Abstract
Purpose
This study examined insomnia severity as a moderator of the associations between obstructive sleep apnea (OSA) severity with impaired mood and diabetes-related distress in adults with OSA and type 2 diabetes (T2D).
Methods
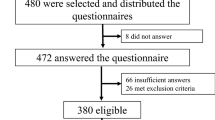
This secondary analysis used pooled baseline data from two randomized controlled trials that evaluated the efficacy of treatment of OSA or insomnia in adults with T2D. Participants for this analysis had OSA (Apnea Hypopnea Index [AHI] ≥ five events/hour obtained from an in-home sleep apnea testing device) and completed questionnaires on insomnia, mood, and diabetes-related distress. Hierarchical multiple linear regression and multivariate linear regression analyses were used controlling for demographic characteristics and restless leg syndrome.
Results
Of 240 participants, mean age was 57.8 ± 10.17, 50% were female, and 35% were non-White. Participants had poorly controlled diabetes (Mean HbA1C = 7.93 ± 1.62), and moderate OSA (Mean AHI = 19.3 ± 16.2). Insomnia severity significantly moderated the association between OSA severity and mood (b = -0.048, p = .017). Although insomnia severity did not moderate the relationship between OSA severity and diabetes-related distress (b = -0.009, p = .458), insomnia severity was independently associated with greater diabetes-related distress (b = 1.133, p < .001).
Conclusions
In adults with T2D and OSA, as insomnia severity increased, increasing OSA severity was associated with lower level of mood disturbances. Insomnia independently increased the level of diabetes-related distress. These findings suggest that comorbid insomnia may be more impactful than OSA on increasing mood disturbances and diabetes-related distress in adults with T2D.



Similar content being viewed by others
Data availability
Data will be made available on reasonable request.
References
Centers for Disease Control and Prevention. (2020) National diabetes statistics report, 2020. U. S. Department of Health and Human Services. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
Anderson RJ, Freedland KE, Clouse RE, Lustman PJ (2011) The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 24(6):1069–1078. https://doi.org/10.2337/diacare.24.6.1069
Li C, Barker L, Ford ES, Zhang X, Strine TW, Mokdad AH (2008) Diabetes and anxiety in US adults: findings from the 2006 Behavioral Risk Factor Surveillance System. Diabetes Med 25(7):878–881. https://doi.org/10.1111/j.1464-5491.2008.02477.x
Fisher L, Hessler DM, Polonsky WH, Mullan J (2012) When is diabetes distress clinically meaningful? Establishing cut points for the Diabetes Distress Scale. Diabetes Care 35(2):259–264. https://doi.org/10.2337/dc11-1572
Anderson RJ, Grigsby AB, Freedland KE, De Groot M, McGill JB, Clouse RE, Lustman PJ (2002) Anxiety and poor glycemic control: a meta-analytic review of the literature. Int J Psychiatry Med 32(3):235–247. https://doi.org/10.2190/KLGD-4H8D-4RYL-TWQ8
Gonzalez JS, Delahanty LM, Safren SA, Meigs JB, Gran RW (2008) Differentiating symptoms of depression from diabetes-specific distress: relationships with self-care in type 2 diabetes. Diabetol 51(10):1822–1825. https://doi.org/10.1007/s00125-008-1113-x
De Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ (2001) Association of depression and diabetes complications: a meta-analysis. Psychosom Med 63(4):619–630. https://doi.org/10.1097/00006842-200107000-00015
Pintaudi B, Lucisano G, Gentile S, Bulotta A, Skovlund SE, Vespasiani G, Rossi MC, Nicolucci A (2015) Correlates of diabetes-related distress in type 2 diabetes: findings from the benchmarking network for clinical and humanistic outcomes in diabetes (BENCH-D) study. J Psychosom Res 79(5):348–354. https://doi.org/10.1016/j.jpsychores.2015.08.010
Schipper SBJ, Van Veen MM, Elders PJM, Van Straten A, Van Der Werf YD, Knutson KL, Rutters F (2021) Sleep disorders in people with type 2 diabetes and associated health outcomes: a review of the literature. Diabetol 64:2367–2377. https://doi.org/10.1007/s00125-021-05541-0
