Abstract
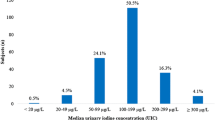
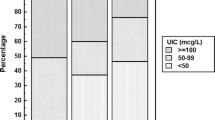
Children aged 3–6 years undergo a critical stage of growth and development and are irreversibly affected by their iodine status. In order to reveal iodine status in preschool children, we detected iodine concentrations in urine samples from 1382 children aged 3–6 years based on a cross-sectional study. The median urinary iodine concentration (UIC) of children was 193.36 μg/L and was 336.96 μg/g·Cr corrected for creatinine. The study developed a link between dietary habits and iodine status, revealing that regular calcium supplement (OR: 1.79, (95% CI: 1.03, 3.12)) increased deficiency risk, while moderate seafood consumption (OR: 0.60, (95% CI: 0.38, 0.95)) decreased it. Additionally, modest intake of shellfish (OR: 0.58, (95% CI: 0.33, 1.00)), vegetables (OR: 0.61, (95% CI: 0.38, 0.97)), and eggs (OR: 0.53, (95% CI: 0.30, 0.95)) was found to protect against excess iodine. The findings underline the importance of balanced diets and various nutrients’ roles in preschoolers’ iodine status.


Similar content being viewed by others
Data availability
The data that support the findings of this study are not openly available due to the inclusion of information that could compromise the subject’s privacy, but are available from the corresponding author on reasonable request.
References
Abt E, Spungen J, Pouillot R, Gamalo-Siebers M, Wirtz M (2018) Update on dietary intake of perchlorate and iodine from U.S. food and drug administration's total diet study: 2008–2012. J Expo Sci Environ Epidemiol 28:21–30
Adu-Afarwuah S, Arnold CD, Maleta K, Ashorn P, Ashorn U, Jorgensen JM, Fan Y-M, Nkhoma M, Bendabenda J, Matchado A, Dewey KG (2021) Consumption of multiple micronutrients or small-quantity lipid-based nutrient supplements containing iodine at the recommended dose during pregnancy, compared with iron and folic acid, does not affect women’s urinary iodine concentration in rural Malawi: a secondary outcome analysis of the iLiNS DYAD trial. Public Health Nutr 24:3049–3057
Andersson M, Karumbunathan V, Zimmermann MB (2012) Global iodine status in 2011 and trends over the past decade. J Nutr 142:744–750
Beer RJ, Herrán OF, Villamor E (2021) Median urinary iodine concentration in Colombian children and women is high and related to sociodemographic and geographic characteristics: results from a nationally representative survey. J Nutr 151:940–948
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R, Uauy R (2013) Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 382:427–451
Carlsen MH, Andersen LF, Dahl L, Norberg N, Hjartåker A (2018) New iodine food composition database and updated calculations of iodine intake among Norwegians. Nutrients 10(7):930. https://doi.org/10.3390/nu10070930
Censi S, Manso J, Barollo S, Mondin A, Bertazza L, De Marchi M, Mian C, On Behalf Of The Food And Nutrition Hygiene Services Sian (2020) Changing dietary habits in veneto region over two decades: still a long road to go to reach an iodine-sufficient status. Nutrients 12(8):2399. https://doi.org/10.3390/nu12082399
Cesar JA, S Santos IS, Black RE, Chrestani MAD, Duarte FA, Nilson EAF (2020) Iodine status of Brazilian school-age children: a national cross-sectional survey. Nutrients 12(4):1077. https://doi.org/10.3390/nu12041077
Copyright © World Health Organization (2014) Geneva
Costa Leite J, Keating E, Pestana D, Cruz Fernandes V, Maia ML, Norberto S, Pinto E, Moreira-Rosário A, Sintra D, Moreira B, Costa A, Silva S, Costa V, Martins I, Castro Mendes F, Queirós P, Peixoto B, Carlos Caldas J, Guerra A, Fontoura M, Calhau C (2017) Iodine status and iodised salt consumption in Portuguese school-aged children: The iogeneration study. Nutrients 9(5):458. https://doi.org/10.3390/nu9050458
Delange F (2002) Iodine deficiency in Europe and its consequences: an update. Eur J Nucl Med Mol Imaging 29(Suppl 2):S404–S416
Dineva M, Rayman MP, Bath SC (2021) Iodine status of consumers of milk-alternative drinks v. cows' milk: data from the UK National Diet and Nutrition Survey. Br J Nutr 126:28–36
