Abstract
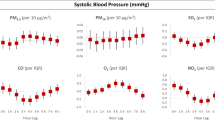
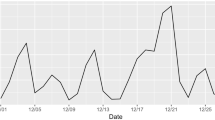
Published literature considering the association between ambient air pollution and blood pressure is highly inconsistent, which may be explained by the different proportions of susceptible subpopulations. We hypothesized that hypertensive patients are more sensitive to air pollution due to the disruption of neurohumoral system. The study aimed to reveal the association between PM2.5 and its carbon components and blood pressure, and whether this association is modified by hypertension status. We conducted a panel study in Beijing, China. Four repeated measurements were performed from 2016 to 2018. Linear mixed-effects models and generalized additive mixed models were performed to investigate the associations between PM2.5 and its carbon components and blood pressure. Subgroup analyses were performed by hypertension status to reveal potential effect modification. Among hypertensive patients, for every 1 μg/m3 increment of PM2.5, TC, OC, and EC in 1-day to 2-day MA, SBP increased from 0.16 mmHg (95% CI, 0.03 to 0.29) to 6.75 mmHg (95% CI, 2.82 to 10.68), and PP increased from 0.14 mmHg (95% CI, 0.02 to 0.26) to 6.03% (95% CI, 2.46 to 9.59%), but no significant association was observed among non-hypertensive subjects. The p values for the interaction between pollutants and hypertension status in 1-day to 2-day MA were less than 0.05. These findings suggest that hypertensive patients may be more susceptible to the adverse effects of air pollution than non-hypertensive subjects, which might provide guidance to hypertensive patients living in areas with high levels of particle pollution.




Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Abbreviations
- BP:
-
Blood pressure
- PM2.5 :
-
Particulate matter in aerodynamic diameter less than 2.5 μm
- OC:
-
Organic carbon
- EC:
-
Elemental carbon
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- PP:
-
Pulse pressure
- MAP:
-
Mean arterial pressure
- MA:
-
Moving average
- LME:
-
Linear mixed-effects
- GAMM:
-
Generalized additive mixed models
References
Bartoli CR, Wellenius GA, Diaz EA, Lawrence J, Coull BA, Akiyama I, Lee LM, Okabe K, Verrier RL, Godleski JJ (2009) Mechanisms of inhaled fine particulate air pollution-induced arterial blood pressure changes. Environ Health Perspect 117:361–366
Brook RD, Rajagopalan S, Pope CA 3RD, Brook JR., Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A, Siscovick D, Smith SC JR, Whitsel L, Kaufman JD, American Heart Association Council On, E., Prevention, C. O. T. K. I. C. D., Council On Nutrition, P. A. & Metabolism (2010) Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 121(21):2331-78
Chang LT, Chuang KJ, Yang WT, Wang VS, Chuang HC, Bao BY, Liu CS, Chang TY (2015) Short-term exposure to noise, fine particulate matter and nitrogen oxides on ambulatory blood pressure: a repeated-measure study. Environ Res 140:634–640
Choi YJ, Kim SH, Kang SH, Kim SY, Kim OJ, Yoon CH, Lee HY, Youn TJ, Chae IH, Kim CH (2019) Short-term effects of air pollution on blood pressure. Sci Rep 9:20298
Chung M, Wang D, Rizzo A, Gachette D, Delnord M, Parambi R, Kang C-M, Brugge D (2015) Association of PNC, BC, and PM2.5 measured at a central monitoring site with blood pressure in a predominantly near highway population. Int J Environ Res Public Health 12:2765–2780
Collaborators, G. B. D. R. F (2018) Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1923–1994
Curto A, Wellenius GA, Mila C, Sanchez M, Ranzani O, Marshall JD, Kulkarni B, Bhogadi S, Kinra S, Tonne C (2019) Ambient Particulate air pollution and blood pressure in peri-urban India. Epidemiology 30:492–500
