Abstract
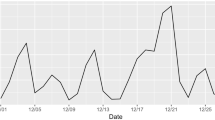
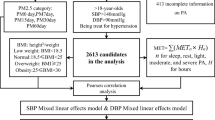
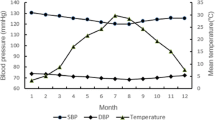
We aimed to examine PM2.5 exposure, blood pressure (SBP and DBP) measurement, and hypertension risk factors and to assess the association between PM2.5 exposure and hypertension among young adults. The mean SBP was 117.78 mmHg, with 11.22% high-normal blood pressure (prehypertension) and 2.51% hypertension (≥ 140 mmHg). DBP was 75.48 mmHg with 26.37% prehypertension and 4.53% hypertension (≥ 90 mmHg). The median PM2.5 in the past year was 31.79 μg/m3, with highest in winter (49.33 μg/m3), followed by spring (37.34 μg/m3), autumn (29.64 μg/m3), and summer (24.33 μg/m3). Blood pressure was positively correlated with age, height, weight, BMI, daily smoking, alcohol consumption, mental stress, and staying up in the past 1 year, and negatively with season-specific temperature. After adjustment for the covariates, each 10 μg/m3 increase in PM2.5 was associated with SBP (day 1 = 1.07 mmHg, day 3 = 1.25 mmHg, day 5 = 1.01 mmHg) and DBP (day 1 = 1.06 mmHg, day 3 = 1.28 mmHg, day 5 = 1.29 mmHg, day 15 = 0.87 mmHg, day 30 = 0.56 mmHg). Exposure in winter and the past year was associated with 1.21 mmHg and 0.95 increase mmHg in SBP, respectively. Logistic models showed for every 1 μg/m3 increase of PM2.5, SBP in day 1 and day 5 was increased by 6% and 4%, and DPB by 3% and 16%, respectively. SBP was increased by 8% in spring and 19% in winter, and DBP was increased by 7% in winter. Our data suggest a certain prevalence of pre- or hypertension among young population, which is associated with short-term fluctuation and season-specific exposure of PM2.5.



Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Baumgartner J, Schauer JJ, Ezzati M, Lu L, Cheng C, Patz JA, Bautista LE (2011) Indoor air pollution and blood pressure in adult women living in rural China. Environ Health Perspect 119:1390–1395
Braziene A, Tamsiunas A, Luksiene D, Radisauskas R, Andrusaityte S, Dedele A, Vencloviene J (2020) Association between the living environment and the risk of arterial hypertension and other components of metabolic syndrome. J Public Health (oxf) 42:e142–e149
Curto A, Wellenius GA, Mila C, Sanchez M, Ranzani O, Marshall JD, Kulkarni B, Bhogadi S, Kinra S, Tonne C (2019) Ambient particulate air pollution and blood pressure in peri-urban India. Epidemiology 30:492–500
Flack JM, Adekola B (2020) Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med 30:160–164
Hicken MT, Dvonch JT, Schulz AJ, Mentz G, Max P (2014) Fine particulate matter air pollution and blood pressure: the modifying role of psychosocial stress. Environ Res 133:195–203
Li MH, Fan LC, Mao B, Yang JW, Choi AMK, Cao WJ, Xu JF (2016) Short-term exposure to ambient fine particulate matter increases hospitalizations and mortality in COPD: a systematic review and meta-analysis. Chest 149:447–458
Lurbe E, Torro I, Alvarez J, Aguilar F, Mancia G, Redon J, Redon P (2019) Impact of ESH and AAP hypertension guidelines for children and adolescents on office and ambulatory blood pressure-based classifications. J Hypertens 37:2414–2421
Qi Y, Han X, Zhao D, Wang W, Wang M, Sun J, Liu J, Li Y, Gao S, Hao Y, Deng Q, Liu J (2018) Long-term cardiovascular risk associated with stage 1 hypertension defined by the 2017 ACC/AHA hypertension guideline. J Am Coll Cardiol 72:1201–1210
Rabito FA, Yang Q, Zhang H, Werthmann D, Shankar A, Chillrud S (2020) The association between short-term residential black carbon concentration on blood pressure in a general population sample. Indoor Air 30:767–775
Ren M, Zhang H, Benmarhnia T, Jalaludin B, Dong H, Wu K, Wang Q, Huang C (2019) Short-term effects of real-time personal PM2.5 exposure on ambulatory blood pressure: a panel study in young adults. Sci Total Environ 697:134079
Shen Y, Chang C, Zhang J, Jiang Y, Ni B, Wang Y (2017) Prevalence and risk factors associated with hypertension and prehypertension in a working population at high altitude in China: a cross-sectional study. Environ Health Prev Med 22:19
Tan C, Wang Y, Lin M, Wang Z, He L, Li Z, Li Y, Xu K (2018) Long-term high air pollution exposure induced metabolic adaptations in traffic policemen. Environ Toxicol Pharmacol 58:156–162
Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, Shao L, Tian Y, Dong Y, Zheng C, Wang J, Zhu M, Weintraub WS, Gao R, China Hypertension Survey, I (2018) Status of hypertension in China: results from the China Hypertension Survey, 2012–2015. Circulation 137:2344–2356
