Abstract
Background
Calcification was recently found to be present in the majority of cerebral aneurysms, though how calcification and the presence or absence of co-localized lipid pools affect failure properties is still unknown.
Objective
The primary objective is to quantify the biomechanical effect of a macro-calcification with surrounding Near-Calcification Region (NCR) of varying mechanical properties on tissue failure behavior.
Methods
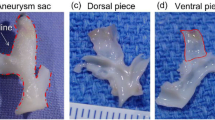
We utilized a structurally informed finite element model to simulate pre-failure and failure behavior of a human cerebral tissue specimen modeled as a composite containing a macro-calcification and surrounding NCR, embedded in a fiber matrix composite. Data from multiple imaging modalities was combined to quantify the collagen organization and calcification geometry. An idealized parametric model utilizing the calibrated model was used to explore the impact of NCR properties on tissue failure.
Results
Compared to tissue without calcification, peak stress was reduced by 82% and 49% for low modulus (representing lipid pool) and high modulus (simulating increase in calcification size) of the NCR, respectively. Failure process strongly depended on NCR properties with lipid pools blunting the onset of complete failure. When the NCR was calcified, the sample was able to sustain larger overall stress, however the failure process was abrupt with nearly simultaneous failure of the loaded fibers.
Conclusions
Failure of calcified vascular tissue is strongly influenced by the ultrastructure in the vicinity of the calcification. Computational modeling of failure in fibrous soft tissues can be used to understand how pathological changes impact the tissue failure process, with potentially important clinical implications.









Similar content being viewed by others
References
Vlak MHM, Algra A, Brandenburg R, Rinkel GJE (2011) Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: a systematic review and meta-analysis. Lancet Neurol 10(7):626–636. https://doi.org/10.1016/S1474-4422(11)70109-0
Kelly PJ, Stein J, Shafqat S, Eskey C, Doherty D, Chang Y, Kurina A, Furie KL (2001) Functional recovery after rehabilitation for cerebellar stroke. Stroke 32(2):530–534. https://doi.org/10.1161/01.str.32.2.530
Ropper AH, Zervas NT (1984) Outcome 1 year after SAH from cerebral aneurysm. 60 (5):909. https://doi.org/10.3171/jns.1984.60.5.0909
Broderick JP, Brown RD, Sauerbeck L, Hornung R, Huston J, Woo D, Anderson C, Rouleau G, Kleindorfer D, Flaherty ML, Meissner I, Foroud T, Charles E, Moomaw J, Connolly ES (2009) Greater Rupture Risk for Familial as Compared to Sporadic Unruptured Intracranial Aneurysms. Stroke 40(6):1952–1957. https://doi.org/10.1161/STROKEAHA.108.542571
Wiebers DO (1998) Unruptured intracranial aneurysms–risk of rupture and risks of surgical intervention. N Engl J Med 339(24):1725–1733. https://doi.org/10.1056/NEJM199812103392401
Juvela S, Poussa K, Lehto H, Porras M (2013) Natural history of unruptured intracranial aneurysms: a long-term follow-up study. Stroke 44(9):2414–2421. https://doi.org/10.1161/STROKEAHA.113.001838
Wiebers DO (2003) Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 362(9378):103–110. https://doi.org/10.1016/s0140-6736(03)13860-3
Berg P, Voss S, Janiga G, Saalfeld S, Bergersen AW, Valen-Sendstad K, Bruening J, Goubergrits L, Spuler A, Chiu TL, Tsang ACO, Copelli G, Csippa B, Paal G, Zavodszky G, Detmer FJ, Chung BJ, Cebral JR, Fujimura S, Takao H, Karmonik C, Elias S, Cancelliere NM, Najafi M, Steinman DA, Pereira VM, Piskin S, Finol EA, Pravdivtseva M, Velvaluri P, Rajabzadeh-Oghaz H, Paliwal N, Meng H, Seshadhri S, Venguru S, Shojima M, Sindeev S, Frolov S, Qian Y, Wu YA, Carlson KD, Kallmes DF, Dragomir-Daescu D, Beuing O (2019) Multiple Aneurysms AnaTomy CHallenge 2018 (MATCH)-phase II: rupture risk assessment. Int J Comput Assist Radiol Surg 14(10):1795–1804. https://doi.org/10.1007/s11548-019-01986-2
Frosen J, Cebral J, Robertson AM, Aoki T (2019) Flow-induced, inflammation-mediated arterial wall remodeling in the formation and progression of intracranial aneurysms. Neurosurg Focus 47(1):E21. https://doi.org/10.3171/2019.5.FOCUS19234
