Abstract
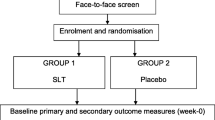
Nicotinamide riboside (NR) increases blood levels of NAD+, a cofactor central to energy metabolism, and improves brain function in some rodent models of neurodegeneration. We conducted a placebo-controlled randomized pilot study with the primary objective of determining safety of NR in older adults with mild cognitive impairment (MCI). Twenty subjects with MCI were randomized to receive placebo or NR using dose escalation to achieve, and maintain, a final dose of 1 g/day over a 10-week study duration. The primary outcome was post-treatment change from baseline measures of cognition (Montreal Cognitive Assessment, MoCA). Predefined secondary outcomes included post-treatment changes in cerebral blood flow (CBF); blood NAD+ levels; and additional neurocognitive, psychometric, and physical performance tests. DNA methylation was assessed in peripheral blood mononuclear cells (PBMCs) as an exploratory outcome. The target NR dose was safely achieved as evidenced by a 2.6-fold increase in blood NAD+ in the NR group (p < 0.001, 95% CI [17.77, 43.49]) with no between-group difference in adverse event reporting. MoCA and other neurocognitive and psychometric metrics remained stable throughout the study. NR reduced CBF in the default mode network (DMN) with greatest differences observed in the left inferior parietal lobe (IPL) (DMN p = 0.013, μ = 0.92, 95% CI [0.23, 1.62]; left IPL p = 0.009, μ = 1.66, 95% CI [0.5, 2.82]). Walking speed in the placebo group significantly improved across the study duration suggestive of a practice effect but did not change in the NR group (p = 0.0402 and p = 0.4698, respectively). Other secondary outcome measures remained stable. Global methylation analyses indicated a modest NR-associated increase in DNA methylation and concomitant reduction in epigenetic age as measured by PhenoAge and GrimAge epigenetic clock analyses. In summary, NR significantly increased blood NAD+ concentrations in older adults with MCI. NR was well tolerated and did not alter cognition. While CBF was reduced by NR treatment, statistical significance would not have withstood multiple comparisons correction. A larger trial of longer duration is needed to determine the potential of NR as a strategy to improve cognition and alter CBF in older adults with MCI. ClinicalTrials.gov NCT02942888





Similar content being viewed by others
Data Availability
The minimum datasets necessary to interpret, verify and extend the research in the article are available within the paper and its Supplementary Information. The trial was registered on ClinicalTrials.gov: NCT02942888.
References
Petersen RC, et al. Mild cognitive impairment: ten years later. Arch Neurol. 2009;66(12):1447–55.
Roberts RO, et al. The Mayo Clinic Study of Aging: design and sampling, participation, baseline measures and sample characteristics. Neuroepidemiology. 2008;30(1):58–69.
Busse A, et al. Mild cognitive impairment: long-term course of four clinical subtypes. Neurology. 2006;67(12):2176–85.
Panza F, et al. Current epidemiology of mild cognitive impairment and other predementia syndromes. Am J Geriatr Psychiatry. 2005;13(8):633–44.
Petersen RC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56(3):303–8.
Bozoki A, et al. Mild cognitive impairments predict dementia in nondemented elderly patients with memory loss. Arch Neurol. 2001;58(3):411–6.
Morris JC, et al. Mild cognitive impairment represents early-stage Alzheimer disease. Arch Neurol. 2001;58(3):397–405.
Ritchie K, Artero S, Touchon J. Classification criteria for mild cognitive impairment: a population-based validation study. Neurology. 2001;56(1):37–42.
Daly E, et al. Predicting conversion to Alzheimer disease using standardized clinical information. Arch Neurol. 2000;57(5):675–80.
Grober E, et al. Memory impairment on free and cued selective reminding predicts dementia. Neurology. 2000;54(4):827–32.
Jicha GA, et al. Neuropathologic outcome of mild cognitive impairment following progression to clinical dementia. Arch Neurol. 2006;63(5):674–81.
2023 Alzheimer's disease facts and figures. Alzheimers Dement. 2023;19(4):1598–1695.
Gonzales MM, et al. Biological aging processes underlying cognitive decline and neurodegenerative disease. J Clin Invest. 2022;132(10).
Tong JJ, et al. Chronic acarbose treatment alleviates age-related behavioral and biochemical changes in SAMP8 mice. Behav Brain Res. 2015;284:138–52.
Dunn HC, et al. Restoration of lipoxin A4 signaling reduces Alzheimer’s disease-like pathology in the 3xTg-AD mouse model. J Alzheimers Dis. 2015;43(3):893–903.