Chen YH, Keller JK, Kang JH, Hsieh HJ, Lin HC (2013) Obstructive sleep apnea and the subsequent risk of depressive disorder: a population-based follow-up study. J Clin Sleep Med 9(5):417–423. https://doi.org/10.5664/jcsm.2652
Li L, Wu C, Gan Y, Qu X, Lu Z (2016) Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry 16(1):1–16. https://doi.org/10.1186/s12888-016-1075-3
Jeon B, Luyster FS, Callan JA, Chasens ER (2021) Depressive symptoms in comorbid obstructive sleep apnea and insomnia: an integrative review. West J Nurs Res 43(11):1061–1072. https://doi.org/10.1177/0193945921989656
Jeon B, Luyster FS, Sereika SM, DiNardo MM, Callan JA, Chasens ER (2022) Comorbid obstructive sleep apnea and insomnia and its associations with mood and diabetes-related distress in type 2 diabetes mellitus. J Clin Sleep Med 18(4):1103–1111. https://doi.org/10.5664/jcsm.9812
Jeon B (2022) The roles of obstructive sleep apnea and insomnia on mood, diabetes-related distress, and glycemic control in adults with type 2 diabetes mellitus. PhD dissertation, University of Pittsburgh
Collop NA, Anderson WM, Boehlecke B, Claman D, Goldberg R, Gottieb DJ, Hudgel D, Sateia M, Schwab R, Portable Monitoring Task Force of the American Academy of Sleep Medicine (2007) Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. J Clin Sleep Med 3(7):737–747
Berry RB, Brooks R, Gamaldo CE, Harding SM, Marcus C, Vaughn BV (2012) The AASM manual for the scoring of sleep and associated events. Rules, terminology and technical specifications, version 2.0. Darien, Illinois, American Academy of Sleep Medicine
Morin CM, Belleville G, Bélanger L, Ivers H (2011) The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 34(5):601–608. https://doi.org/10.1093/sleep/34.5.601
McNair DM, Heuchert P (2007) Profile of Mood States: POMS: technical update. Multi-Health Systems
Haensel A, Norman D, Natarajan L, Bardwell WA, Ancoli-Israel S, Dimsdale JE (2007) Effect of a 2 week CPAP treatment on mood states in patients with obstructive sleep apnea: a double-blind trial. Sleep Breath 11(4):239–244. https://doi.org/10.1107/s11325-007-0115-0
Jungquist CR, Tra Y, Smith MT, Pigeon WR, Matteson-Rusby S, Xia Y, Perlis ML (2012) The durability of cognitive behavioral therapy for insomnia in patients with chronic pain. Sleep Disord 2012:679648. https://doi.org/10.1155/2012/679648
Chasens ER, Morris J, Strollo PJ, Sereika SM, Burke LE, Korytkowski M (2016) Gender differences in the response to impaired sleep in adults with diabetes. Behav Sleep Med 14(4):457–466. https://doi.org/10.1080/15402002.2015.1017100
Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, Schwartz CE (1995) Assessment of diabetes-related distress. Diabetes Care 18(6):754–760. https://doi.org/10.2337/diacare.18.6.754
Johns MW (1991) A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 14(6):540–545. https://doi.org/10.1093/sleep/14.6.540
Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4
American Diabetes Association (2020) Standards of medical care in diabetes – 2020 abridged for primary care providers. Clin Diabetes 38(1):10–38. https://doi.org/10.2337/cd21-as01
Pillar G, Lavie P (1998) Psychiatric symptoms in sleep apnea syndrome: effects of gender and respiratory disturbance index. Chest 114(3):697–703. https://doi.org/10.1378/chest.114.3.697
Sforza E, Hilaire ZDS, Pelissolo A, Rochat T, Ibanez V (2002) Personality, anxiety and mood traits in patients with sleep-related breathing disorders: effect of reduced daytime alertness. Sleep Med 3(2):139–145. https://doi.org/10.1016/s1389-9457(01)00128-9
Ohayon MM (2003) The effects of breathing-related sleep disorders on mood disturbances in the general population. J Clin Psychiatry 64(10):1195–1200. https://doi.org/10.4088/jcp.v64n1009
Peppard PE, Szklo-Coxe M, Mae Hla K, Young T (2006) Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med 166(16):1709–1715. https://doi.org/10.1001/archinte.166.16.1709
