Abstract
Objective
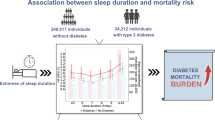
To explore the correlation between sleep duration and type II diabetes in adults.
Method
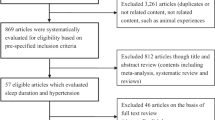
Computer databases searches were carried out through October 1, 2022, including PubMed, Cochrane Library, Embase, and Web of Science. Relevant literature was collected, and the Newcastle–Ottawa Scale (NOS) and extracted data were used to exclude studies and evaluate quality on the basis of inclusion and exclusion criteria. Meta-analysis was conducted using RevMan 5.4.1 software with random/fixed effects models.
Results
A total of 5 studies with 74,226 subjects (31,611 in the male study group, 42,615 in the female study group) were included. The meta-analysis revealed that women with long sleep duration (LSD) have a higher risk for developing type II diabetes than men, OR = 0.70; 95% CI 0.59–0.84, Z = 4.00 and P < 0.001. Men with short sleep duration (SSD) tended to have a higher risk in developing type II diabetes than women though the difference between men and women did not reach statistical significance, OR = 1.09, 95% CI 0.73–1.62, Z = 0.42 and P = 0.68. Further subgroup analysis by regional populations suggested that men in Europe and America with SSD had a higher risk of type II diabetes OR = 1.52, 95% CI 1.04–2.21, Z = 2.18 and P = 0.03.
Conclusion
Women with LSD may have a higher risk for type II diabetes, and men in Europe and America with SSD may have a higher risk for type II diabetes than men of other regions.






Similar content being viewed by others
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
References
Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ et al (2011) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 378:31–40
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N et al (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pr 157:107843
Xu Y, Wang L, He J, Bi Y, Li M, Wang T et al (2013) Prevalence and control of diabetes in Chinese adults. Jama-J Am Med Assoc 310:948–959
Dag IDF (2015) Update of mortality attributable to diabetes for the IDF Diabetes Atlas: Estimates for the year 2013. Diabetes Res Clin Pr 109:461–465
Larcher S, Benhamou PY, Pepin JL, Borel AL (2015) Sleep habits and diabetes. Diabetes Metab 41:263–271
Shan Z, Ma H, Xie M, Yan P, Guo Y, Bao W et al (2015) Sleep duration and risk of type II diabetes: a meta-analysis of prospective studies. Diabetes Care 38:529–537
Ayas NT, White DP, Al-Delaimy WK, Manson JE, Stampfer MJ, Speizer FE et al (2003) A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care 26:380–384
Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE et al (2004) A prospective study of sleep duration and mortality risk in women. Sleep 27:440–444
Mallon L, Broman JE, Hetta J (2005) High incidence of diabetes in men with sleep complaints or short sleep duration: a 12-year follow-up study of a middle-aged population. Diabetes Care 28:2762–2767
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama-J Am Med Assoc 283:2008–12
Zhang X, Tan R, Lam WC, Yao L, Wang X, Cheng CW et al (2020) PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Extension for Chinese Herbal Medicines 2020 (PRISMA-CHM 2020). Am J Chinese Med 48:1279–1313
Stang A, Jonas S, Poole C (2018) Case study in major quotation errors: a critical commentary on the Newcastle-Ottawa scale. Eur J Epidemiol 33:1025–1031
Zhang P, Wu Y, Jiang Z, Jiang L, Fang B (2012) Osteogenic response of mesenchymal stem cells to continuous mechanical strain is dependent on ERK1/2-Runx2 signaling. Int J Mol Med 29:1083–1089
Chaput JP, Despres JP, Bouchard C, Tremblay A (2007) Association of sleep duration with type II diabetes and impaired glucose tolerance. Diabetologia 50:2298–2304
Wu HB, Wang H, Hu RY, Zhong JM, Qian YJ, Wang CM et al (2017) The association between sleep duration, snoring and prevalent type II diabetes mellitus with regard to gender and menopausal status: the CKB study in Zhejiang rural area. China Acta Diabetol 54:81–90
Lou P, Zhang P, Zhang L, Chen P, Chang G, Zhang N et al (2015) Effects of sleep duration and sleep quality on prevalence of type II diabetes mellitus: a 5-year follow-up study in China. Diabetes Res Clin Pr 109:178–184
Tuomilehto H, Peltonen M, Partinen M, Seppa J, Saaristo T, Korpi-Hyovalti E et al (2008) Sleep duration is associated with an increased risk for the prevalence of type 2 diabetes in middle-aged women - The FIN-D2D survey. Sleep Med 9:221–227
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L et al (2015) National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health 1:40–43
Desquilbet L, Mariotti F (2010) Dose-response analyses using restricted cubic spline functions in public health research. Stat Med 29:1037–1057
