Abstract
Background
Hemolysis in sickle cell disease (SCD) releases cell free hemoglobin, which scavenges nitric oxide (NO), leading to pulmonary vascular vasoconstriction, increased pulmonary vascular resistance (PVR), and the development of PH. However, PVR is only one component of right ventricular (RV) afterload. Whether sickled red blood cells increase the total RV afterload, including compliance and wave reflections, is unclear.
Objective
Patients with SCD and pulmonary hypertension (PH) have a significantly increased risk of sudden death compared to patients with SCD alone. Sickled red blood cells (RBCs) are fragile and lyse easily. Here, we sought to determine the acute effects of SCD RBCs and increased cell free hemoglobin on RV afterload.
Methods
Main pulmonary artery pressures and flows were measured in C57BL6 mice before and after exchanges of whole blood (~200 uL, Hct = 45%) with an equal volume of SCD RBCs in plasma (Hct = 45%) or cell free hemoglobin (Hb+) in solution. After transfusions, animals were additionally stressed with acute hypoxia (AH; 10% O2).
Results
SCD RBCs increased PVR only compared to control RBCs; cell free hemoglobin increased PVR and wave reflections. These increases in RV afterload increased further with AH.
Conclusions
The release of cell free hemoglobin from fragile SCD RBCs in vivo increases the total RV afterload and may impair RV function more than the SCD RBCs themselves.




Similar content being viewed by others
References
Organization W.H (2006) Sickle-cell anaemia: Report by the Secretariat. 59th World Health Assembly. 11
Machado RF, Farber HW (2013) Pulmonary hypertension associated with chronic hemolytic anemia and other blood disorders. Clin Chest Med 34(4):739–752
Maciaszek JL, Andemariam B, Lykotrafitis G (2011) Microelasticity of red blood cells in sickle cell disease. J Strain Anal Eng Des 46(5):368–379
Bunn HF, Nathan DG, Dover GJ, Hebbel RP, Platt OS, Rosse WF, Ware RE (2010) Pulmonary hypertension and nitric oxide depletion in sickle cell disease. Blood 116(5):687–692
Gaggar A, Patel RP (2016) There is blood in the water: hemolysis, hemoglobin, and heme in acute lung injury. Am J Physiol Lung Cell Mol Physiol 311(4):L714–l718
Ataga KI, Sood N, de Gent G, Kelly E, Henderson AG, Jones S, Strayhorn D, Lail A, Lieff S, Orringer EP (2004) Pulmonary hypertension in sickle cell disease. Am J Med 117(9):665–669
De Castro LM et al (2008) Pulmonary hypertension associated with sickle cell disease: clinical and laboratory endpoints and disease outcomes. Am J Hematol 83(1):19–25
Gordeuk VR, Castro OL, Machado RF (2016) Pathophysiology and treatment of pulmonary hypertension in sickle cell disease. Blood 127(7):820–828
Haque AK, Gokhale S, Rampy BA, Adegboyega P, Duarte A, Saldana MJ (2002) Pulmonary hypertension in sickle cell hemoglobinopathy: a clinicopathologic study of 20 cases. Hum Pathol 33(10):1037–1043
Ander S, MacLennan M, Bentil S, Leavitt B, Chesler N (2005) Pressure-induced vector transport in human saphenous vein. Ann Biomed Eng 33(2):202–208
Charache S (1994) Sickle cells and sudden death. J Lab Clin Med 124(4):473–474
Castro O, Hoque M, Brown BD (2003) Pulmonary hypertension in sickle cell disease: cardiac catheterization results and survival. Blood 101(4):1257–1261
Fonseca GH et al (2012) Pulmonary hypertension diagnosed by right heart catheterisation in sickle cell disease. Eur Respir J 39(1):112–118
Mushemi-Blake S, Melikian N, Drasar E, Bhan A, Lunt A, Desai SR, Greenough A, Monaghan MJ, Thein SL, Shah AM (2015) Pulmonary Haemodynamics in sickle cell disease are driven predominantly by a high-output state rather than elevated pulmonary vascular resistance: a prospective 3-dimensional echocardiography/Doppler study. PLoS One 10(8):e0135472
