Abstract
Background
In the midst of the nationwide opioid epidemic, our institution began an effort to improve the education of opioid prescribers and disseminate procedure-specific guidelines for the number of opioid pills to prescribe post-operatively for total joint arthroplasty. The number of opioid pills suggested for total hip or knee replacement was 70 tablets.
Questions/Purposes
We sought to evaluate the impact of the new institutional guideline on opioid prescribing practices, hypothesizing that it would lead to a decrease in the number of pills prescribed but an increase in patient call volume after discharge.
Methods
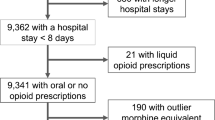
After the new guidelines were implemented in February 2018, we retrospectively reviewed all opioid prescriptions written for patients on the joint-replacement service from March 2016 to March 2018. In addition, we tabulated post-operative telephone calls made to the nurse practitioner service before and after guideline implementation. The majority of calls to the nurse practitioner service are for opioid renewals.
Results
We included 9514 patients in the analysis. Prior to guideline implementation, the mean number of pills prescribed after primary total joint arthroplasty was 91 ± 26.6 pills and after it was 65 ± 16.3 pills. The monthly number of unique patient telephone interactions was statistically significantly lower after the implementation of the new guidelines.
Conclusion
An institutional guideline for opioid prescribing after total joint arthroplasty significantly reduced the number of pills prescribed to patients without causing a significant increase in the number of phone calls to the service.

Similar content being viewed by others
References
American Academy of Orthopaedic Surgeons. Information statement 1045. Opioid use, misuse, and abuse in orthopaedic practice. 2015. Available at https://www.aaos.org/uploadedFiles/PreProduction/About/Opinion_Statements/advistmt/1045 Opioid Use, Misuse, and Abuse in Practice.pdf.
Chiu AS, Jean RA, Hoag JR, Freedman-Weiss M, Healy JM, Pei KY. Association of lowering default pill counts in electronic medical record systems with postoperative opioid prescribing. JAMA Surg. Published online July 18, 2018. https://doi.org/10.1001/jamasurg.2018.2083.
Cozowicz C, Olson A, Poeran J, et al. Opioid prescription levels and postoperative outcomes in orthopedic surgery. Pain. 2017;158(12):2422–2430.
Cushman PA, Liebschutz JM, Hodgkin JG, et al. What do providers want to know about opioid prescribing? A qualitative analysis of their questions. Subst Abus. 2017;38:222–229.
Donaldson SR, Harding AM, Taylor SE, Vally H, Greene SL. Evaluation of a targeted prescriber education intervention on emergency department discharge oxycodone prescribing. Emerg Med Australas. 2017;29:400–406.
Dwyer CL, Soong M, Hunter A, Dashe J, Tolo E, Kasparyan NG. Prospective evaluation of an opioid reduction protocol in hand surgery. J Hand Surg Am. 2018; 43(6):516–522.
Fink A, Kosecoff J, Chassin M, Brook RH. Consensus methods: characteristics and guidelines for use. Am J Pub Health. 1984;74:979–983.
Goesling J, Moser SE, Zaidi B, et al. Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain. 2016;157:1259–1265.
Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003–2013. JAMA. 2015;314:1468–1478.
Hernandez NM, Parry JA, Taunton MJ. Patients at risk: large opioid prescriptions after total knee arthroplasty. J Arthroplast. 2017;32:2395–2398.
Khalid L, Liebschutz JM, Xuan Z, et al. Adherence to prescription opioid monitoring guidelines among residents and attending physicians in the primary care setting. Pain Med. 2015;16:480–487.
Kim N, Matzon JL, Abboudi J, et al. A prospective evaluation of opioid utilization after upper-extremity surgical procedures: identifying consumption patterns and determining prescribing guidelines. J Bone Joint Surg Am. 2016;98:e89.
Kumar K, Gulotta LV, Dines JS, et al. Unused opioid pills after outpatient shoulder surgeries given current perioperative prescribing habits. Am J Sports Med. 2017;45:636–641.
Manchikanti L, Helm S, Fellows B, et al. Opioid epidemic in the United States. Pain Physician. 2012;15:ES9–38.
Rodgers J, Cunningham K, Fitzgerald K, Finnerty E. Opioid consumption following outpatient upper extremity surgery. J Hand Surg Am 2012;37:645–650.
Schairer WW, Kahlenberg CA, Sculco PK, Nwachukwu BU. What is the quality of online resources about pain control after total knee arthroplasty? J Arthroplasty. 2017;32(12):3616–3620.
Seth P, Scholl L, Rudd RA, Bacon S. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67(12):349–358.
Seymour RB, Ring D, Higgins T, Hsu JR. Leading the way to solutions to the opioid epidemic: AOA critical issues. J Bone Joint Surg Am. 2017; 99(21):e113.
Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long-term opioid use—United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66:265–269.
Stanek JJ, Renslow MA, Kalliainen LK. The effect of an educational program on opioid prescription patterns in hand surgery: a quality improvement program. J Hand Surg Am. 2015;40:341–346.
Stepan JG, London DA, Osei DA, Boyer MI, Dardas AZ, Calfee RP. Perioperative celecoxib and postoperative opioid use in hand surgery: a prospective cohort study. J Hand Surg Am. 2018;43:346–353.
Volkow ND, McLellan TA, Cotto JH, Karithanom M, Weiss SRB. Characteristics of opioid prescriptions in 2009. JAMA. 2011;305:1299–301.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Cynthia A. Kahlenberg, MD, Jeffrey G. Stepan, MD, Ajay Premkumar, MD, MPH, and Francis D. Lovecchio, MD, declare that they have no conflicts of interest. Michael B. Cross, MD, reports receiving grants or personal fees from or owning stock in Acelity, Exactech, Inc., Intellijoint, Link Orthopaedics, Smith & Nephew, Zimmer, Flexion Therapeutics, Imagen, Insight Medical, and Parvizi Surgical Innovation, as well as serving on the editorial or governing boards of Bone and Joint Journal 360, Journal of Orthopaedics and Traumatology, and Techniques in Orthopaedics, all outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Additional information
Level of Evidence: Level IV, retrospective review
Rights and permissions
About this article
Cite this article
Kahlenberg, C.A., Stepan, J.G., Premkumar, A. et al. Institutional Guidelines Can Decrease the Amount of Opioids Prescribed After Total Joint Replacement. HSS Jrnl 15, 27–30 (2019). https://doi.org/10.1007/s11420-018-9632-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-018-9632-6