Chandra S, Jana M, Pahan K. Aspirin induces lysosomal biogenesis and attenuates amyloid plaque pathology in a mouse model of Alzheimer’s disease via PPARalpha. J Neurosci. 2018;38(30):6682–99.
Medeiros R, et al. Aspirin-triggered lipoxin A4 stimulates alternative activation of microglia and reduces Alzheimer disease-like pathology in mice. Am J Pathol. 2013;182(5):1780–9.
Caccamo A, et al. Molecular interplay between mammalian target of rapamycin (mTOR), amyloid-beta, and Tau: effects on cognitive impairments. J Biol Chem. 2010;285(17):13107–20.
Majumder S, et al. Inducing autophagy by rapamycin before, but not after, the formation of plaques and tangles ameliorates cognitive deficits. PLoS One. 2011;6(9):e25416.
Zhang L, et al. Evaluating the effectiveness of GTM-1, rapamycin, and carbamazepine on autophagy and Alzheimer disease. Med Sci Monit. 2017;23:801–8.
Orr ME, et al. Mammalian target of rapamycin hyperactivity mediates the detrimental effects of a high sucrose diet on Alzheimer’s disease pathology. Neurobiol Aging. 2014;35(6):1233–42.
Musi N, et al. Tau protein aggregation is associated with cellular senescence in the brain. Aging Cell. 2018;17(6):e12840.
Gonzales MM, et al. A geroscience motivated approach to treat Alzheimer’s disease: senolytics move to clinical trials. Mech Ageing Dev. 2021;200:111589.
Gonzales MM, et al. Senolytic therapy in mild Alzheimer’s disease: a phase 1 feasibility trial. Nat Med. 2023;29(10):2481–8.
Rajman L, Chwalek K, Sinclair DA. Therapeutic potential of NAD-boosting molecules: the in vivo evidence. Cell Metab. 2018;27(3):529–47.
Ansari HR, Raghava GP. Identification of NAD interacting residues in proteins. BMC Bioinform. 2010;11:160.
Zhu XH, et al. In vivo NAD assay reveals the intracellular NAD contents and redox state in healthy human brain and their age dependences. Proc Natl Acad Sci U S A. 2015;112(9):2876–81.
Long AN, et al. Effect of nicotinamide mononucleotide on brain mitochondrial respiratory deficits in an Alzheimer’s disease-relevant murine model. BMC Neurol. 2015;15:19.
Klaidman LK, et al. Nicotinamide as a precursor for NAD+ prevents apoptosis in the mouse brain induced by tertiary-butylhydroperoxide. Neurosci Lett. 1996;206(1):5–8.
Donmez G, et al. SIRT1 suppresses beta-amyloid production by activating the alpha-secretase gene ADAM10. Cell. 2010;142(2):320–32.
Fang EF, et al. Mitophagy inhibits amyloid-beta and tau pathology and reverses cognitive deficits in models of Alzheimer’s disease. Nat Neurosci. 2019;22(3):401–12.
Hou Y, et al. NAD(+) supplementation normalizes key Alzheimer’s features and DNA damage responses in a new AD mouse model with introduced DNA repair deficiency. Proc Natl Acad Sci U S A. 2018;115(8):E1876–85.
Xu XJ, Jiang GS. Niacin-respondent subset of schizophrenia - a therapeutic review. Eur Rev Med Pharmacol Sci. 2015;19(6):988–97.
Holubiec P, et al. Pathophysiology and clinical management of pellagra - a review. Folia Med Cracov. 2021;61(3):125–37.
Mero A, et al. Effects of nicotinamide adenine dinucleotide hydride on physical and mental performance. J Sports Sci. 2008;26(3):311–9.
Arenas-Jal M, et al. Trends in the food and sports nutrition industry: a review. Crit Rev Food Sci Nutr. 2020;60(14):2405–21.
DS W, et al. Drugbank: a comprehensive resource for in silico drug discovery and exploration. Nucleic Acids Res. 2006;34:D668–72.
Bieganowski P, Brenner C. Discoveries of nicotinamide riboside as a nutrient and conserved NRK genes establish a Preiss-Handler independent route to NAD+ in fungi and humans. Cell. 2004;117(4):495–502.
Trammell SA, et al. Nicotinamide riboside is uniquely and orally bioavailable in mice and humans. Nat Commun. 2016;7:12948.
Conze D, Brenner C, Kruger CL. Safety and metabolism of long-term administration of NIAGEN (nicotinamide riboside chloride) in a randomized, double-blind, placebo-controlled clinical trial of healthy overweight adults. Sci Rep. 2019;9(1):9772.
Airhart SE, et al. An open-label, non-randomized study of the pharmacokinetics of the nutritional supplement nicotinamide riboside (NR) and its effects on blood NAD+ levels in healthy volunteers. PLoS One. 2017;12(12):e0186459.