Wang Q, Gan X, Li F, Chen Y, Fu W, Zhu X, Xu D, Long M, Xu D (2019a) PM2.5 exposure induces more serious apoptosis of cardiomyocytes mediated by Caspase3 through JNK/ P53 pathway in hyperlipidemic rats. Int J Biol Sci 15:24–33
Wang X, Zou Z, Dong B, Dong Y, Ma Y, Gao D, Yang Z, Wu S, Ma J (2019b) Association of school residential PM2.5 with childhood high blood pressure: results from an observational study in 6 cities in China. Int J Environ Res Public Health 16:2515
Wellenius GA, Boyle LD, Wilker EH, Sorond FA, Coull BA, Koutrakis P, Mittleman MA, Lipsitz LA (2013) Ambient fine particulate matter alters cerebral hemodynamics in the elderly. Stroke 44:1532–1536
Yan M, Xu J, Li C, Guo P, Yang X, Tang NJ (2021) Associations between ambient air pollutants and blood pressure among children and adolescents: a systemic review and meta-analysis. Sci Total Environ 785:147279
Yin R, Yin L, Li L, Silva-Nash J, Tan J, Pan Z, Zeng J, Yan LL (2021) Hypertension in China: burdens, guidelines and policy responses: a state-of-the-art review. J Hum Hypertens 1–9
Ying Z, Xu X, Bai Y, Zhong J, Chen M, Liang Y, Zhao J, Liu D, Morishita M, Sun Q, Spino C, Brook RD, Harkema JR, Rajagopalan S (2014) Long-term exposure to concentrated ambient PM2.5 increases mouse blood pressure through abnormal activation of the sympathetic nervous system: a role for hypothalamic inflammation. Environ Health Perspect 122:79–86
Zeng Y, Lin C, Guo C, Bo Y, Chang LY, Lau AKH, Tam T, Yu Z, Lao XQ (2021) Combined effects of chronic PM2.5 exposure and habitual exercise on renal function and chronic kidney disease: a longitudinal cohort study. Int J Hyg Environ Health 236:113791
Zhang Q, Zheng Y, Tong D, Shao M, Wang S, Zhang Y, Xu X, Wang J, He H, Liu W, Ding Y, Lei Y, Li J, Wang Z, Zhang X, Wang Y, Cheng J, Liu Y, Shi Q, Yan L, Geng G, Hong C, Li M, Liu F, Zheng B, Cao J, Ding A, Gao J, Fu Q, Huo J, Liu B, Liu Z, Yang F, He K, Hao J (2019) Drivers of improved PM2.5 air quality in China from 2013 to 2017. Proc Natl Acad Sci U S A 116:24463–24469
Zhang J, Cai L, Gui Z, Wang S, Zeng X, Lai L, Lv Y, Tan K, Wang H, Huang C, Chen Y (2020) Air pollution-associated blood pressure may be modified by diet among children in Guangzhou, China. J Hypertens 38:2215–2222
Zhao Y, Jin L, Chi Y, Yang J, Zhen Q, Wu H (2019a) Fine particulate matter leads to unfolded protein response and shortened lifespan by inducing oxidative stress in C. elegans. Oxid Med Cell Longev 2019:2492368
Zhao Z, Lv S, Zhang Y, Zhao Q, Shen L, Xu S, Yu J, Hou J, Jin C (2019b) Characteristics and source apportionment of PM2.5 in Jiaxing, China. Environ Sci Pollut Res Int 26:7497–7511
Zheng S, Zhu W, Wang M, Shi Q, Luo Y, Miao Q, Nie Y, Kang F, Mi X, Bai Y (2020) The effect of diurnal temperature range on blood pressure among 46,609 people in Northwestern China. Sci Total Environ 730:138987
Zhou X, Cao Z, Ma Y, Wang L, Wu R, Wang W (2016) Concentrations, correlations and chemical species of PM2.5/PM10 based on published data in China: potential implications for the revised particulate standard. Chemosphere 144:518–526
Acknowledgements
We appreciate the help of the Top-level Talent Project of Zhejiang Province, and apologize to all those researchers whose work could not be cited due to space limitations.
Funding
This work was financially supported by the Sci-Tech Planning Project of Jiaxing, China (2019AY32010 to Xu L), and the Student Research Training Project of Jiaxing University (CD8517193191 to Xu L).
Author information
Authors and Affiliations
Contributions
Huaze Ye: questionnaire design, survey, collection and project implementation; Jie Tang: conceptualize the idea, statistical analysis, paper draft; Leiqin Luo: questionnaire design, survey, collection, project implementation, data analysis; Tianjian Yang: questionnaire collection, PM2.5 data collection; Kedi Fan: questionnaire collection, PM2.5 data collection; Long Xu: conceptualize the idea, financial support, statistical analysis, editing the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Human Ethical Committee of Jiaxing University Medical College (JUMC-IRB-2018), and the informed consent was given to all subjects prior to research.
Consent to publish
All participants consented to publish.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ye, H., Tang, J., Luo, L. et al. High-normal blood pressure (prehypertension) is associated with PM2.5 exposure in young adults. Environ Sci Pollut Res 29, 40701–40710 (2022). https://doi.org/10.1007/s11356-022-18862-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-022-18862-3