Abstract
Purpose
To analyze relative efficacies of mandibular advancement devices (MAD) in sleep apnea treatment.
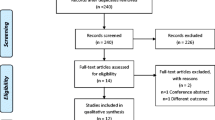
Methods
From eligible randomized controlled trials (RCT), MADs were classified based on their mechanistic designs. Data on apnea–hypopnea index (AHI), Epworth sleepiness scale (ESS), nadir oxygen saturation (minSaO2), and sleep efficiency (SE%) from RCTs were then analyzed in network meta-analyses, and relative ranking of different MADs was computed based on P scores (a method of ranking similar to SUCRA). Similar analyses were conducted based on the different brands of MADs.
Results
There were no statistically significant differences between MADs in any of the outcomes analyzed. However, the P-scores, based on the point estimates and standard errors of the network estimates, ranked some MADs higher than others in some of the outcomes. Of the different mechanistic designs, the highest P scores were achieved for attached midline traction (P score = 0.84) and unattached bilateral interlocking (P score = 0.78) devices for AHI reduction, attached bilateral traction (P score = 0.78) and unattached bilateral interlocking (P score = 0.76) for ESS, monobloc (P score = 0.91) and unattached bilateral interlocking (P score = 0.64) for minSaO2, and unattached bilateral interlocking (P score = 0.82) and attached bilateral traction (P score = 0.77) for SE%. Notable findings in the network meta-analyses based on MAD brands, of the limited number of studies that specified them were the effects of SomnoDent Flex™, TAP™, and IST® in their effects on AHI reduction, with P scores of 0.94, 0.83, and 0.82, respectively. Monobloc decreased supine-AHI the most (− 44.46 [− 62.55; − 26.36], P score = 0.99), and unattached bilateral interlocking had the greatest effect on REM-AHI (− 11.10 [− 17.10; − 5.10], P score = 0.87).
Conclusions
Findings from this study show clinically (but not statistically) significant differences between MADs in terms of their relative efficacy when analyzed for different sleep apnea treatment outcomes and sleep apnea phenotypes.








Similar content being viewed by others
Data availability
On reasonable request, data can be made available.
References
Sharples LD, Clutterbuck-James AL, Glover MJ, Bennett MS, Chadwick R, Pittman MA, Quinnell TG (2016) Meta-analysis of randomised controlled trials of oral mandibular advancement devices and continuous positive airway pressure for obstructive sleep apnoea-hypopnoea. Sleep Med Rev 27:108–124. https://doi.org/10.1016/j.smrv.2015.05.003
Iftikhar IH, Bittencourt L, Youngstedt SD, Ayas N, Cistulli P, Schwab R, Durkin MW, Magalang UJ (2017) Comparative efficacy of CPAP, MADs, exercise-training, and dietary weight loss for sleep apnea: a network meta-analysis. Sleep Med 30:7–14. https://doi.org/10.1016/j.sleep.2016.06.001
Schwartz M, Acosta L, Hung YL, Padilla M, Enciso R (2018) Effects of CPAP and mandibular advancement device treatment in obstructive sleep apnea patients: a systematic review and meta-analysis. Sleep Breath 22(3):555–568. https://doi.org/10.1007/s11325-017-1590-6
Bratton DJ, Gaisl T, Wons AM, Kohler M (2015) CPAP vs mandibular advancement devices and blood pressure in patients with obstructive sleep apnea: a systematic review and meta-analysis. JAMA 314(21):2280–2293. https://doi.org/10.1001/jama.2015.16303
Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, Chervin RD (2015) Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med 11(7):773–827. https://doi.org/10.5664/jcsm.4858