Cebral JR, Castro MA, Burgess JE, Pergolizzi RS, Sheridan MJ, Putman CM (2005) Characterization of cerebral aneurysms for assessing risk of rupture by using patient-specific computational hemodynamics models. Am J Neuroradiol 26(10):2550–2559
Gade PS, Tulamo R, Lee KW, Mut F, Ollikainen E, Chuang CY, Jae Chung B, Niemela M, Rezai Jahromi B, Aziz K, Yu A, Charbel FT, Amin-Hanjani S, Frosen J, Cebral JR, Robertson AM (2019) Calcification in Human Intracranial Aneurysms Is Highly Prevalent and Displays Both Atherosclerotic and Nonatherosclerotic Types. Arterioscler Thromb Vasc Biol 39(10):2157–2167. https://doi.org/10.1161/ATVBAHA.119.312922
Gade PS, Robertson AM, Chuang CY (2019) Multiphoton Imaging of Collagen, Elastin, and Calcification in Intact Soft-Tissue Samples. Curr Protoc Cytom 87(1):e51. https://doi.org/10.1002/cpcy.51
Barrett HE, Van der Heiden K, Farrell E, Gijsen FJH, Akyildiz AC (2019) Calcifications in atherosclerotic plaques and impact on plaque biomechanics. J Biomech 87:1–12. https://doi.org/10.1016/j.jbiomech.2019.03.005
Buijs R, Willems T, Tio R, Boersma H, Tielliu I, Slart R, Zeebregts C (2013) Calcification as a risk factor for rupture of abdominal aortic aneurysm. Eur J Vasc Endovasc Surg 46(5):542–548
Cardoso L, Kelly-Arnold A, Maldonado N, Laudier D, Weinbaum S (2014) Effect of tissue properties, shape and orientation of microcalcifications on vulnerable cap stability using different hyperelastic constitutive models. J Biomech 47(4):870–877. https://doi.org/10.1016/j.jbiomech.2014.01.010
Speelman L, Bohra A, Bosboom EMH, Schurink GWH, van de Vosse FN, Makaroun MS, Vorp DA (2006) Effects of wall calcifications in patient-specific wall stress analyses of abdominal aortic aneurysms. J Biomech Eng. 2007;129(1):105–109. https://doi.org/10.1115/1.2401189
Volokh KY, Aboudi J (2016) Aneurysm strength can decrease under calcification. J Mech Behav Biomed Mater 57:164–174. https://doi.org/10.1016/j.jmbbm.2015.11.012
Sang C, Maiti S, Fortunato RN, Kofler J, Robertson AM (2018) A uniaxial testing approach for consistent failure in vascular tissues. J Biomech Eng 140(6):6061010-6061011. https://doi.org/10.1115/1.4039577
Robertson AM, Duan X, Aziz KM, Hill MR, Watkins SC, Cebral JR (2015) Diversity in the Strength and Structure of Unruptured Cerebral Aneurysms. Ann Biomed Eng 43(7):1502–1515. https://doi.org/10.1007/s10439-015-1252-4
Hill MR, Duan X, Gibson GA, Watkins S, Robertson AM (2012) A theoretical and non-destructive experimental approach for direct inclusion of measured collagen orientation and recruitment into mechanical models of the artery wall. J Biomech 45(5):762–771. https://doi.org/10.1016/j.jbiomech.2011.11.016
Bredfeldt JS, Liu Y, Pehlke CA, Conklin MW, Szulczewski JM, Inman DR, Keely PJ, Nowak RD, Mackie TR, Eliceiri KW (2014) Computational segmentation of collagen fibers from second-harmonic generation images of breast cancer. J Biomed Opt 19(1):16007. https://doi.org/10.1117/1.JBO.19.1.016007
Schneider CA, Rasband WS, Eliceiri KW (2012) NIH Image to ImageJ: 25 years of image analysis. Nat Methods 9(7):671–675. https://doi.org/10.1038/nmeth.2089
Thunes JR, Pal S, Fortunato RN, Phillippi JA, Gleason TG, Vorp DA, Maiti S (2016) A structural finite element model for lamellar unit of aortic media indicates heterogeneous stress field after collagen recruitment. J Biomech 49(9):1562–1569. https://doi.org/10.1016/j.jbiomech.2016.03.034
Thunes JR, Phillippi JA, Gleason TG, Vorp DA, Maiti S (2018) Structural modeling reveals microstructure-strength relationship for human ascending thoracic aorta. J Biomech 71:84–93. https://doi.org/10.1016/j.jbiomech.2018.01.037
Bonet J, Wood RD (2008) Nonlinear continuum mechanics for finite element analysis. 2nd edn. Cambridge University Press, Cambridge. https://doi.org/10.1017/cbo9780511755446
Maiti S, Geubelle PH (2004) Mesoscale modeling of dynamic fracture of ceramic materials. CMES-Computer Modeling in Engineering & Sciences, 5(2), 91–102. https://doi.org/10.3970/cmes.2004.005.091
Fortunato RN, Robertson AM, Sang C, Maiti S (2019) Computational modeling reveals the relationship between intrinsic failure properties and uniaxial biomechanical behavior of arterial tissue. Biomech Model Mechanobiol 18(6):1791–1807. https://doi.org/10.1007/s10237-019-01177-7