Sands-Lincoln M, Loucks EB, Lu B, Carskadon MA, Sharkey K, Stefanick ML et al (2013) Sleep duration, insomnia, and coronary heart disease among postmenopausal women in the Women’s Health Initiative. J Womens Health 22:477–486
Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR (2002) Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry 59:131–136
Cai H, Shu XO, Xiang YB, Yang G, Li H, Ji BT et al (2015) Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women. Sleep 38:529–536
Tan X, Chapman CD, Cedernaes J, Benedict C (2018) Association between long sleep duration and increased risk of obesity and type 2 diabetes: a review of possible mechanisms. Sleep Med Rev 40:127–134
Zizi F, Jean-Louis G, Brown CD, Ogedegbe G, Boutin-Foster C, McFarlane SI (2010) Sleep duration and the risk of diabetes mellitus: epidemiologic evidence and pathophysiologic insights. Curr Diabetes Rep 10:43–47
Martin-Millan M, Castaneda S (2013) Estrogens, osteoarthritis and inflammation. Joint Bone Spine 80:368–373
Habib P, Dreymueller D, Rosing B, Botung H, Slowik A, Zendedel A et al (2018) Estrogen serum concentration affects blood immune cell composition and polarization in human females under controlled ovarian stimulation. J Steroid Biochem 178:340–347
Eldridge RC, Wentzensen N, Pfeiffer RM, Brinton LA, Hartge P, Guillemette C et al (2020) Endogenous estradiol and inflammation biomarkers: potential interacting mechanisms of obesity-related disease. Cancer Cause Control 31:309–320
Quintero OL, Amador-Patarroyo MJ, Montoya-Ortiz G, Rojas-Villarraga A, Anaya JM (2012) Autoimmune disease and gender: plausible mechanisms for the female predominance of autoimmunity. J Autoimmun 38:J109–J119
Hoeksema SN (1995) Gender differences in coping with depression across the lifespan. Depression 3
Bigos KL, Pollock BG, Stankevich BA, Bies RR (2009) Sex differences in the pharmacokinetics and pharmacodynamics of antidepressants: an updated review. Gend Med 6:522–543
Dhabhar FS, Burke HM, Epel ES, Mellon SH, Rosser R, Reus VI et al (2009) Low serum IL-10 concentrations and loss of regulatory association between IL-6 and IL-10 in adults with major depression. J Psychiatr Res 43:962–969
Dale E, Bang-Andersen B, Sanchez C (2015) Emerging mechanisms and treatments for depression beyond SSRIs and SNRIs. Biochem Pharmacol 95:81–97
Knutson KL (2005) Sex differences in the association between sleep and body mass index in adolescents. J Pediatr-Us 147:830–834
Irwin MR, Carrillo C, Olmstead R (2010) Sleep loss activates cellular markers of inflammation: sex differences. Brain Behav Immun 24:54–57
Tasali E, Leproult R, Ehrmann DA, Van Cauter E (2008) Slow-wave sleep and the risk of Type II diabetes in humans. P Natl Acad Sci USA 105:1044–1049
Bixler EO, Papaliaga MN, Vgontzas AN, Lin HM, Pejovic S, Karataraki M et al (2009) Women sleep objectively better than men and the sleep of young women is more resilient to external stressors: effects of age and menopause. J Sleep Res 18:221–228
Scheer FA, Hilton MF, Mantzoros CS, Shea SA (2009) Adverse metabolic and cardiovascular consequences of circadian misalignment. P Natl Acad Sci USA 106:4453–4458
Cain SW, Dennison CF, Zeitzer JM, Guzik AM, Khalsa SB, Santhi N et al (2010) Sex differences in phase angle of entrainment and melatonin amplitude in humans. J Biol Rhythm 25:288–296
Spiegel K, Leproult R, Van Cauter E (1999) Impact of sleep debt on metabolic and endocrine function. Lancet 354:1435–1439
Acknowledgements
We would also like to thank everyone who has helped with our research.
Funding
This study was funded by the Natural Science Foundation of Guangdong Province (2019A1515010981).
Author information
Authors and Affiliations
Contributions
RC, CW, YL, ZZZ, XC, and JZ are the guarantor of the manuscript and take responsibility for the content of this manuscript. RC, ZZ, and CW contributed to the design of the study. HC and JL were involved in the data analysis. HL and ZW contributed to the acquisition of primary data. ZZZ, CW, and XC wrote the initial draft of the manuscript. RC and YL contributed significantly to the revision of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
For this type of study formal consent is not required.
Informed consent
This article does not contain any studies with human participants performed by any of the authors.
Conflict of interest
All authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, C., Liu, Y., Chen, X. et al. Meta-analysis of correlation between sleep duration and gender difference in adults with type 2 diabetes. Sleep Breath 27, 2325–2332 (2023). https://doi.org/10.1007/s11325-023-02841-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02841-0