Bamagoos AA, Cistulli PA, Sutherland K, Ngiam J, Burke PGR, Bilston LE, Butler JE, Eckert DJ (2019). Dose-dependent effects of mandibular advancement on upper airway collapsibility and muscle function in obstructive sleep apnea. Sleep 42(6):zsz049. https://doi.org/10.1093/sleep/zsz049
AADSM Mastery nomenclature for device classification. https://aadsm.org/docs/Mastery_Nomenclature_for_Device_Classification_-_FOR_ATTENDEES_FINAL_2-19-19.pdf. [Accessed 15th Apr 2022]
Ahrens A, McGrath C, Hagg U (2011) A systematic review of the efficacy of oral appliance design in the management of obstructive sleep apnoea. Eur J Orthod 33(3):318–324. https://doi.org/10.1093/ejo/cjq079
Bortolotti F, Corazza G, Bartolucci ML, Incerti Parenti S, Paganelli C, Alessandri-Bonetti G (2021) Dropout and adherence of obstructive sleep apnoea patients to mandibular advancement device therapy: a systematic review of randomised controlled trials with meta-analysis and meta-regression. J Oral Rehabil. https://doi.org/10.1111/joor.13290
Ishiyama H, Hasebe D, Sato K, Sakamoto Y, Furuhashi A, Komori E, Yuasa H (2019) The efficacy of device designs (mono-block or bi-block) in oral appliance therapy for obstructive sleep apnea patients: a systematic review and meta-analysis. Int J Environ Res Public Health 16(17):3182. https://doi.org/10.3390/ijerph16173182
Serra-Torres S, Bellot-Arcis C, Montiel-Company JM, Marco-Algarra J, Almerich-Silla JM (2016) Effectiveness of mandibular advancement appliances in treating obstructive sleep apnea syndrome: a systematic review. Laryngoscope 126(2):507–514. https://doi.org/10.1002/lary.25505
Venema J, Rosenmoller B, de Vries N, de Lange J, Aarab G, Lobbezoo F, Hoekema A (2021) Mandibular advancement device design: a systematic review on outcomes in obstructive sleep apnea treatment. Sleep Med Rev 60:101557. https://doi.org/10.1016/j.smrv.2021.101557
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, Mulrow C, Catala-Lopez F, Gotzsche PC, Dickersin K, Boutron I, Altman DG, Moher D (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162(11):777–784. https://doi.org/10.7326/M14-2385
Aarab G, Lobbezoo F, Hamburger HL, Naeije M (2011) Oral appliance therapy versus nasal continuous positive airway pressure in obstructive sleep apnea: a randomized, placebo-controlled trial. Respiration 81(5):411–419. https://doi.org/10.1159/000319595
Al-Dharrab A (2017) A randomized cross over study comparing the efficacy of two mandibular advancement appliances in the treatment of mild-moderate obstructive sleep apnea. Cranio 35(6):379–384. https://doi.org/10.1080/08869634.2016.1252563
Bishop B, Verrett R, Girvan T (2014) A randomized crossover study comparing two mandibular repositioning appliances for treatment of obstructive sleep apnea. Sleep Breath 18(1):125–131. https://doi.org/10.1007/s11325-013-0859-7
Blanco J, Zamarron C, Abeleira Pazos MT, Lamela C, Suarez Quintanilla D (2005) Prospective evaluation of an oral appliance in the treatment of obstructive sleep apnea syndrome. Sleep Breath 9(1):20–25. https://doi.org/10.1007/s11325-005-0003-4
Bloch KE, Iseli A, Zhang JN, Xie X, Kaplan V, Stoeckli PW, Russi EW (2000) A randomized, controlled crossover trial of two oral appliances for sleep apnea treatment. Am J Respir Crit Care Med 162(1):246–251. https://doi.org/10.1164/ajrccm.162.1.9908112
de Britto Teixeira AO, Abi-Ramia LB, de Oliveira Almeida MA (2013) Treatment of obstructive sleep apnea with oral appliances. Prog Orthod 14:10. https://doi.org/10.1186/2196-1042-14-10
Duran-Cantolla J, Crovetto-Martinez R, Alkhraisat MH, Crovetto M, Municio A, Kutz R, Aizpuru F, Miranda E, Anitua E (2015) Efficacy of mandibular advancement device in the treatment of obstructive sleep apnea syndrome: a randomized controlled crossover clinical trial. Med Oral Patol Oral Cir Bucal 20(5):e605-615. https://doi.org/10.4317/medoral.20649