Dvonch JT, Kannan S, Schulz AJ, Keeler GJ, Mentz G, House J, Benjamin A, Max P, Bard RL, Brook RD (2009) Acute effects of ambient particulate matter on blood pressure: differential effects across urban communities. Hypertension 53:853–859
Grassi G, Mark A, Esler M (2015) The sympathetic nervous system alterations in human hypertension. Circ Res 116:976–990
Harvey A, Montezano AC, Touyz RM (2015) Vascular biology of ageing-implications in hypertension. J Mol Cell Cardiol 83:112–121
Ibald-Mulli A, Timonen KL, Peters A, Heinrich J, Wolke G, Lanki T, Buzorius G, Kreyling WG, DE Hartog J, Hoek G, Ten Brink HM, Pekkanen J (2004) Effects of particulate air pollution on blood pressure and heart rate in subjects with cardiovascular disease: a multicenter approach. Environ Health Perspect 112:369–377
Kjeldsen SE, Narkiewicz K, Burnier M, Oparil S (2017) The global burden of disease study 2015 and blood pressure. Blood Press 26:1
Laurent S, Boutouyrie P (2015) The structural factor of hypertension: large and small artery alterations. Circ Res 116:1007–1021
Li A, Mei Y, Zhao M, Xu J, Li R, Zhao J, Zhou Q, Ge X, Xu Q (2021) Associations between air pollutant exposure and renal function: a prospective study of older adults without chronic kidney disease. Environ Pollut 277:116750
Li A, Mei Y, Zhao M, Xu J, Zhao J, Zhou Q, Ge X, Xu Q (2022) Do urinary metals associate with the homeostasis of inflammatory mediators? Results from the perspective of inflammatory signaling in middle-aged and older adults. Environ Int 163:107237
Li A, Pei L, Zhao M, Xu J, Mei Y, Li R, Xu Q (2019a) Investigating potential associations between O3 exposure and lipid profiles: a longitudinal study of older adults in Beijing. Environ Int 133:105135
Li W, Pei L, Li A, Luo K, Cao Y, Li R, Xu Q (2019b) Spatial variation in the effects of air pollution on cardiovascular mortality in Beijing, China. Environ Sci Pollut Res Int 26:2501–2511
Lin Z, Niu Y, Chen R, XU W, Li H, Liu C, Cai J, Zhao Z, Kan H, Qiao L (2017) Fine particulate matter constituents and blood pressure in patients with chronic obstructive pulmonary disease: a panel study in Shanghai, China. Environ Res 159:291–296
Lin Z, Wang X, Liu F, Yang X, Liu Q, Xing X, Cao J, Li J, Huang K, Yan W, Liu T, Fan M, Li W, Chen S, Lu X, Gu D, Huang J (2021) Impacts of short-term fine particulate matter exposure on blood pressure were modified by control status and treatment in hypertensive patients. Hypertension 78:174–183
Madsen C, Nafstad P (2006) Associations between environmental exposure and blood pressure among participants in the Oslo Health Study (HUBRO). Eur J Epidemiol 21:485–491
Mannisto T, Mendola P, Liu D, Leishear K, Sherman S, Laughon SK (2015) Acute air pollution exposure and blood pressure at delivery among women with and without hypertension. Am J Hypertens 28:58–72
Mccracken JP, Smith KR, Diaz A, Mittleman MA, Schwartz J (2007) Chimney stove intervention to reduce long-term wood smoke exposure lowers blood pressure among Guatemalan women. Environ Health Perspect 115:996–1001
Norris C, Goldberg MS, Marshall JD, Valois MF, Pradeep T, Narayanswamy M, Jain G, Sethuraman K, Baumgartner J (2016) A panel study of the acute effects of personal exposure to household air pollution on ambulatory blood pressure in rural Indian women. Environ Res 147:331–342
Oparil S, Acelajado MC, Bakris GL, Berlowitz DR, Cifkova R, Dominiczak AF, Grassi G, Jordan J, Poulter NR, Rodgers A, Whelton PK (2018) Hypertension. Nat Rev Dis Primers 4:18014
