Abstract
Introduction
Intermittent hypoxemia has an important role in the physiopathogenesis of obstructive sleep apnea (OSA) complications. Increased apoptosis due to intermittent hypoxemia may be an important clinical entity in OSA. In this study, we aimed to evaluate caspase-3 enzyme level, which is an indirect marker of increased apoptosis in patients with OSA and to evaluate the effect of OSA treatment with continuous positive airway pressure on caspase-3 enzyme level.
Materials and methods
This study included 141 consecutive patients admitted to the sleep-disordered breathing laboratory within 6 months. Caspase-3 was measured in routine blood samples obtained on the morning of polysomnography (PSG) performed at night. The compliance of the patients to CPAP treatment was evaluated and caspase-3 levels were checked again after treatment.
Results
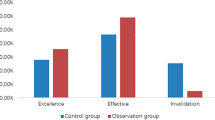
A total of 141 patients, 39 females (27,7%) and 102 males (72,3%) were included in the study. The mean age of the patients was 49 ± 12 years (min-17, max-77). According to PSG results, OSA was detected in 95.7% (135/141) of the cases. Mild OSA was 35 (24.8%), moderate OSA 39 (27.7%) and severe OSA 61 (43.3%) cases. Median caspase-3 enzyme levels were similar in men and women in the study group. There was no statistically significant difference in hemogram parameters and caspase-3 enzyme levels between the groups divided according to the presence and severity of OSA. It was determined that caspase-3 enzyme level did not change significantly after 3 months of CPAP treatment in OSA compared to pretreatment. Caspase-3 was found to have a negative correlation with both the percentage of daily use of CPAP therapy and the percentage of CPAP device use for more than 1 h per night. It was found that the control caspase-3 level decreased statistically significantly as the percentage of daily use of CPAP therapy increased (r = -0.397, p = 0.030). It was found that the control caspase-3 level decreased statistically significantly as the percentage of CPAP therapy use for more than 1 h per night increased (r = -0.411, p = 0.024).
Conclusion
The results of this study did not reveal a relationship between the severity of OSA and caspase-3 levels. However, blood caspase-3 levels decreased as treatment compliance increased, suggesting that CPAP treatment may correct increased apoptosis in OSA. There is a need for more comprehensive studies on this issue.




Similar content being viewed by others
Data Availability
Our manuscript hasno associated data.
References
Young T, Palta M, Dempsey J et al (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235. https://doi.org/10.1056/NEJM199304293281704
Köktürk O (1998) OSAS epidemiyolojisi, Tüberküloz ve Toraks Dergisi 46(2):193–01
Benjafield AV, Ayas NT, Eastwood PR et al (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7:687–698. https://doi.org/10.1016/S2213-2600(19)30198-5
Kezban OS, Ali NA, Umran T et al (2012) Is obstructive sleep apnea syndrome a risk factor for pulmonary thromboembolism? Chin Med J (Engl) 125:3712–3718
Balbay EG, Balbay O, Annakkaya AN et al (2014) Obstructive sleep apnoea syndrome in patients with primary open-angle glaucoma. Hong Kong Med J. https://doi.org/10.12809/hkmj134021
Thompson CB (1999) Apoptosis. In Paul WE (ed) Fundamental Immunology, 4th edn. Lippincott-Raven, New York, pp 813–829
Neubauer JA (2001) Invited Review: Physiological and pathophysiological responses to intermittent hypoxia. J Appl Physiol 90:1593–1599. https://doi.org/10.1152/jappl.2001.90.4.1593
Fei W, Jiao W, Feng X et al (2021) Intermittent hypoxia mimicking obstructive sleep apnea aggravates early brain injury following ICH via neuroinflammation and apoptosis. Mol Med Rep 24:824. https://doi.org/10.3892/mmr.2021.12464
Chen MY-C (2015) Role of Sodium-Hydrogen Exchanger-1 (NHE-1) in the Effect of Exercise on Intermittent Hypoxia-Induced Left Ventricular Dysfunction. Chin J Physiol 58:254–262. https://doi.org/10.4077/CJP.2015.BAE357
Yu AY, Frid MG, Shimoda LA et al (1998) Temporal, spatial, and oxygen-regulated expression of hypoxia-inducible factor-1 in the lung. Am J Physiol Lung Cell Mol Physiol 275:L818–L826. https://doi.org/10.1152/ajplung.1998.275.4.L818
Liu Y, Song X, Wang X et al (2010) Effect of chronic intermittent hypoxia on biological behavior and hypoxia-associated gene expression in lung cancer cells. J Cell Biochem 111:554–563. https://doi.org/10.1002/jcb.22739
Nicholson DW (1999) Caspase structure, proteolytic substrates, and function during apoptotic cell death. Cell Death Differ 6:1028–1042. https://doi.org/10.1038/SJ.CDD.4400598
Larsen BD, Sørensen CS (2017) The caspase-activated DNase: apoptosis and beyond. FEBS J 284:1160–1170. https://doi.org/10.1111/FEBS.13970
Selznick LA, Holtzman DM, Han BH et al (1999) In Situ Immunodetection of Neuronal Caspase-3 Activation in Alzheimer Disease. J Neuropathol Exp Neurol 58:1020–1026. https://doi.org/10.1097/00005072-199909000-00012
Su JH, Zhao M, Anderson AJ et al (2001) Activated caspase-3 expression in Alzheimer’s and aged control brain: correlation with Alzheimer pathology. Brain Res 898:350–357. https://doi.org/10.1016/S0006-8993(01)02018-2