Mehari A, Gladwin MT, Tian X, Machado RF, Kato GJ (2012) Mortality in adults with sickle cell disease and pulmonary hypertension. Jama 307(12):1254–1256
Parent F, Bachir D, Inamo J, Lionnet F, Driss F, Loko G, Habibi A, Bennani S, Savale L, Adnot S, Maitre B, Yaïci A, Hajji L, O'Callaghan DS, Clerson P, Girot R, Galacteros F, Simonneau G (2011) A hemodynamic study of pulmonary hypertension in sickle cell disease. N Engl J Med 365(1):44–53
Leight L et al (1954) Hemodynamic studies in sickle cell anemia. Circulation 10(5):653–662
Fonseca G, Souza R (2015) Pulmonary hypertension in sickle cell disease. Curr Opin Pulm Med 21(5):432–437
Machado RF, Barst RJ, Yovetich NA, Hassell KL, Kato GJ, Gordeuk VR, Gibbs JSR, Little JA, Schraufnagel DE, Krishnamurti L, Girgis RE, Morris CR, Rosenzweig EB, Badesch DB, Lanzkron S, Onyekwere O, Castro OL, Sachdev V, Waclawiw MA, Woolson R, Goldsmith JC, Gladwin MT, on behalf of the walk-PHaSST Investigators and Patients (2011) Hospitalization for pain in patients with sickle cell disease treated with sildenafil for elevated TRV and low exercise capacity. Blood 118(4):855–864
Nauser TD, Stites SW (2001) Diagnosis and treatment of pulmonary hypertension. Am Fam Physician 63(9):1789–1798
Potoka KP, Gladwin MT (2015) Vasculopathy and pulmonary hypertension in sickle cell disease. Am J Physiol Lung Cell Mol Physiol 308(4):L314–L324
Noguchi CT, Schechter AN, Rodgers GP (1993) Sickle cell disease pathophysiology. Baillieres Clin Haematol 6(1):57–91
Guarda CCD, Santiago RP, Fiuza LM, Aleluia MM, Ferreira JRD, Figueiredo CVB, Yahouedehou SCMA, Oliveira RM, Lyra IM, Gonçalves MS (2017) Heme-mediated cell activation: the inflammatory puzzle of sickle cell anemia. Expert Rev Hematol 10(6):533–541
Aessopos A, Farmakis D, Tsironi M, Diamanti-Kandarakis E, Matzourani M, Fragodimiri C, Hatziliami A, Karagiorga M (2007) Endothelial function and arterial stiffness in sickle-thalassemia patients. Atherosclerosis 191(2):427–432
Ranque B, Menet A, Boutouyrie P, Diop IB, Kingue S, Diarra M, N’Guetta R, Diallo D, Diop S, Diagne I, Sanogo I, Tolo A, Chelo D, Wamba G, Gonzalez JP, Abough’elie C, Diakite CO, Traore Y, Legueun G, Deme-Ly I, Faye BF, Seck M, Kouakou B, Kamara I, le Jeune S, Jouven X (2016) Arterial stiffness impairment in sickle cell disease associated with chronic vascular complications: the multinational African CADRE study. Circulation 134(13):923–933
Champion HC, Michelakis ED, Hassoun PM (2009) Comprehensive invasive and noninvasive approach to the right ventricle-pulmonary circulation unit: state of the art and clinical and research implications. Circulation 120(11):992–1007
Lammers S, Scott D, Hunter K, Tan W, Shandas R, Stenmark KR (2012) Mechanics and function of the pulmonary vasculature: implications for pulmonary vascular disease and right ventricular function. Compr Physiol 2(1):295–319
Schreier DA, Forouzan O, Hacker TA, Sheehan J, Chesler N (2016) Increased red blood cell stiffness increases pulmonary vascular resistance and pulmonary arterial pressure. J Biomech Eng 138(2):021012. https://doi.org/10.1115/1.4032187
Schreier DA, Hacker TA, Hunter K, Eickoff J, Liu A, Song G, Chesler N (1985) Impact of increased hematocrit on right ventricular afterload in response to chronic hypoxia. J Appl Physiol 117(8):833–839. https://doi.org/10.1152/japplphysiol.00059.2014
Tabima DM, Roldan-Alzate A, Wang Z, Hacker TA, Molthen RC, Chesler NC (2012) Persistent vascular collagen accumulation alters hemodynamic recovery from chronic hypoxia. J Biomech 45(5):799–804
Wang Z, Chesler NC (2011) Pulmonary vascular wall stiffness: an important contributor to the increased right ventricular afterload with pulmonary hypertension. Pulm Circ 1(2):212–223
