Abstract
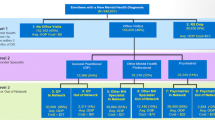
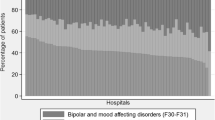
Analyses of healthcare expenditures and adequacy are needed to identify cost-effective policies and practices that improve mental healthcare quality. Data are from 2010 to 2012 electronic health records from three hospital psychiatry departments in Madrid (n = 29,944 person-years) and three in Boston (n = 14,109 person-years). Two-part multivariate generalized linear regression and logistic regression models were estimated to identify site differences in mental healthcare expenditures and quality of care. Annual total average treatment expenditures were $4442.14 in Boston and $2277.48 in Madrid. Boston patients used inpatient services more frequently and had higher 30-day re-admission rates (23.7 vs. 8.7%) despite higher rates of minimally adequate care (49.5 vs. 34.8%). Patients in Madrid were more likely to receive psychotropic medication, had fewer inpatient stays and readmissions, and had lower expenditures, but had lower rates of minimally adequate care. Differences in insurance and healthcare system policies and mental health professional roles may explain these dissimilarities.
Similar content being viewed by others
References
Hamid H, Abanilla K, Bauta B, et al. Evaluating the WHO Assessment Instrument for Mental Health Systems by Comparing Mental Health Policies in Four Countries. Bulletin of the World Health Organization. 2008;86(6):467–473.
Kessler RC, Zhao S, Katz SJ, et al. Past-Year Use of Outpatient Services for Psychiatric Problems in the National Comorbidity Survey. American Journal of Psychiatry. 1999;156:115–123.
Wittchen HU, Jacobi F. Size and Burden of Mental Disorders in Europe—A Critical Review and Appraisal of 27 Studies. European Neuropsychopharmacology. 2005;15(4):357–376.
Degenhardt L, Hall W. Extent of Illicit Drug Use and Dependence, and Their Contribution to the Global Burden of Disease. Lancet. 2012;379(9810):55–70.
Olfson M, Kessler RC, Berglund PA, et al. Psychiatric Disorder Onset and First Treatment Contact in the United States and Ontario. American Journal of Psychiatry. 1998;155(10):1415–1422.
Wang PS, Demler O, Kessler RC. Adequacy of Treatment for Serious Mental Illness in the United States. American Journal of Public Health. 2002;92(1):92–98.
Feachem R, Dixon, J, Berwick, DM, et al. Getting More for Their Dollar: A Comparison of the NHS with California's Kaiser Permanente. British Medical Journal. 2002;324:135–141.
Moran V, Jacobs R. An International Comparison of Efficiency of Inpatient Mental Health Care Systems. Health Policy. 2013;112(1–2):88–89.
Hannigan B, Coffey M. Where the Wicked Problems Are: The Case of Mental Health. Health Policy. 2011;101(3):220–227.
Hussey PS, Wertheimer S, Mehrotra A. The Association between Health Care Auality and Cost: A Systematic Review. Annals of Internal Medicine. 2013;158(1):27–34.
Lostao L, Blane D, Gimeno D, et al. Socioeconomic Patterns in Use of Private and Public Health Services in Spain and Britain: Implications for Equity in Health Care. Health & Place. 2014;25:19–25.
Andrulis DP, Siddiqui NJ. Health Reform Holds Both Risks and Rewards for Safety-Net Providers and Racially and Ethnically Diverse Patients. Health Affairs. 2011;30(10):1830–1836.
Fernández A, Haro JM, Codony M, et al. Treatment Adequacy of Anxiety and Depressive Disorders: Primary Versus Specialised Care in Spain. Journal of Affective Disorders. 2006;96(1):9–20.
Mechanic D. More People Than Ever Before are Receiving Behavioral Health Care in the United States, But Gaps and Challenges Remain. Health Affairs. 2014;33(8):1416–1424.
Dezetter A, Briffault X, Alonso J, et al. Factors Associated with Use of Psychiatrists and Nonpsychiatrist Providers by ESEMeD Respondents in Six European Countries. Psychiatric Services. 2011;62(2):143–151.
Saloner B, Bandara S, Bachhuber M, et al. Insurance Ccoverage And Treatment Use Under the Affordable Care Act among Adults with Mental and Substance Use Disorders. Psychiatric Services. 2017;68(6):542–548.
McGuire TG, Alegria M, Cook BL, et al. Implementing the Institute of Medicine Definition of Disparities: An Application to Mental Health Care. Health Services Research. 2006;41(5):1979–2005.
Reeves A, Gourtsoyannis Y, Basu S, et al. Financing Universal Health Coverage—Effects of Alternative Tax Structures on Public Health Systems: Cross-National Modelling in 89 Low-Income and Middle-Income Countries. The Lancet. 2015;386(9990):274–280.