Eftekhari MH, Simondon KB, Jalali M, Keshavarz SA, Elguero E, Eshraghian MR, Saadat N (2006) Effects of administration of iron, iodine and simultaneous iron-plus-iodine on the thyroid hormone profile in iron-deficient adolescent Iranian girls. Eur J Clin Nutr 60:545–552
Ershow AG, Skeaff SA, Merkel JM, Pehrsson PR (2018) Development of databases on Iodine in foods and dietary supplements. Nutrients 10(1):100. https://doi.org/10.3390/nu10010100
Farebrother J, Zimmermann MB, Andersson M (2019) Excess iodine intake: sources, assessment, and effects on thyroid function. Ann NY Acad Sci 1446:44–65
Felker P, Bunch R, Leung AM (2016) Concentrations of thiocyanate and goitrin in human plasma, their precursor concentrations in brassica vegetables, and associated potential risk for hypothyroidism. Nutr Rev 74:248–258
Fuse Y, Ito Y, Shishiba Y, Irie M (2022) Current iodine status in Japan: a cross-sectional nationwide survey of schoolchildren, 2014–2019. J Clin Endocrinol Metab 107:e2065–e2079
Ghattas H, Francis S, El Mallah C, Shatila D, Merhi K, Hlais S, Zimmermann M, Obeid O (2017) Lebanese children are iodine deficient and urinary sodium and fluoride excretion are weak positive predictors of urinary iodine. Eur J Nutr 56:749–755
Gostas DE, Larson-Meyer DE, Yoder HA, Huffman AE, Johnson EC (2020) Dietary relationship with 24 h urinary iodine concentrations of young adults in the mountain west region of the United States. Nutrients 12(1):121. https://doi.org/10.3390/nu12010121
Haldimann M, Alt A, Blanc A, Blondeau K (2005) Iodine content of food groups. J Food Compos Anal 18:461–471
Hess SY, Pearce EN (2023) Iodine: Physiology, dietary sources, and requirements. In: Caballero B (ed) Encyclopedia of human nutrition (fourth edition). Academic Press, Oxford, pp 273–281
Huang CJ, Tseng CL, Chen HS, Garabwan C, Korovo S, Tang KT, Won JG, Hsieh CH, Wang FF (2016) Iodine nutritional status of school children in Nauru 2015. Nutrients 8(9):520. https://doi.org/10.3390/nu8090520
Jayatissa R, Okosieme OE, Ranasinghe S, Carter JL, Gunatunga IP, Lazarus JH, Premawardhana LD (2021) Thyroid autoimmunity and dysfunction in Sri Lankan children and adolescents after 22 years of sustained universal salt iodization. Thyroid 31:1105–1113
Johner SA, Thamm M, Nöthlings U, Remer T (2013) Iodine status in preschool children and evaluation of major dietary iodine sources: a German experience. Eur J Nutr 52:1711–1719
Khatiwada S, Lamsal M, Gelal B, Gautam S, Nepal AK, Brodie D, Baral N (2016) Anemia, iron deficiency and iodine deficiency among Nepalese school children. Indian J Pediatr 83:617–621
Krzepiłko A, Zych-Wężyk I, Molas J (2015) Alternative ways of enriching the human diet with iodine. J Pre Clin Clin Res. 9:167–171
Laillou A, Sophonneary P, Kuong K, Hong R, Un S, Chamnan C, Poirot E, Berger J, Wieringa F (2016) Low urinary iodine concentration among mothers and children in Cambodia. Nutrients 8:172
Lee J, Kim JH, Lee SY, Lee JH (2014) Iodine status in Korean preschool children as determined by urinary iodine excretion. Eur J Nutr 53:683–688
Lee KW, Shin D, Cho MS, Song WO (2016) Food group intakes as determinants of iodine status among US adult population. Nutrients 8(6):325. https://doi.org/10.3390/nu8060325
Lee SY, Leung AM, He X, Braverman LE, Pearce EN (2010) Iodine content in fast foods: comparison between two fast-food chains in the United States. Endocr Pract 16(6):1071–1072. https://doi.org/10.4158/EP10180.CO
Leung AM, LaMar A, He X, Braverman LE, Pearce EN (2011) Iodine status and thyroid function of Boston-area vegetarians and vegans. J Clin Endocrinol Metab 96:E1303–E1307
Leung AM, Braverman LE (2014) Consequences of excess iodine. Nat Rev Endocrinol 10:136–142
Liu Z, Lin Y, Wu J, Chen D, Wu X, Lan Y, Chen Z (2022) Is the urinary iodine/creatinine ratio applicable to assess short term individual iodine status in Chinese adults? Comparison of iodine estimates from 24-h urine and timed-spot urine samples in different periods of the day. Nutr Metab (Lond) 19:27
