 925.e11–925.e22.
Ji, L.N., Lu, J.M., Guo, X.H., Yang, W.Y., Weng, J.P., Jia, W.P., Zou, D.J., Zhou, Z.G., Yu, D.M., Liu, J., Shan, Z.Y., Yang, Y.Z., Hu, R.M., Zhu, D.L., Yang, L.Y., Chen, L., Zhao, Z.G., Li, Q.F., Tian, H.M., Ji, Q.H., Liu, J., Ge, J.P., Shi, L.X., and Xu, Y.C. (2013). Glycemic control among patients in China with type 2 diabetes mellitus receiving oral drugs or injectables. BMC Public Health 13, 602.
Kahn, S.E., Cooper, M.E., and Del Prato, S. (2014). Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet 383, 1068–1083.
Karagiannis, T., Paschos, P., Paletas, K., Matthews, D.R., and Tsapas, A. (2012). Dipeptidyl peptidase-4 inhibitors for treatment of type 2 diabetes mellitus in the clinical setting: systematic review and meta-analysis. BMJ 344, e1369–e1369.
Khunti, K., Wolden, M.L., Thorsted, B.L., Andersen, M., and Davies, M.J. (2013). Clinical inertia in people with type 2 diabetes: a retrospective cohort study of more than 80,000 people. Diabetes Care 36, 3411–3417.
Lancet. (2014). Principles to guide type 2 diabetes care in the USA. Lancet 384, 1822.
Levin, P.A. (2016). Practical combination therapy based on pathophysiology of type 2 diabetes. DMSO Volume 9, 355–369.
Lin, J.D., Chen, Y.L., Hsu, C.H., Wu, C.Z., Hsieh, A.T., Hsieh, C.H., Chang, J.B., Liang, Y.J., and Pei, D. (2013). Beta-cell function and insulin sensitivity at various degrees of glucose tolerance in Chinese subjects. Diabetes Res Clin Pract 100, 391–397.
Liu, S.C., Chien, K.L., Wang, C.H., Chen, W.C., and Leung, C.H. (2013). Efficacy and safety of adding pioglitazone or sitagliptin to patients with type 2 diabetes insufficiently controlled with metformin and a sulfonylurea. Endocr Pract 19, 980–988.
McIntosh B., Cameron C., Singh S.R., Yu C., Dolovich L., Houlden R. (2012). Choice of therapy in patients with type 2 diabetes inadequately controlled with metformin and a sulphonylurea: a systematic review and mixed-treatment comparison meta-analysis. Open Med 6: e62–e74.
Moses, R.G., Kalra, S., Brook, D., Sockler, J., Monyak, J., Visvanathan, J., Montanaro, M., and Fisher, S.A. (2014). A randomized controlled trial of the efficacy and safety of saxagliptin as add-on therapy in patients with type 2 diabetes and inadequate glycaemic control on metformin plus a sulphonylurea. Diabetes Obes Metab 16, 443–450.
National Institute for Care and Health Excellence. (2015). Type 2 Diabetes in Adults: Management. (London: National Institute for Health and Care Excellence (UK)).
Ng, C.J., Lai, P.S.M., Lee, Y.K., Azmi, S.A., and Teo, C.H. (2015). Barriers and facilitators to starting insulin in patients with type 2 diabetes: a systematic review. Int J Clin Pract 69, 1050–1070.
Owens, D.R., Swallow, R., Dugi, K.A., and Woerle, H.J. (2011). Efficacy and safety of linagliptin in persons with type 2 diabetes inadequately controlled by a combination of metformin and sulphonylurea: a 24-week randomized study1. Diabet Med 28, 1352–1361.
Peyrot, M., Rubin, R.R., Lauritzen, T., Skovlund, S.E., Snoek, F.J., Matthews, D.R., Landgraf, R., and Kleinebreil, L. (2005). Resistance to insulin therapy among patients and providers: results of the cross-national diabetes attitudes, wishes, and needs (DAWN) study. Diabetes Care 28, 2673–2679.
Phung, O.J., Scholle, J.M., Talwar, M., and Coleman, C.I. (2010). Effect of noninsulin antidiabetic drugs added to metformin therapy on glycemic control, weight gain, and hypoglycemia in type 2 diabetes. JAMA 303, 1410–1418.
Scheen, A.J. (2015). A review of gliptins for 2014. Expert Opin Pharmacother 16, 43–62.
Schernthaner, G., Grimaldi, A., Di Mario, U., Drzewoski, J., Kempler, P., Kvapil, M., Novials, A., Rottiers, R., Rutten, G.E.H.M., and Shaw, K.M. (2004). GUIDE study: double-blind comparison of once-daily gliclazide MR and glimepiride in type 2 diabetic patients. Eur J Clin Invest 34, 535–542.
UK Prospective Diabetes Study (UKPDS) Group. (1998). Intensive bloodglucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352: 837–853.
Weng, J., Ji, L., Jia, W., Lu, J., Zhou, Z., Zou, D., Zhu, D., Chen, L., Chen, L., Guo, L., Guo, X., Ji, Q., Li, Q., Li, X., Liu, J., Ran, X., Shan, Z., Shi, L., Song, G., Yang, L., Yang, Y., Yang, W., and Yang, W. (2016). Standards of care for type 2 diabetes in China. Diabetes Metab Res Rev 32, 442–458.