Ye L, Pien GW, Ratcliffe SJ, Bjornsdottir E, Arnardottir ES, Pack AI, Benediktsdottir B, Gislason T (2014) The different clinical faces of obstructive 194 sleep apnoea: a cluster analysis. Eur Respir J 44(6):1600–1607. https://doi.org/10.1183/09031936.00032314
Saaresranta T, Hedner J, Bonsignore MR, Riha RL, McNicholas WT, Penzel T, Anttalainen U, Kvamme JA, Pretl M, Sliwinski P, Verbraecken J, Grote L, ESADA Study Group (2016) Clinical phenotypes and comorbidity in European sleep apnoea patients. PLoS One 11(10):e0163439. https://doi.org/10.1371/journal.pone.0163439
Young-Hyman D, De Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M (2016) Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Diabetes Care 39(12):2126–2140. https://doi.org/10.2337/dc16-2053
Quinn CC, Shardell MD, Terrin ML, Barr EA, Ballew SH, Gruber-Baldini AL (2011) Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care 34(9):1934–1942. https://doi.org/10.2337/dc11-0366
Simmons D, Prevost AT, Bunn C, Holman D, Parker RA, Cohn S, Donald S, Paddison CAM, Ward C, Robins P, Graffy J (2015) Impact of community based peer support in type 2 diabetes: a cluster randomised controlled trial of individual 191 and/or group approaches. PLoS One 10(3):e0120277. https://doi.org/10.1371/journal.pone.0120277
Van Dijk-de Vries A, Van Bokhoven MA, Winkens B, Terluin B, Knottnerus JA, Van Der Weijden T, Van Eijk JTM (2015) Lessons learnt from a cluster-randomised trial evaluating the effectiveness of Self-Management Support (SMS) delivered by practice nurses in routine diabetes care. BMJ Open 5(6):e007014. https://doi.org/10.1136/bmjopen-2014-007014
Chew BH, Vos RC, Metzendorf MI, Scholten RJ, Rutten GEHM (2017) Psychological interventions for diabetes-related distress in adults with type 2 diabetes mellitus. Cochrane Database Sys Rev 9(9):CD011469. https://doi.org/10.1002/14651858.CD011469.pub2
Smyth A, Jenkins M, Dunham M, Kutzer Y, Taheri S, Whitehead L (2020) Systematic review of clinical practice guidelines to identify recommendations for sleep in type 2 diabetes mellitus management. Diabetes Res Clin Pract 170:108532. https://doi.org/10.1016/j.diabres.2020.108532
Epstein LJ, Kristo D, Strollo PJ, Friedman N, Malhotra A, Patil SP, Ramar K, Rogers R, Schwab RJ, Weaver EM, Weinstein MD (2009) Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 5(3):263–276
Buysse DJ (2013) Insomnia. JAMA 309(7):706–716. https://doi.org/10.1001/jama.2013.193
Acknowledgements
This study is part of a doctoral dissertation from the University of Pittsburgh. The doctoral dissertation was published on http://d-scholarship.pitt.edu/42773/1/bomin_jeon_phd_etdfinal.pdf.
Funding
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (Chasens; R01-DK096028) and the National Institute of Nursing Research (Chasens; K24-NR016685). This research was also supported through Clinical Translational Science Institute at the University of Pittsburgh Grant Numbers UL1- RR024153 and UL1-TR000005.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data analysis and investigation were performed by Bomin Jeon and Susan M. Sereika. The first draft of the manuscript was written by Bomin Jeon, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by exemption from the University of Pittsburgh Institutional Review Board (IRB) because it was categorized as secondary research on an existing dataset (STUDY19100353).
Consent to participate
This study was a secondary analysis using existing dataset and formal consent was not required.
Consent to publication
Not applicable.
Competing interests
The author(s) have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jeon, B., Chasens, E.R., Luyster, F.S. et al. Is insomnia severity a moderator of the associations between obstructive sleep apnea severity with mood and diabetes-related distress?. Sleep Breath 27, 1081–1089 (2023). https://doi.org/10.1007/s11325-023-02819-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02819-y