Löf C, Sukumaran P, Viitanen T, Vainio M, Kemppainen K, Pulli I, Näsman J, Kukkonen JP, Törnquist K (2012) Communication between the calcium and cAMP pathways regulate the expression of the TSH receptor: TRPC2 in the Center of Action. Mol Endocrinol 26:2046–2057
Montenegro-Bethancourt G, Johner SA, Stehle P, Neubert A, Remer T (2015a) Iodine status assessment in children: spot urine iodine concentration reasonably reflects true twenty-four-hour iodine excretion only when scaled to creatinine. Thyroid 25:688–697
Montenegro-Bethancourt G, Johner SA, Stehle P, Neubert A, Remer T (2015b) Iodine status assessment in children: spot urine iodine concentration reasonably reflects true twenty-four-hour iodine excretion only when scaled to creatinine. Thyroid 25:688–697
Muñoz-Serrano A, González-González A, Tenías-Burillo JM, Falero-Gallego P, Cañete R (2014) Iodine-deficiency levels in school children aged between 6 and 12. Horm Res Paediatr 82:313
Nazeri P, Dalili H, Mehrabi Y, Hedayati M, Mirmiran P, Azizi F (2018) Breast milk iodine concentration rather than maternal urinary iodine is a reliable indicator for monitoring iodine status of breastfed neonates. Biol Trace Elem Res 185:71–77
Nerhus I, Wik Markhus M, Nilsen BM, Øyen J, Maage A, Ødegård ER, Midtbø LK, Frantzen S, Kögel T, Graff IE, Lie Ø, Dahl L, Kjellevold M (2018) Iodine content of six fish species, Norwegian dairy products and hen's egg. Food Nutr Res 62. https://doi.org/10.29219/fnr.v62.1291
Nerhus I, Odland M, Kjellevold M, Midtbø LK, Markhus MW, Graff IE, Lie Ø, Kvestad I, Frøyland L, Dahl L, Øyen J (2019) Iodine status in Norwegian preschool children and associations with dietary iodine sources: the FINS-KIDS study. Eur J Nutr 58:2219–2227
O’Kane SM, Mulhern MS, Pourshahidi LK, Strain JJ, Yeates AJ (2018) Micronutrients, iodine status and concentrations of thyroid hormones: a systematic review. Nutr Rev 76:418–431
Ovadia YS, Arbelle JE, Gefel D, Brik H, Wolf T, Nadler V, Hunziker S, Zimmermann MB, Troen AM (2017) First Israeli national iodine survey demonstrates iodine deficiency among school-aged children and pregnant women. Thyroid 27:1083–1091
Pearce EN, Pino S, He X, Bazrafshan HR, Lee SL, Braverman LE (2004) Sources of dietary iodine: bread, cows’ milk, and infant formula in the Boston area. J Clin Endocrinol Metab 89:3421–3424
Pearce EN, Andersson M, Zimmermann MB (2013) Global iodine nutrition: where do we stand in 2013? Thyroid 23:523–528
Perrine CG, Cogswell ME, Swanson CA, Sullivan KM, Chen TC, Carriquiry AL, Dodd KW, Caldwell KL, Wang CY (2014) Comparison of population iodine estimates from 24-hour urine and timed-spot urine samples. Thyroid 24:748–757
Qin Y, Cifelli CJ, Agarwal S, Fugoni VL (2023) Dairy food consumption is beneficially linked with iodine status in US children and adults: National Health and Nutrition Examination Surveys 2001-2018. Public Health Nutr 26(9):1828–1839. https://doi.org/10.1017/S136898002300071X
Remer T, Fonteyn N, Alexy U, Berkemeyer S (2006) Longitudinal examination of 24-h urinary iodine excretion in schoolchildren as a sensitive, hydration status-independent research tool for studying iodine status. Am J Clin Nutr 83:639–646
Röttger AS, Halle I, Wagner H, Breves G, Dänicke S, Flachowsky G (2012) The effects of iodine level and source on iodine carry-over in eggs and body tissues of laying hens. Arch Anim Nutr 66:385–401
Sakai N, Esho OY, Mukai M (2022) Iodine concentrations in conventional and organic milk in the northeastern U.S. Dairy 3(2):211–219. https://doi.org/10.3390/dairy3020017
Shan X, Liu C, Luo X, Zou Y, Huang L, Zhou W, Qin Q, Mao D, Li M, Yang L (2021) Iodine nutritional status and related factors among Chinese school-age children in three different areas: a cross-sectional study. Nutrients 13(5):1404. https://doi.org/10.3390/nu13051404
Soldin OP (2002) Controversies in urinary iodine determinations. Clin Biochem 35:575–579
Stråvik M, Gustin K, Barman M, Skröder H, Sandin A, Wold AE, Sandberg AS, Kippler M, Vahter M (2021) Infant iodine and selenium status in relation to maternal status and diet during pregnancy and lactation. Front Nutr 8:733602. https://doi.org/10.3389/fnut.2021.733602
