Abstract
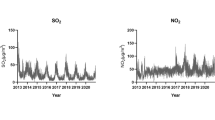
Considering the increasing rate of hospitalization due to the symptoms intensification, and the increasing trend of air pollution, this study aimed to determine the relationship between the amount of air pollutants and the incidence of cardiovascular disease leading to hospitalization. This case-crossover study was carried out on the data of admitted patients with cardiovascular disease such as hypertension, ischemic heart disease, and cerebrovascular disease in Urmia during 2011–2016. Weather data about air pollutants (NO2, PM10, SO2, and CO) were obtained from the meteorological department of Urmia. The data were coded for each patient and matched with the meteorological data for statistical modeling. The data were analyzed through STATA version 14. Conditional logistic regression was used to estimate the effects of air pollutants on cardiovascular disease adjusted to air temperature, relative humidity, and air pollutants. The final analysis was performed on 43,424 patients with cardiovascular disease using code I10-I99 including ischemic heart disease, hypertension, and cerebrovascular disease adjusted to air temperature and relative humidity. Of all pollutants, CO with each increase 10 μg/m3 had a meaningful relationship with the incidence of cardiovascular hospitalization. By selecting the window of exposure, 1, 2, and 6 days before admission, lag 6 (6 days) was the best estimation for exposure time in the patients with cardiovascular patients (OR 1.0056, CI 1.0041–1.007), and in the patients with ischemic heart disease (OR 1.000055, CI 1.000036–1.000075) and in the patients with hypertension (OR 1.000076, CI 1.00002–1.000132). Regarding cerebrovascular disease, no statistically significant association was observed. The results showed that only CO was associated with an increased risk of admission in patients with cardiovascular disease, ischemic heart disease, and hypertension, and there was no clear evidence for pollution effects on cerebrovascular diseases.


Similar content being viewed by others
Data availability
Due to the fact that access to hospital data is subject to certain conditions and is not freely available to the public, so we went to Seyed Al-Shohada, Taleghani, and Imam Khomeini hospitals for access with the permission of the management. Weather data about air pollutants (NO2, PM10, SO2, and CO) were obtained from meteorological department of Urmia. I can provide you with all the raw data information that I have received from the mentioned sources immediately if needed. Sites that I visited with permission and was able to access raw data.
https://taleghani.umsu.ac.ir/index.aspx?fkeyid=&siteid=22&pageid=13267
References
Atkinson RW, Anderson HR, Sunyer J, Ayres J, Baccini M, Vonk JM, Boumghar A, Forastiere F, Forsberg B, Touloumi G (2001) Acute effects of particulate air pollution on respiratory admissions: results from APHEA 2 project. Am J Respir Crit Care Med 164(10):1860–1866
Azizi F, Hatami H, Janghorbani M (2000) Epidemiology and control of common diseases in Iran. Eshtiagh Publications, Tehran, pp 602–616
Azizi F, Rahmani M, Emami H, Mirmiran P, Hajipour R, Madjid M, Ghanbili J, Ghanbarian A, Mehrabi J, Saadat N (2002) Cardiovascular risk factors in an Iranian urban population: Tehran lipid and glucose study (phase 1). Sozial-und Präventivmedizin 47(6):408–426
Barros AJ, Hirakata VN (2003) Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 3(1):21
Bateson TF, Schwartz J (1999) Control for seasonal variation and time trend in case-crossover studies of acute effects of environmental exposures. Epidemiology 10:539–544
Bateson TF, Schwartz J (2001) Selection bias and confounding in case-crossover analyses of environmental time-series data. Epidemiology 12(6):654–661
Bhaskaran K, Wilkinson P, Smeeth L (2011) Cardiovascular consequences of air pollution: what are the mechanisms? BMJ Publishing Group Ltd.