Morel FM, Baker RF, Wayland H (1971) Quantitation of human red blood cell fixation by glutaraldehyde. J Cell Biol 48(1):91–100
Schaer DJ, Buehler PW (2013) Cell-free hemoglobin and its scavenger proteins: new disease models leading the way to targeted therapies. Cold Spring Harb Perspect Med 3(6)
Alvarado AM, Ward KM, Muntz DS, Thompson AA, Rodeghier M, Fernhall B, Liem RI (2015) Heart rate recovery is impaired after maximal exercise testing in children with sickle cell anemia. J Pediatr 166(2):389–93 e1
Mitchell GF et al (1994) Measurement of aortic input impedance in rats. Am J Phys 267(5 Pt 2):H1907–H1915
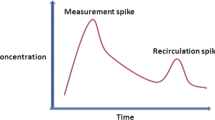
Westerhof N et al (1972) Forward and backward waves in the arterial system. Cardiovasc Res 6(6):648–656
Hollander EH, Wang JJ, Dobson GM, Parker KH, Tyberg JV (2001) Negative wave reflections in pulmonary arteries. Am J Physiol Heart Circ Physiol 281(2):H895–H902
Nie M, Kobayashi H, Sugawara M, Tomita T, Ohara K, Yoshimura H (2001) Helium inhalation enhances vasodilator effect of inhaled nitric oxide on pulmonary vessels in hypoxic dogs. Am J Physiol Heart Circ Physiol 280(4):H1875–H1881
Smolich JJ, Mynard JP, Penny DJ (2008) Simultaneous pulmonary trunk and pulmonary arterial wave intensity analysis in fetal lambs: evidence for cyclical, midsystolic pulmonary vasoconstriction. Am J Physiol Regul Integr Comp Physiol 294(5):R1554–R1562
Mitchell GF, Parise H, Benjamin EJ, Larson MG, Keyes MJ, Vita JA, Vasan RS, Levy D (2004) Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: the Framingham heart study. Hypertension 43(6):1239–1245
Brandao MM et al (2003) Optical tweezers for measuring red blood cell elasticity: application to the study of drug response in sickle cell disease. Eur J Haematol 70(4):207–211
Higgins JM, Eddington DT, Bhatia SN, Mahadevan L (2007) Sickle cell vasoocclusion and rescue in a microfluidic device. Proc Natl Acad Sci USA 104(51):20496–20500
Hiruma H et al (1995) Contributions of sickle hemoglobin polymer and sickle cell membranes to impaired filterability. Am J Phys 268(5 Pt 2):H2003–H2008
Noguchi CT, Torchia DA, Schechter AN (1980) Determination of deoxyhemoglobin S polymer in sickle erythrocytes upon deoxygenation. Proc Natl Acad Sci USA 77(9):5487–5491
Wood DK et al (2012) A biophysical indicator of vaso-occlusive risk in sickle cell disease. Sci Transl Med 4(123):123ra26
Ballas SK, Mohandas N (2004) Sickle red cell microrheology and sickle blood rheology. Microcirculation 11(2):209–225
Eaton WA, Hofrichter J (1990) Sickle cell hemoglobin polymerization. Adv Protein Chem 40:63–279
Acknowledgments
We thank Dr. Ron R. Magness for the use of the viscometer. We would also like to thank Gaoussou Diarra for his surgical expertise performing the in vivo hemodynamic measurements.
Funding
This study is supported by National Institutes of Health (NIH), NIH R21-HL086939 (NCC) and NIH F31 HL128088–01 (DAS).
Author information
Authors and Affiliations
Contributions
David Schreier1,2,3,4, Timothy Hacker1,2,4, Diana Tabima1,4, Manu O. Platt1,4, Naomi Chesler1,4
1. Designed research.
2. Performed research.
3. Analyzed data.
4. Wrote the paper.
Corresponding author
Ethics declarations
Conflict of Interest
No conflicts of interest, financial or otherwise, are declared by the author(s). The University of Wisconsin-Madison Institutional Animal Care and Use Committee approved all procedures.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 78 kb)
Rights and permissions
About this article
Cite this article
Schreier, D.A., Hacker, T.A., Tabima, D.M. et al. Effects of Red Blood Cell Sickling on Right Ventricular Afterload in vivo. Exp Mech 61, 229–235 (2021). https://doi.org/10.1007/s11340-020-00669-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11340-020-00669-3