Stråvik M, Gustin K, Barman M, Levi M, Sandin A, Wold AE, Sandberg A-S, Kippler M, Vahter M (2023) Biomarkers of seafood intake during pregnancy—pollutants versus fatty acids and micronutrients. Environ Res 225:115576
Sun D, Codling K, Chang S, Zhang S, Shen H, Su X, Chen Z, Scherpbier RW, Yan J (2017) Eliminating iodine deficiency in China: achievements, challenges and global implications. Nutrients 9:361
Torres MT, Francés L, Vila L, Manresa JM, Falguera G, Prieto G, Casamitjana R, Toran P (2017) Iodine nutritional status of women in their first trimester of pregnancy in Catalonia. BMC Pregnancy Childbirth 17:249
Vanderpump MP, Lazarus JH, Smyth PP, Laurberg P, Holder RL, Boelaert K, Franklyn JA (2011a) Iodine status of UK schoolgirls: a cross-sectional survey. Lancet 377:2007–2012
Vanderpump MPJ, Lazarus JH, Smyth PP, Laurberg P, Holder RL, Boelaert K, Franklyn JA (2011b) Iodine status of UK schoolgirls: a cross-sectional survey. Lancet 377:2007–2012
Viitanen TM, Sukumaran P, Löf C, Törnquist K (2013) Functional coupling of TRPC2 cation channels and the calcium-activated anion channels in rat thyroid cells: implications for iodide homeostasis. J Cell Physiol 228:814–823
von Oettingen JE, Brathwaite TD, Carpenter C, Bonnell R, He X, Braverman LE, Pearce EN, Larco P, Larco NC, Jean-Baptiste E, Brown RS (2017) Population survey of iodine deficiency and environmental disruptors of thyroid function in young children in Haiti. J Clin Endocrinol Metab 102:644–651
Wang Z, Zang J, Shi Z, Zhu Z, Song J, Zou S, Jin W, Jia X, Guo C, Liu S (2019) Iodine status of 8 to 10 years old children within 20 years following compulsory salt iodization policy in Shanghai, China. Nutr J 18:63
Witard OC, Bath SC, Dineva M, Sellem L, Mulet-Cabero AI, van Dongen LH, Zheng JS, Valenzuela C, Smeuninx B (2022) Dairy as a source of iodine and protein in the UK: implications for human health across the life course, and future policy and research. Front Nutr 9:800559. https://doi.org/10.3389/fnut.2022.800559
World Health Oraganization (2014) WHO guidelines approved by the guidelines review committee, Guideline: fortification of food-grade salt with iodine for the prevention and control of iodine deficiency disorders. World Health Organization
Wu Y, Li X, Chang S, Liu L, Zou S, Hipgrave DB (2012) Variable iodine intake persists in the context of universal salt iodization in China. J Nutr 142:1728–1734
Zimmermann MB, Jooste PL, Pandav CS (2008) Iodine-deficiency disorders. Lancet 372:1251–1262
Zimmermann MB (2009) Iodine deficiency. Endocr Rev 30:376–408
Zimmermann MB, Andersson M (2021) Global endocrinology: global perspectives in endocrinology: coverage of iodized salt programs and iodine status in 2020. Eur J Endocrinol 185:R13–r21
Funding
This study received financial support from the National Key R&D Program of China (Grant No. 2017YFC1600500) and the National Basic Research Program of China (“973” Program; Grant No. 2012CB525001). The sponsor had no role in the study design, data analysis and interpretation, manuscript preparation, review, or approval.
Author information
Authors and Affiliations
Contributions
JL: conceptualization, formal analysis, writing original draft and editing. JL: methodology and software. YW: investigation, formal analysis, and visualization. AL: investigation and visualization. YW: formal analysis and software. YL: methodology and data curation. CY: conceptualization, supervised the study, writing—review and editing.
Corresponding author
Ethics declarations
Ethics approval
This research was approved by the Medical Ethics Committee of Xinhua Hospital affiliated with Shanghai Jiao Tong University School of Medicine, and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from children’s parents recruited in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, ., Liu, JX., Wang, YQ. et al. Iodine status and associated dietary factors among preschool children in Shanghai. Environ Sci Pollut Res 30, 121823–121833 (2023). https://doi.org/10.1007/s11356-023-30942-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-30942-6