Ebenstein DM, Coughlin D, Chapman J, Li C, Pruitt LA (2009) Nanomechanical properties of calcification, fibrous tissue, and hematoma from atherosclerotic plaques. J Biomed Mater Res A 91(4):1028–1037. https://doi.org/10.1002/jbm.a.32321
Cahalane RM, Barrett HE, O’Brien JM, Kavanagh EG, Moloney MA, Walsh MT (2018) Relating the mechanical properties of atherosclerotic calcification to radiographic density: A nanoindentation approach. Acta Biomater 80:228–236. https://doi.org/10.1016/j.actbio.2018.09.010
Holzapfel GA, Sommer G, Regitnig P (2004) Anisotropic mechanical properties of tissue components in human atherosclerotic plaques. J Biomech Eng 126(5):657–665. https://doi.org/10.1115/1.1800557
Ferrara A, Pandolfi A (2008) Numerical modelling of fracture in human arteries. Computer Methods in Biomechanics and Biomedical Engineering 11 (5):553-567. https://doi.org/10.1080/10255840701771743
Vengrenyuk Y, Carlier S, Xanthos S, Cardoso L, Ganatos P, Virmani R, Einav S, Gilchrist L, Weinbaum S (2006) A hypothesis for vulnerable plaque rupture due to stress-induced debonding around cellular microcalcifications in thin fibrous caps. Proc Natl Acad Sci 103 (40):14678–14683
Kelly-Arnold A, Maldonado N, Laudier D, Aikawa E, Cardoso L, Weinbaum S (2013) Revised microcalcification hypothesis for fibrous cap rupture in human coronary arteries. Proc Natl Acad Sci U S A 110(26):10741–10746. https://doi.org/10.1073/pnas.1308814110
Converse MI, Walther RG, Ingram JT, Li Y, Yu SM, Monson KL (2018) Detection and characterization of molecular-level collagen damage in overstretched cerebral arteries. Acta Biomater 67:307–318. https://doi.org/10.1016/j.actbio.2017.11.052
Enea D, Henson F, Kew S, Wardale J, Getgood A, Brooks R, Rushton N (2011) Extruded collagen fibres for tissue engineering applications: effect of crosslinking method on mechanical and biological properties. J Mater Sci Mater Med 22(6):1569–1578. https://doi.org/10.1007/s10856-011-4336-1
Gentleman E, Lay AN, Dickerson DA, Nauman EA, Livesay GA, Dee KC (2003) Mechanical characterization of collagen fibers and scaffolds for tissue engineering. Biomaterials 24(21):3805–3813. https://doi.org/10.1016/s0142-9612(03)00206-0
Miyazaki H, Hayashi K (1999) Tensile Tests of Collagen Fibers Obtained from the Rabbit Patellar Tendon. Biomed Microdevice 2(2):151–157. https://doi.org/10.1023/a:1009953805658
Sacks MS, Sun W (2003) Multiaxial mechanical behavior of biological materials. Annu Rev Biomed Eng 5:251–284. https://doi.org/10.1146/annurev.bioeng.5.011303.120714
Sacks MS, Zhang W, Wognum S (2016) A novel fibre-ensemble level constitutive model for exogenous cross-linked collagenous tissues. Interface Focus 6(1):20150090. https://doi.org/10.1098/rsfs.2015.0090
Schriefl AJ, Schmidt T, Balzani D, Sommer G, Holzapfel GA (2015) Selective enzymatic removal of elastin and collagen from human abdominal aortas: uniaxial mechanical response and constitutive modeling. Acta Biomater 17:125–136. https://doi.org/10.1016/j.actbio.2015.01.003
Weisbecker H, Viertler C, Pierce DM, Holzapfel GA (2013) The role of elastin and collagen in the softening behavior of the human thoracic aortic media. J Biomech 46(11):1859–1865. https://doi.org/10.1016/j.jbiomech.2013.04.025
Zhang W, Ayoub S, Liao J, Sacks MS (2016) A meso-scale layer-specific structural constitutive model of the mitral heart valve leaflets. Acta Biomater 32:238–255. https://doi.org/10.1016/j.actbio.2015.12.001
Acknowledgments
Research reported in this work was supported by the National Institutes of Health under award number 1R01-NS097457-01 and 5T32HL076124-12. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All protocols involving Human Participants have been approved by University of Pittsburgh IRB under STUDY20020015.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fortunato, R.N., Robertson, A.M., Sang, C. et al. Effect of Macro-calcification on the Failure Mechanics of Intracranial Aneurysmal Wall Tissue. Exp Mech 61, 5–18 (2021). https://doi.org/10.1007/s11340-020-00657-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11340-020-00657-7