Brakedal B, et al. The NADPARK study: a randomized phase I trial of nicotinamide riboside supplementation in Parkinson’s disease. Cell Metab. 2022;34(3):396-407 e6.
Vreones M, et al. Oral nicotinamide riboside raises NAD+ and lowers biomarkers of neurodegenerative pathology in plasma extracellular vesicles enriched for neuronal origin. Aging Cell. 2022;22:e13754.
Nasreddine ZS, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9.
Segal DL, et al. Development and initial validation of a self-report assessment tool for anxiety among older adults: the Geriatric Anxiety Scale. J Anxiety Disord. 2010;24(7):709–14.
Trammell SA, Brenner C. Targeted, LCMS-based metabolomics for quantitative measurement of NAD(+) metabolites. Comput Struct Biotechnol J. 2013;4:e201301012.
Aryee MJ, et al. Minfi: a flexible and comprehensive Bioconductor package for the analysis of Infinium DNA methylation microarrays. Bioinformatics. 2014;30(10):1363–9.
Ram V, ZJ C. ggplot2: elegant graphics for data analysis. 2nd ed. Meas Interdiscip Res Perspect; 2019.
Ritchie ME, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43(7):e47.
Martorell-Marugan J, Gonzalez-Rumayor V, Carmona-Saez P. mCSEA: detecting subtle differentially methylated regions. Bioinformatics. 2019;35(18):3257–62.
Hannum G, et al. Genome-wide methylation profiles reveal quantitative views of human aging rates. Mol Cell. 2013;49(2):359–67.
Levine ME, et al. An epigenetic biomarker of aging for lifespan and healthspan. Aging (Albany NY). 2018;10(4):573–91.
Lu AT, et al. DNA methylation GrimAge strongly predicts lifespan and healthspan. Aging (Albany NY). 2019;11(2):303–27.
Ho J, et al. Moving beyond P values: data analysis with estimation graphics. Nat Methods. 2019;16(7):565–6.
Katz S, et al. Studies of illness in the aged. The index of Adl: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–86.
Royall DR, Mahurin RK, Gray KF. Bedside assessment of executive cognitive impairment: the executive interview. J Am Geriatr Soc. 1992;40(12):1221–6.
Royall DR, Cordes JA, Polk M. CLOX: an executive clock drawing task. J Neurol Neurosurg Psychiatry. 1998;64(5):588–94.
Douaud G, et al. Anatomically related grey and white matter abnormalities in adolescent-onset schizophrenia. Brain. 2007;130(Pt 9):2375–86.
Good CD, et al. A voxel-based morphometric study of ageing in 465 normal adult human brains. Neuroimage. 2001;14(1 Pt 1):21–36.
Smith SM, et al. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage. 2004;23(Suppl 1):S208–19.
Andersson JL, Jenkinson M, Smith S. Non-linear registration aka spatial normalisation. Oxford, United Kingdom: FMRIB Centre; 2007.
Ma C, et al. Variational Bayesian inference for a nonlinear forward model. IEEE Trans Signal Proc. 2009;57(1):223–36.
Jenkinson M, et al. Fsl. Neuroimage. 2012;62(2):782–90.
Laird AR, et al. Investigating the functional heterogeneity of the default mode network using coordinate-based meta-analytic modeling. J Neurosci. 2009;29(46):14496–505.
Guralnik JM, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94.
Martens CR, et al. Chronic nicotinamide riboside supplementation is well-tolerated and elevates NAD(+) in healthy middle-aged and older adults. Nat Commun. 2018;9(1):1286.
Li K, et al. Progressive bidirectional age-related changes in default mode network effective connectivity across six decades. Front Aging Neurosci. 2016;8:137.
Horvath S, Raj K. DNA methylation-based biomarkers and the epigenetic clock theory of ageing. Nat Rev Genet. 2018;19(6):371–84.
Grant R, et al. A pilot study investigating changes in the human plasma and urine NAD+ metabolome during a 6 hour intravenous infusion of NAD. Front Aging Neurosci. 2019;11:257.
Elhassan YS, et al. Nicotinamide riboside augments the aged human skeletal muscle NAD(+) metabolome and induces transcriptomic and anti-inflammatory signatures. Cell Rep. 2019;28(7):1717-1728 e6.
Remie CME, et al. Nicotinamide riboside supplementation alters body composition and skeletal muscle acetylcarnitine concentrations in healthy obese humans. Am J Clin Nutr. 2020;112.
Dollerup OL, et al. A randomized placebo-controlled clinical trial of nicotinamide riboside in obese men: safety, insulin-sensitivity, and lipid-mobilizing effects. Am J Clin Nutr. 2018;108(2):343–53.