Brook RD, Franklin B, Cascio W, Hong Y, Howard G, Lipsett M, Luepker R, Mittleman M, Samet J, Smith SC Jr (2004) Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation 109(21):2655–2671
Burnett RT, Smith-Doiron M, Stieb D, Cakmak S, Brook JR (1999) Effects of particulate and gaseous air pollution on cardiorespiratory hospitalizations. Arch Environ Health 54(2):130–139
Carson C, Hajat S, Armstrong B, Wilkinson P (2006) Declining vulnerability to temperature-related mortality in London over the 20th century. Am J Epidemiol 164(1):77–84
Chen C-H, Chan C-C, Chen B-Y, Cheng T-J, Guo YL (2015) Effects of particulate air pollution and ozone on lung function in non-asthmatic children. Environ Res 137:40–48
Cheng M-H, Chiu H-F, Yang C-Y (2015) Coarse particulate air pollution associated with increased risk of hospital admissions for respiratory diseases in a tropical city, Kaohsiung, Taiwan. Int J Environ Res Public Health 12(10):13053–13068
Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, Friel S, Groce N, Johnson A, Kett M (2009) Managing the health effects of climate change: lancet and University College London Institute for Global Health Commission. Lancet 373(9676):1693–1733
Di Nardo F, Laurenti P (2015) Respiratory diseases and health disorders related to indoor and outdoor air pollution. A Systematic Review of Key Issues in Public Health, Springer, pp 109–127
Frampton MW, Pietropaoli A, Dentler M, Chalupa D, Little EL, Stewart J, Frasier L, Oakes D, Wiltshire J, Vora R (2015) Cardiovascular effects of ozone in healthy subjects with and without deletion of glutathione-S-transferase M1. Inhal Toxicol 27(2):113–119
Goudarzi G, Geravandi S, Foruozandeh H, Babaei AA, Alavi N, Niri MV, Khodayar MJ, Salmanzadeh S, Mohammadi MJ (2015) Cardiovascular and respiratory mortality attributed to ground-level ozone in Ahvaz, Iran. Environ Monit Assess 187(8):487
Goudarzi G, Geravandi S, Salmanzadeh S, Zallaghi E (2014) The number of myocardial infarction and cardiovascular death cases associated with sulfur dioxide exposure in Ahvaz, Iran. Arch Hygiene Sci 3(3):112–119
Jaakkola J (2003) Case-crossover design in air pollution epidemiology. Eur Respir J 21(40 suppl):81s–85s
Janes H, Sheppard L, Lumley T (2005) Overlap bias in the case-crossover design, with application to air pollution exposures. Stat Med 24(2):285–300
Katsouyanni K, Samet JM, Anderson HR, Atkinson R, Le AT, Medina S, Samoli E, Touloumi G, Burnett RT, Krewski D (2009) Air pollution and health: a European and North American approach (APHENA). Res Rep Health Eff Inst (142):5–90
Lee B-J, Kim B, Lee K (2014) Air pollution exposure and cardiovascular disease. Toxicol Res 30(2):71–75
Lee J-T, Schwartz J (1999) Reanalysis of the effects of air pollution on daily mortality in Seoul, Korea: a case-crossover design. Environ Health Perspect 107(8):633–636
Ljungman PL, Mittleman MA (2014) Ambient air pollution and stroke. Stroke 45(12):3734–3741
Lorenzo C, Williams K, Hunt KJ, Haffner SM (2007) The National Cholesterol Education Program–Adult Treatment Panel III, International Diabetes Federation, and World Health Organization definitions of the metabolic syndrome as predictors of incident cardiovascular disease and diabetes. Diabetes Care 30(1):8–13
Lumley T, Levy D (2000) Bias in the case–crossover design: implications for studies of air pollution. Environmetrics 11(6):689–704
Maclure M, Mittleman MA (2000) Should we use a case-crossover design? Annu Rev Public Health 21(1):193–221
Milojevic A, Wilkinson P, Armstrong B, Bhaskaran K, Smeeth L, Hajat S (2014) Short-term effects of air pollution on a range of cardiovascular events in England and Wales: case-crossover analysis of the MINAP database, hospital admissions and mortality. Heart 100(14):1093–1098
Navidi W (1998) Bidirectional case-crossover designs for exposures with time trends. Biometrics 54:596–605
Nawrot TS, Perez L, Künzli N, Munters E, Nemery B (2011) Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet 377(9767):732–740
Neas LM, Schwartz J, Dockery D (1999) A case-crossover analysis of air pollution and mortality in Philadelphia. Environ Health Perspect 107(8):629–631
Nhung NTT, Amini H, Schindler C, Joss MK, Dien TM, Probst-Hensch N, Perez L, Künzli N (2017) Short-term association between ambient air pollution and pneumonia in children: a systematic review and meta-analysis of time-series and case-crossover studies. Environ Pollut 230:1000–1008
Organization WH (2014) “Ambient (outdoor) air quality and health. Fact Sheet No 313.” EU Commission, Mobility and Transport. Retrieved from http://www.who.int/mediacentre/factsheets/fs313/en/. Accessed on January 14: 201