Pei L, Zhao M, Xu J, Li A, Luo K, Li R, Yang M, Xu Q (2019) Associations of ambient fine particulate matter and its constituents with serum complement C3 in a panel study of older adults in China. Environ Pollut 252:1019–1025
Ren M, Zhang H, Benmarhnia T, Jalaludin B, Dong H, Wu K, Wang Q, Huang C (2019) Short-term effects of real-time personal PM2.5 exposure on ambulatory blood pressure: a panel study in young adults. Sci Total Environ 697:134079
Rodriguez-Iturbe B, Pons H, Johnson RJ (2017) Role of the immune system in hypertension. Physiol Rev 97:1127–1164
Te Riet L, Van Esch JH, Roks AJ, Van Den Meiracker AH, Danser AH (2015) Hypertension: renin-angiotensin-aldosterone system alterations. Circ Res 116:960–975
Tong Y, Luo K, Li R, Pei L, Li A, Yang M, Xu Q (2018) Association between multi-pollutant mixtures pollution and daily cardiovascular mortality: an exploration of exposure-response relationship. Atmosp Environ 186:136–143
Versari D, Daghini E, Virdis A, Ghiadoni L, Taddei S (2009) Endothelium-dependent contractions and endothelial dysfunction in human hypertension. Br J Pharmacol 157:527–536
Xia B, Zhou Y, Zhu Q, Zhao Y, Wang Y, Ge W, Yang Q, Zhao Y, Wang P, Si J, Luo R, Li J, Shi H, Zhang Y (2019) Personal exposure to PM2.5 constituents associated with gestational blood pressure and endothelial dysfunction. Environ Pollut 250:346–356
Xia Y, Niu Y, Cai J, Lin Z, Liu C, Li H, Chen C, Song W, Zhao Z, Chen R, Kan H (2018) Effects of personal short-term exposure to ambient ozone on blood pressure and vascular endothelial function: a mechanistic study based on DNA methylation and metabolomics. Environ Sci Technol 52:12774–12782
Ying Z, Xu X, Bai Y, Zhong J, Chen M, Liang Y, Zhao J, Liu D, Morishita M, Sun Q, Spino C, Brook RD, Harkema JR, Rajagopalan S (2014) Long-term exposure to concentrated ambient PM2.5 increases mouse blood pressure through abnormal activation of the sympathetic nervous system: a role for hypothalamic inflammation. Environ Health Perspect 122:79–86
Zanobetti A, Canner MJ, Stone PH, Schwartz J, Sher D, Eagan-Bengston E, Gates KA, Hartley LH, Suh H, Gold DR (2004) Ambient pollution and blood pressure in cardiac rehabilitation patients. Circulation 110:2184–2189
Funding
This study was supported by the China Medical Board (Grant No. 15-230); the China Prospective cohort study of Air pollution and health effects in Typical areas (C-PAT) (Grant No. MEE-EH- 20190802).
Author information
Authors and Affiliations
Contributions
Xue Wang: data curation, software programming, writing—original draft preparation; Ang Li, Meiduo Zhao, Jing Xu, and Yayuan Mei: investigation; Qun Xu: conceptualization, supervision, project administration
Corresponding author
Ethics declarations
Ethics approval
This study was supported by the China Medical Board (Grant No. 15-230); the China Prospective cohort study of Air pollution and health effects in Typical areas (C-PAT) (Grant No. MEE-EH-20190802. Written informed consent was obtained prior to each visit after a complete description of the study was provided.
Consent to participate
Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Participants signed informed consent regarding publishing their data.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, ., Li, A., Zhao, M. et al. Differential effects of PM2.5 and its carbon components on blood pressure in hypertensive and non-hypertensive populations: a panel study in Beijing. Environ Sci Pollut Res 30, 123226–123236 (2023). https://doi.org/10.1007/s11356-023-30532-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-30532-6