Krishnan K, et al. Changes in Montreal Cognitive Assessment scores over time. Assessment. 2017;24(6):772–7.
Jagust WJ, et al. Brain function and cognition in a community sample of elderly Latinos. Neurology. 2002;59(3):378–83.
Haan MN, et al. Prevalence of dementia in older Latinos: the influence of type 2 diabetes mellitus, stroke and genetic factors. J Am Geriatr Soc. 2003;51(2):169–77.
Mulrow CD, et al. Function and medical comorbidity in south Texas nursing home residents: variations by ethnic group. J Am Geriatr Soc. 1996;44(3):279–84.
Tabatabaei-Jafari H, Shaw ME, Cherbuin N. Cerebral atrophy in mild cognitive impairment: a systematic review with meta-analysis. Alzheimers Dement (Amst). 2015;1(4):487–504.
Damoiseaux JS, et al. Reduced resting-state brain activity in the “default network” in normal aging. Cereb Cortex. 2008;18(8):1856–64.
Jones DT, et al. Age-related changes in the default mode network are more advanced in Alzheimer disease. Neurology. 2011;77(16):1524–31.
Greicius MD, et al. Default-mode network activity distinguishes Alzheimer’s disease from healthy aging: evidence from functional MRI. Proc Natl Acad Sci U S A. 2004;101(13):4637–42.
Arora A, et al. Left inferior-parietal lobe activity in perspective tasks: identity statements. Front Hum Neurosci. 2015;9:360.
Dai W, et al. Mild cognitive impairment and Alzheimer disease: patterns of altered cerebral blood flow at MR imaging. Radiology. 2009;250(3):856–66.
Zhou J, et al. Predicting regional neurodegeneration from the healthy brain functional connectome. Neuron. 2012;73(6):1216–27.
Fatokun AA, Stone TW, Smith RA. Oxidative stress in neurodegeneration and available means of protection. Front Biosci. 2008;13:3288–311.
Zhang H, Wang Y, Lyu D, Li Y, Li W, Wang Q, Li Y, Qin Q, Wang X, Gong M, Jiao H, Liu W, Jia J. Cerebral blood flow in mild cognitive impairment and Alzheimer’s disease: A systematic review and meta-analysis. Ageing Res Rev. 2021;71.
Studenski S, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50–8.
Ummarino S, et al. NAD modulates DNA methylation and cell differentiation. Cells. 2021;10(11).
Chang J, et al. Nicotinamide adenine dinucleotide (NAD)-regulated DNA methylation alters CCCTC-binding factor (CTCF)/cohesin binding and transcription at the BDNF locus. Proc Natl Acad Sci U S A. 2010;107(50):21836–41.
Acknowledgements
We would like to thank Beverly Orsak and Terry Romo for assisting with study coordination and patient visits, Rozmin Jiwani for assisting with study visits and Meghana Koleti for data entry; Crystal Franklin in the Research Imaging Institute staff for data curation and essential preprocessing steps. We also thank Dr. Brian Kennedy for offering valuable insights on experimental design.
Funding
Some authors were supported in part by funds from the National Institutes of Health (NIH South Texas Medical Scientist Training Program: T32GM113898, NIMH: R01MH074457-11S1, NIMH: R01MH074457, NCATS Translational Scientist Training Program: TL1TR002647-01). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
Research study design: MEO, PTF, NM, and BP; subject enrollment: DBK; conducted experiments: EK, DBK, MSS, YW, JG, and BP; provided reagents: CB; data analyses and interpretation: MEO, EK, PR, CB, PTF, JG, SE, BF, NM, and BP; drafted the manuscript: MEO, EK, and BP; critical revision: MEO, EK, CB, PTF, JG, SE, NM, and BP.
Corresponding author
Ethics declarations
Conflict of interest
ChromaDex Inc. provided the investigators with NR and placebo. Charles Brenner, a co-author, is an inventor of intellectual property on uses of nicotinamide riboside. He serves as Chief Scientific Advisor of ChromaDex and owns ChromaDex stock. Dr. Brenner’s contributions included data interpretation regarding NAD+ metabolites and manuscript editing. He was not involved in study design or execution. Dr. Orr reports a grant from US Department of Veterans Affairs during the conduct of the study. In addition, Dr. Orr has a patent biosignature and therapeutic approach for neuronal senescence pending outside the scope of this work. No other co-authors have COIs to declare.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 219 kb)
About this article
Cite this article
Orr, M.E., Kotkowski, E., Ramirez, P. et al. A randomized placebo-controlled trial of nicotinamide riboside in older adults with mild cognitive impairment. GeroScience 46, 665–682 (2024). https://doi.org/10.1007/s11357-023-00999-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-023-00999-9