Moran V, O'Connor S, Borowitz M. International Approaches to Measuring the Quality of Mental Health Care. Epidemiology and Psychiatric Sciences. 2013;22(01):3–7.
Zuvekas SH. Trends in Mental Health Services Use and Spending, 1987-1996. Health Affairs. 2001;20(2):212–224.
Alegría M, Chatterji P, Wells K, et al. Disparity in Depression Treatment among Racial and Ethnic Minority Populations in the United States. Psychiatric Services. 2008;59(11):1264.
Cook BL, Zuvekas SH, Carson N, et al. Assessing Racial/Ethnic Disparities in Treatment Across Episodes of Mental Health Care. Health Services Research. 2014;49(1):206–229.
Hernandez AF, Curtis LH. Minding the Gap between Efforts to Reduce Readmissions and Disparities. The Journal of the American Medical Association. 2011;305(7):715–716.
Benbassat J, Taragin, M. Hospital Readmissions as a Measure of Quality of Health Care: Advantages and Limitations. Archives of Internal Medicine. 2000;160(8):1074–1081.
111th Congress. Compilation of Patient Protection and Affordable Care Act: 42 U.S.C.. U.S. Department of Health and Human Services. Available online at https://www.hhs.gov/sites/default/files/ppacacon.pdf. Accessed on August 24, 2017.
Rubin DB. Multiple Imputation of Nonresponse in Surveys. New York, NY: Wiley, 2004.
McCullagh P, Nelder J. Generalized Linear Models. London: Chapman and Hall; 1989.
Buntin MB, Zaslavsky AM. Too Much Ado about Two-Part Models and Transformation?: Comparing Methods of Modeling Medicare Expenditures. Journal of Health Economics. 2004;23(3):525–542.
Manning WG, Mullahy J. Estimating Log Models: To Transform or Not To Transform? Journal of Health Economics. 2001;20(4):461–494.
Glied S. Managed care. In: AJ Culyer, JP Newhouse (Eds). Handbook of Health Economics, Volume 1. North Holland: Elsevier, 2000, pp. 707–753.
Robinson JC, Shortell SM, Li R, et al. The Alignment and Blending of Payment Incentives within Physician Organizations. Health Services Research. 2004;39(5):1589–1606.
Amaddeo F, Grigoletti L, Montagni I. Mental Health Care Financing in Italy: Current Situation and Perspectives. The Journal of Nervous and Mental Disease. 2014;202(6):464–468.
Gosden T, Forland F, Kristiansen I, et al. Capitation, Salary, Fee-for-Service and Mixed Systems of Payment: Effects on the Behaviour of Primary Care Physicians. Cochrane Database of Systematic Reviews. 2000; Art. No.: CD002215.
Sobotka T, Toulemon L. Overview Chapter 4: Changing Family and Partnership Behaviour: Common Trends and Persistent Diversity Across Europe. Demographic Research. 2008;19(6):85–138.
Zunzunegui MV, Beland F, Otero A. Support from Children, Living Arrangements, Self-Rated Health and Depressive Symptoms of Older People in Spain. International Journal of Epidemiology. 2001;30(5):1090–1099.
Mynors-Wallis LM, Gath DH, Day A, et al. Randomised Controlled Trial of Problem Solving Treatment, Antidepressant Medication, and Combined Treatment for Major Depression in Primary Care. British Medical Journal. 2000;320(7226):26–30.
Salminen JK, Karlsson H, Hietala J, et al. Short-Term Psychodynamic Psychotherapy and Fluoxetine in Major Depressive Disorder: A Randomized Comparative Study. Psychotherapy and Psychosomatics. 2008;77(6):351–357.
Strandberg-Larsen M. Measuring Integrated Care. Danish Medical Bulletin. 2011;58(2):B4245.
Fourie C, Biller-Andorno N, Wild V. Systematically Evaluating the Impact of Diagnosis-Related Groups (DRGs) on Health Care Delivery: A Matrix of Ethical Implications. Health Policy. 2014;115(2–3):157–164.
Frank RG, Goldman HH, McGuire TG. Trends in Mental Health Cost Growth: An Expanded Role for Management? Health Affairs. 2009;28(3):649–659.
Falgas I, Ramos Z, Herrera L, et al. Barriers to and Correlates of Retention in Behavioral Health Treatment among Latinos in 2 Different Host Countries: The United States and Spain. Journal of Public Health Management and Practice. 2016;23(1):e20-e27.
Funding
This study was supported by the National Institute on Drug Abuse Grant 5R01DA034952-02. Researchers are independent from funders.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Carmona, R., Cook, B.L., Baca-García, E. et al. Comparison of Mental Health Treatment Adequacy and Costs in Public Hospitals in Boston and Madrid. J Behav Health Serv Res 46, 464–474 (2019). https://doi.org/10.1007/s11414-018-9596-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11414-018-9596-9