Xiao, J., Weng, J., Ji, L., Jia, W., Lu, J., Shan, Z., Liu, J., Tian, H., Ji, Q., Yang, Z., Yang, W., and Yang, W. (2014). Worse pancreatic ß-cell function and better insulin sensitivity in older Chinese without diabetes. J Gerontol A Biol Sci Med Sci 69, 463–470.
Xu, Y., Wang, L., He, J., Bi, Y., Li, M., Wang, T., Wang, L., Jiang, Y., Dai, M., Lu, J., Xu, M., Li, Y., Hu, N., Li, J., Mi, S., Chen, C.S., Li, G., Mu, Y., Zhao, J., Kong, L., Chen, J., Lai, S., Wang, W., Zhao, W., Ning, G., and Ning, G. (2013). Prevalence and control of diabetes in Chinese adults. JAMA 310, 948–959.
Acknowledgements
We acknowledge the Chinese Medical Association for overseeing the ethical obligations of this study and for its kind support in communication with all the participating 237 centers, and Sun Yat-sen University for providing good clinical practice training to all the investigators. We would like to thank Prof. John B. Buse from University of North Carolina School of Medicine, USA for his constructive discussion of the manuscript preparation, and thank Prof. Rury R. Holman from University of Oxford, Oxford, United Kingdom for kind advice concerning trial conduct and constructive discussions with respect to the study results. The authors thank Zengyu Wen from MacroStat for his statistical assistance of the current work, and are grateful to the patients enrolled and the investigators participating in this study for their dedication to the study (the list seen in Text S3 in Supporting Information).This work was supported by Merck & Co., Inc., Kenilworth, NJ, the 5010 Project of Sun Yat-sen University, and Program for Changjiang Scholars and Innovative Research Team in University (to Jianping Weng).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Contributed equally to this work
Prof. Jianping Weng is a professor of the Department of Endocrinology at the Third Affiliated Hospital, Sun Yat-sen University in Guangdong, China. He is the director of Guangdong Provincial Key Laboratory of Diabetology. Dr Weng received his Bachelor degree at the former Nanjing Railway Medical College, Master and Ph.D degrees at the former Sun Yat-sen University of Medical Science. He was a research fellow of the Department of Endocrinology at Malmö University Hospital in Lund, Sweden. Dr Weng’s research interests focus on endocrinology, metabolic disease and genetics in diabetes. He has published over 110 scientific articles in international peer-reviewed journals including the Lancet, Molecular Endocrinology, Endocrinology, Human Genetics, Diabetes, Diabetes Care. His research has been funded by National Natural Science Foundation of China (NSFC), Hi-tech Research and Development Program of China (863 program), National Health and Family Planning Commission and Ministry of Education. He is the Editor-in-Chief of the Chinese Journal of Diabetes Mellitus, and the Associate Editor-in-Chief of the Chinese Medical Journal. He is also a board editor of the Diabetes and of the Journal of Internal Medicine. Dr Weng was the President of the Chinese Diabetes Society 2012−2015. Over the years, he has garnered much recognition and accolade from the scientific community, including being named an Outstanding Young Scholar by the NSFC in 2010, and a Changjiang Scholar professor by the Ministry of Education in 2012. He was also a winner of the Support Program for 100 Outstanding Talents in Guangdong in 2013.
Prof. Yiming Mu is Professor and Chief of the Department of Endocrinology, Chinese PLA General Hospital, in Beijing. He also holds the post of the President of Chinese Society of Endocrinology (CSE) and Vice President of the Chinese Endocrinologist Association. He received the Distinguished Contribution Award of the CSE in 2014. Professor Mu completed his basic medical education in China and then went to Japan to hone his skills on the principles of molecular research and obtained a Ph.D degree from the Kyushu University in Japan. His broad research interests are reflected in more than 400 publications to date in diverse fields including diabetes, glucose metabolism and pancreatic beta-cell biology and stem cell biology.
Prof. Weiping Jia is now Professor of Division of Endocrinology & metabolism at Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Director of Shanghai Clinical Center for Diabetes, Shanghai Key Laboratory for Diabetes and Shanghai Diabetes Institute. Dr. Jia is now president of Chinese Diabetes Society, and Chief Editor of Chinese Journal of Internal Medicine as well as editorial board members of Lancet Diabetes Endocrinology and Diabetes. Her research interest involved various aspects of diabetes, obesity and metabolic disorders from genetic and molecular biology to disease management, especially the translational research on the disease. She has published more than 400 papers and over 100 research articles in international scientific journals, including British Medical Journal, Journal of the American College of Cardiology, Diabetes, Diabetes Care, Diabetologia, Journal of Clinical Endocrinology and Metabolism, American Journal of Psychiatry, and Obesity Review, etc. Her research has been funded by National Natural Science Foundation of China (NSFC), National Basic Research Program of China (973 program), Hi-tech Research and Development Program of China (863 program), and European Association for the Study of Diabetes (EASD). She is the Co-PI of research projects funded by the National Institute of Health (NIH) in USA.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Xu, W., Mu, Y., Zhao, J. et al. Efficacy and safety of metformin and sitagliptin based triple antihyperglycemic therapy (STRATEGY): a multicenter, randomized, controlled, non-inferiority clinical trial. Sci. China Life Sci. 60, 225–238 (2017). https://doi.org/10.1007/s11427-016-0409-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11427-016-0409-7