Pope C 3rd (2000) Epidemiology of fine particulate air pollution and human health: biologic mechanisms and who's at risk? Environ Health Perspect 108(suppl 4):713–723
Porta M (2014) A dictionary of epidemiology. Oxford university press
Rezaeian M, Tabatabaei Z, Naeimi R, Esmaeili A, Jamali M, VaziriNejad R, Nouri E (2007) Knowledge, attitude and practice of Rafsanjan male pensioners towards prevention of prostate cancer in the year 2006. Horizon Med Sci 12(4):19–25
Samet JM, Zeger SL, Dominici F, Curriero F, Coursac I, Dockery DW, Schwartz J, Zanobetti A (2000) “The national morbidity, mortality, and air pollution study.” Part II: morbidity and mortality from air pollution in the United States. Res Rep Health Eff Inst 94(pt 2):5–79
Schwartz J, Morris R (1995) Air pollution and hospital admissions for cardiovascular disease in Detroit, Michigan. Am J Epidemiol 142(1):23–35
Shah AS, Lee KK, McAllister DA, Hunter A, Nair H, Whiteley W, Langrish JP, Newby DE, Mills NL (2015) Short term exposure to air pollution and stroke: systematic review and meta-analysis. bmj 350:h1295
Szklo M, Nieto FJ, Miller D (2001) Epidemiology: beyond the basics. Oxford University Press
Urch B, Silverman F, Corey P, Brook JR, Lukic KZ, Rajagopalan S, Brook RD (2005) Acute blood pressure responses in healthy adults during controlled air pollution exposures. Environ Health Perspect 113(8):1052–1055
Wing JJ, Adar SD, Sánchez BN, Morgenstern LB, Smith MA, Lisabeth LD (2017) Short-term exposures to ambient air pollution and risk of recurrent ischemic stroke. Environ Res 152:304–307
Xu X, Ha SU, Basnet R (2016) A review of epidemiological research on adverse neurological effects of exposure to ambient air pollution. Front Public Health 4:157
Yang W-S, Wang X, Deng Q, Fan W-Y, Wang W-Y (2014) An evidence-based appraisal of global association between air pollution and risk of stroke. Int J Cardiol 175(2):307–313
Yitshak Sade M, Novack V, Ifergane G, Horev A, Kloog I (2015) Air pollution and ischemic stroke among young adults. Stroke 46(12):3348–3353
Acknowledgments
This article was extracted from research project approved by Iran University of Medical Sciences in 2017 with ethical code IR.IUMS.REC 1396.32421. Also, the authors would like to thank the department of environment of West Azerbaijan Province as well as Imam Khomeini, Taleghani and Seyyid al-Shohada hospitals for preparing the basic information.
Author information
Authors and Affiliations
Contributions
LS: She analyzed and interpreted the patient data regarding the cardiovascular disease and the transplant.
ShR: She was a major contributor in writing the manuscript.
BH: He was a major contributor in writing the manuscript.
MK: He was a major contributor in writing the manuscript.
LJ: I analyzed and interpreted the patient data regarding the cardiovascular and am a major contributor in writing the manuscript.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclaimer
Iran University of Medical Sciences (Tehran) was in charge of the role of the power supply institution in designing the study and collecting experiences and analyzing and interpreting the data and writing the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable
Consent to participate
Not applicable
Consent to publish
Not applicable
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
What is “already known” in this topic:
Air pollution in Urmia, especially in the recent decade, has imposed serious problems on the society’s health. The results showed that CO was associated with high risk of admission in patients with cardiovascular disease, ischemic heart disease, and hypertension, but there was no clear evidence for pollution effects on cerebrovascular diseases.
What this article adds:
So far, no assessment has been done about the consequences of air pollution on the health of residents of Urmia during the last decade. This study used the WHO approach and STATA software. Air pollution impacts health, and thus, its assessment is highly important to help authorities and managers for making decision in this regard. Specialists should focus on air pollution to reduce it.
Rights and permissions
About this article
Cite this article
Sokoty, L., Rimaz, S., Hassanlouei, B. et al. Short-term effects of air pollutants on hospitalization rate in patients with cardiovascular disease: a case-crossover study. Environ Sci Pollut Res 28, 26124–26131 (2021). https://doi.org/10.1007/s11356-021-12390-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-12390-2