Gauthier L, Laberge L, Beaudry M, Laforte M, Rompre PH, Lavigne GJ (2009) Efficacy of two mandibular advancement appliances in the management of snoring and mild-moderate sleep apnea: a cross-over randomized study. Sleep Med 10(3):329–336. https://doi.org/10.1016/j.sleep.2008.03.011
Ghazal A, Sorichter S, Jonas I, Rose EC (2009) A randomized prospective long-term study of two oral appliances for sleep apnoea treatment. J Sleep Res 18(3):321–328. https://doi.org/10.1111/j.1365-2869.2009.00738.x
Gotsopoulos H, Chen C, Qian J, Cistulli PA (2002) Oral appliance therapy improves symptoms in obstructive sleep apnea: a randomized, controlled trial. Am J Respir Crit Care Med 166(5):743–748. https://doi.org/10.1164/rccm.200203-208OC
Guimaraes TM, Poyares D, Oliveira ESL, Luz G, Coelho G, Dal Fabbro C, Tufik S, Bittencourt L (2021) The treatment of mild OSA with CPAP or mandibular advancement device and the effect on blood pressure and endothelial function after one year of treatment. J Clin Sleep Med 17(2):149–158. https://doi.org/10.5664/jcsm.8822
Hans MG, Nelson S, Luks VG, Lorkovich P, Baek SJ (1997) Comparison of two dental devices for treatment of obstructive sleep apnea syndrome (OSAS). Am J Orthod Dentofacial Orthop 111(5):562–570. https://doi.org/10.1016/s0889-5406(97)70293-2
Isacsson G, Nohlert E, Fransson AMC, Bornefalk-Hermansson A, Wiman Eriksson E, Ortlieb E, Trepp L, Avdelius A, Sturebrand M, Fodor C, List T, Schumann M, Tegelberg A (2019) Use of bibloc and monobloc oral appliances in obstructive sleep apnoea: a multicentre, randomized, blinded, parallel-group equivalence trial. Eur J Orthod 41(1):80–88. https://doi.org/10.1093/ejo/cjy030
Johnston CD, Gleadhill IC, Cinnamond MJ, Gabbey J, Burden DJ (2002) Mandibular advancement appliances and obstructive sleep apnoea: a randomized clinical trial. Eur J Orthod 24(3):251–262. https://doi.org/10.1093/ejo/24.3.251
Lam B, Sam K, Mok WY, Cheung MT, Fong DY, Lam JC, Lam DC, Yam LY, Ip MS (2007) Randomised study of three non-surgical treatments in mild to moderate obstructive sleep apnoea. Thorax 62(4):354–359. https://doi.org/10.1136/thx.2006.063644
Maguire J, Steele JG, Gibson GJ, Wilson JA, Steen N, McCracken GI (2010) Randomised cross-over study of oral appliances for snoring. Clin Otolaryngol 35(3):204–209. https://doi.org/10.1111/j.1749-4486.2010.02126.x
Marklund M, Carlberg B, Forsgren L, Olsson T, Stenlund H, Franklin KA (2015) Oral appliance therapy in patients with daytime sleepiness and snoring or mild to moderate sleep apnea: a randomized clinical trial. JAMA Intern Med 175(8):1278–1285. https://doi.org/10.1001/jamainternmed.2015.2051
Mehta A, Qian J, Petocz P, Darendeliler MA, Cistulli PA (2001) A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Crit Care Med 163(6):1457–1461. https://doi.org/10.1164/ajrccm.163.6.2004213
Naismith SL, Winter VR, Hickie IB, Cistulli PA (2005) Effect of oral appliance therapy on neurobehavioral functioning in obstructive sleep apnea: a randomized controlled trial. J Clin Sleep Med 1(4):374–380
Petri N, Svanholt P, Solow B, Wildschiodtz G, Winkel P (2008) Mandibular advancement appliance for obstructive sleep apnoea: results of a randomised placebo controlled trial using parallel group design. J Sleep Res 17(2):221–229. https://doi.org/10.1111/j.1365-2869.2008.00645.x