Hori T, Sugita Y, Koga E et al (2001) Proposed supplements and amendments to ‘ A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Subjects ’, the Rechtschaffen & Kales (1968) standard. Psychiatry Clin Neurosci 55:305–310. https://doi.org/10.1046/j.1440-1819.2001.00810.x
Malhotra RK, Kirsch DB, Kristo DA et al (2018) Polysomnography for Obstructive Sleep Apnea Should Include Arousal-Based Scoring: An American Academy of Sleep Medicine Position Statement. J Clin Sleep Med 14:1245–1247. https://doi.org/10.5664/jcsm.7234
Sateia MJ (2014) International classification of sleep disorders-third edition: highlights and modifications. Chest 146:1387–1394. https://doi.org/10.1378/CHEST.14-0970
Shin C, Kim JK, Kim JH et al (2008) Increased cell-free DNA concentrations in patients with obstructive sleep apnea. Psychiatry Clin Neurosci 62:721–727. https://doi.org/10.1111/j.1440-1819.2008.01876.x
El Solh AA, Akinnusi ME, Baddoura FH, Mankowski CR (2007) Endothelial Cell Apoptosis in Obstructive Sleep Apnea. Am J Respir Crit Care Med 175:1186–1191. https://doi.org/10.1164/rccm.200611-1598OC
Li RC, Row BW, Gozal E et al (2003) Cyclooxygenase 2 and Intermittent Hypoxia-induced Spatial Deficits in the Rat. Am J Respir Crit Care Med 168:469–475. https://doi.org/10.1164/rccm.200211-1264OC
Elmore S (2007) Apoptosis: A Review of Programmed Cell Death. Toxicol Pathol 35:495–516. https://doi.org/10.1080/01926230701320337
Lin X, Wang H, Wu D et al (2017) High Leptin Level Attenuates Embryo Development in Overweight/Obese Infertile Women by Inhibiting Proliferation and Promotes Apoptosis in Granule Cell. Horm Metab Res 49:534–541. https://doi.org/10.1055/s-0043-107617
Han J, Zhao C, Guo H et al (2023) Obesity induces male mice infertility via oxidative stress, apoptosis, and glycolysis. Reproduction 166:27–36. https://doi.org/10.1530/REP-23-0097
Butler AE, Janson J, Bonner-Weir S et al (2003) β-Cell Deficit and Increased β-Cell Apoptosis in Humans With Type 2 Diabetes. Diabetes 52:102–110. https://doi.org/10.2337/diabetes.52.1.102
Wang Q, Cui Y, Lin N, Pang S (2019) Correlation of cardiomyocyte apoptosis with duration of hypertension, severity of hypertension and caspase-3 expression in hypertensive rats. Exp Ther Med. https://doi.org/10.3892/etm.2019.7249
Schwarz K, Simonis G, Yu X et al (2006) Apoptosis at a distance: Remote activation of caspase-3 occurs early after myocardial infarction. Mol Cell Biochem 281:45–54. https://doi.org/10.1007/s11010-006-0233-1
Yang B, Ye D, Wang Y (2013) Caspase-3 as a therapeutic target for heart failure. Expert Opin Ther Targets 17:255–263. https://doi.org/10.1517/14728222.2013.745513
González A, López B, Ravassa S et al (2002) Stimulation of Cardiac Apoptosis in Essential Hypertension. Hypertension 39:75–80. https://doi.org/10.1161/hy0102.100788
Wang J, Sun H, Liu Y (2020) The proliferative and anti-apoptosis functions of KGF/KGFR contributes to bronchial epithelial repair in asthma. Pulm Pharmacol Ther 63:101931. https://doi.org/10.1016/j.pupt.2020.101931
Chiappara G, Gjomarkaj M, Sciarrino S et al (2014) Altered expression of p21, activated caspase-3, and PCNA in bronchiolar epithelium of smokers with and without chronic obstructive pulmonary disease. Exp Lung Res 40:343–353. https://doi.org/10.3109/01902148.2014.928836
Dirican E, Özcan H, Karabulut Uzunçakmak S, Takım U (2023) Evaluation Expression of the Caspase-3 and Caspase-9 Apoptotic Genes in Schizophrenia Patients. Clin Psychopharmacol Neurosci 21:171–178. https://doi.org/10.9758/cpn.2023.21.1.171
Mogi M, Togari A, Kondo T et al (2000) Caspase activities and tumor necrosis factor receptor R1 (p55) level are elevated in the substantia nigra from Parkinsonian brain. J Neural Transm 107:335–341. https://doi.org/10.1007/s007020050028
Young Yoo J, Kim CH, Song SH et al (2004) Expression of Caspase-3 and c-myc in Non-Small Cell Lung Cancer. Cancer Res Treat 36:303. https://doi.org/10.4143/crt.2004.36.5.303
Pu X, Storr SJ, Zhang Y et al (2017) Caspase-3 and caspase-8 expression in breast cancer: caspase-3 is associated with survival. Apoptosis 22:357–368. https://doi.org/10.1007/s10495-016-1323-5
Balasubramanian M, Kuberan A, Rawat A et al (2021) Effect of General Anesthetics on Caspase-3 Levels in Patients With Aneurysmal Subarachnoid Hemorrhage: A Preliminary Study. J Neurosurg Anesthesiol 33:172–176. https://doi.org/10.1097/ANA.0000000000000648
Funding
This study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declared no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by Duzce University Medical Faculty Non-Invasive Clinical Trials Ethics Committee (Decision Number: 2022/161).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The research is a medical specialization thesis (thesis number: 2023/10603375).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kaypak, M.K., Annakkaya, A.N., Davran, F. et al. The Effect of Continuous Positive Airway Pressure (CPAP) Therapy on Serum Caspase-3 Level in Patients with Obstructive Sleep Apnea (OSA). Sleep Breath (2024). https://doi.org/10.1007/s11325-024-03039-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11325-024-03039-8