Abstract
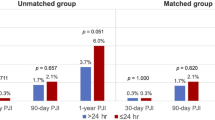
In 2018, Inabathula et al. published the results of a historical control study examining 90-day peri-prosthetic joint infection (PJI) rates at a single center before and after the institution of an extended post-operative oral antibiotic protocol for high-risk total hip arthroplasty (THA) and total knee arthroplasty (TKA) patients. In the study, “Extended Oral Antibiotic Prophylaxis in High-Risk Patients Substantially Reduces Primary Total Hip and Knee Arthroplasty 90-Day Infection Rate” (J Bone Joint Surg Am. 2018;100[24]:2103–2109), the authors considered any one of several patient-related criteria—including diabetes, a body mass index of 35 kg/m2 or higher, or active smoking—as sufficient to designate a patient “high risk” for PJI. Before the extended antibiotic therapy protocol was instituted, PJI rates for primary THA and TKA in the high-risk subgroup were 4.3% and 2.1%, respectively. After it was instituted, the respective rates dropped to 1.1% and 0.4%, comparable to those seen in the non-high-risk patients treated using standard peri-operative prophylaxis. After adjusting for patient factors, regression analysis showed that high-risk patients receiving only peri-operative antibiotics were more likely to develop PJI than high-risk patients receiving the extended antibiotic protocol. Although these results suggest possible benefits of extended antibiotic prophylaxis in arthroplasty, methodologic limitations and inadequate discussion of potential drawbacks of widespread adoption of such protocols limit the impact of the findings. Future research is warranted to more narrowly define risk factors for PJI and to demonstrate the safety and efficacy of extended antibiotics in reducing the long-term burden of PJI.
Similar content being viewed by others
References
Aboltins CA, Berdal JE, Casas F, et al. Hip and Knee Section, Prevention, Antimicrobials (Systemic): Proceedings of International Consensus on Orthopedic Infections. J Arthroplasty. 2019;34(2S):S279–S288.
Ascione T, Balato G, Mariconda M, Rotondo R, Baldini A, Pagliano P. Continuous antibiotic therapy can reduce recurrence of prosthetic joint infection in patients undergoing 2-stage exchange. J Arthroplasty. 2019;34(4):704–709.
Baquero F, Hsueh P, Paterson DL, et al. In vitro susceptibilities of aerobic and facultatively anaerobic gram-negative bacilli isolated from patients with intra-abdominal infections worldwide: 2005 results from Study for Monitoring Antimicrobial Resistance Trends (SMART). Surg Infect (Larchmt). 2009;10:99–104.
Burke JF. The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery. 1961;50:161–168.
Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, Burke JP. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med. 1992;326:281–286.
Dale H, Hallan G, Espehaug B, Havelin LI, Engesæter LB. Increasing risk of revision due to deep infection after hip arthroplasty. Acta Orthopaedica. 2009;80:639–645.
Harbarth S, Samore MH, Lichtenberg D, Carmeli Y. Prolonged antibiotic prophylaxis after cardiovascular surgery and its effect on surgical site infections and antimicrobial resistance. Circulation. 2000;101:2916–2921.
Inabathula A, Dilley JE, Ziemba-Davis M, et al. Extended oral antibiotic prophylaxis in high-risk patients substantially reduces primary total hip and knee arthroplasty 90-day infection rate. J Bone Joint Surg Am. 2018;100:2103–2109.
Kapadia BH, Berg RA, Daley JA, Fritz J, Bhave A, Mont MA. Periprosthetic joint infection. Lancet. 2016;387:386–394.
Khatod M. Prepare for more antibiotics: commentary on an article by Avinash Inabathula, MD, et al.: “Extended Oral Antibiotic Prophylaxis in High-Risk Patients Substantially Reduces Primary Total Hip and Knee Arthroplasty 90-Day Infection Rate.” J Bone Joint Surg Am. 2018;100:e155.
Kurtz S, Ong K, Lau E, Bozic K, Berry D, Parvizi J. Prosthetic joint infection risk after TKA in the Medicare population. Clin Orthop Relat Res. 2010;468:52–56.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785.
Kurtz SM, Lau EC, Son M, Chang ET, Zimmerli W, Parvizi J. Are we winning or losing the battle with periprosthetic joint infection: trends in periprosthetic joint infection and mortality risk for the Medicare population. J Arthroplasty. 2018;33:3238–3245.
Parvizi J, Gehrke T, Chen AF. Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Joint J. 2013;95-B:1450–1452.
Roberts NJ, Douglas RG. Gentamicin use and Pseudomonas and Serratia resistance: effect of a surgical prophylaxis regimen. Antimicrob Agents Chemother. 1978;13(2):214–220.
Siddiqi A, Forte SA, Docter S, Bryant D, Sheth NP, Chen AF. Perioperative antibiotic prophylaxis in total joint arthroplasty: a systematic review and meta-analysis. J Bone Joint Surg Am. 2019;101:828–842.
Tande AJ, Gomez-Urena EO, Berbari EF, Osmon DR. Management of prosthetic joint infection. Infect Dis Clin North Am. 2017;31:237–252; doi: https://doi.org/10.1016/j.idc.2017.01.009.
Yates AJ. Postoperative prophylactic antibiotics in total joint arthroplasty. Arthroplast Today. 2018;4:130–131.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Christopher J. DeFrancesco, MD; Michael C. Fu, MD, MHS; Cynthia A. Kahlenberg, MD; and Andy O. Miller, MD, declare that they have no conflicts of interest. Mathias P. Bostrom, MD, reports personal fees from Smith & Nephew, outside the submitted work.
Human/Animal Rights
N/A
Informed Consent
N/A
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Rights and permissions
About this article
Cite this article
DeFrancesco, C.J., Fu, M.C., Kahlenberg, C.A. et al. Extended Antibiotic Prophylaxis May Be Linked to Lower Peri-prosthetic Joint Infection Rates in High-Risk Patients: An Evidence-Based Review. HSS Jrnl 15, 297–301 (2019). https://doi.org/10.1007/s11420-019-09698-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-019-09698-8