Quinnell TG, Bennett M, Jordan J, Clutterbuck-James AL, Davies MG, Smith IE, Oscroft N, Pittman MA, Cameron M, Chadwick R, Morrell MJ, Glover MJ, Fox-Rushby JA, Sharples LD (2014) A crossover randomised controlled trial of oral mandibular advancement devices for obstructive sleep apnoea-hypopnoea (TOMADO). Thorax 69(10):938–945. https://doi.org/10.1136/thoraxjnl-2014-205464
Rose E, Staats R, Virchow C, Jonas IE (2002) A comparative study of two mandibular advancement appliances for the treatment of obstructive sleep apnoea. Eur J Orthod 24(2):191–198. https://doi.org/10.1093/ejo/24.2.191
Sari E, Menillo S (2011) Comparison of titratable oral appliance and mandibular advancement splint in the treatment of patients with obstructive sleep apnea. ISRN Dent 2011:581692. https://doi.org/10.5402/2011/581692
Schneiderman E, Schramm P, Hui J, Wilson PD, Moura P, German Z, McCann A, Newton M (2021) Randomized trial of 2 self-titrated oral appliances for airway management. J Dent Res 100(2):155–162. https://doi.org/10.1177/0022034520956977
Tegelberg A, Nohlert E, Bornefalk-Hermansson A, Fransson A, Isacsson G (2020) Respiratory outcomes after a 1-year treatment of obstructive sleep apnoea with bibloc versus monobloc oral appliances: a multicentre, randomized equivalence trial. Acta Odontol Scand 78(6):401–408. https://doi.org/10.1080/00016357.2020.1730436
Vanderveken OM, Devolder A, Marklund M, Boudewyns AN, Braem MJ, Okkerse W, Verbraecken JA, Franklin KA, De Backer WA, Van de Heyning PH (2008) Comparison of a custom-made and a thermoplastic oral appliance for the treatment of mild sleep apnea. Am J Respir Crit Care Med 178(2):197–202. https://doi.org/10.1164/rccm.200701-114OC
Zhou J, Liu YH (2012) A randomised titrated crossover study comparing two oral appliances in the treatment for mild to moderate obstructive sleep apnoea/hypopnoea syndrome. J Oral Rehabil 39(12):914–922. https://doi.org/10.1111/joor.12006
Yanamoto S, Harata S, Miyoshi T, Nakamura N, Sakamoto Y, Murata M, Soutome S, Umeda M (2021) Semi-fixed versus fixed oral appliance therapy for obstructive sleep apnea: a randomized crossover pilot study. J Dent Sci 16(1):404–409. https://doi.org/10.1016/j.jds.2020.08.005
Norrhem N, Marklund M (2016) An oral appliance with or without elastic bands to control mouth opening during sleep-a randomized pilot study. Sleep Breath 20(3):929–938. https://doi.org/10.1007/s11325-016-1312-5
Bartolucci ML, Bortolotti F, Corazza G, Incerti Parenti S, Paganelli C, Alessandri Bonetti G (2021) Effectiveness of different mandibular advancement device designs in obstructive sleep apnoea therapy: a systematic review of randomised controlled trials with meta-analysis. J Oral Rehabil 48(4):469–486. https://doi.org/10.1111/joor.13077
Cartwright RD (1984) Effect of sleep position on sleep apnea severity. Sleep 7(2):110–114. https://doi.org/10.1093/sleep/7.2.110
Lee CH, Jung HJ, Lee WH, Rhee CS, Yoon IY, Yun PY, Kim JW (2012) The effect of positional dependency on outcomes of treatment with a mandibular advancement device. Arch Otolaryngol Head Neck Surg 138(5):479–483. https://doi.org/10.1001/archoto.2012.452
Takaesu Y, Tsuiki S, Kobayashi M, Komada Y, Nakayama H, Inoue Y (2016) Mandibular advancement device as a comparable treatment to nasal continuous positive airway pressure for positional obstructive sleep apnea. J Clin Sleep Med 12(8):1113–1119. https://doi.org/10.5664/jcsm.6048
Iftikhar IH (2016) MADs and positional sleep apnea: more than meets the eye! J Clin Sleep Med 12(8):1079–1080. https://doi.org/10.5664/jcsm.6036
Chen H, Eckert DJ, van der Stelt PF, Guo J, Ge S, Emami E, Almeida FR, Huynh NT (2020) Phenotypes of responders to mandibular advancement device therapy in obstructive sleep apnea patients: a systematic review and meta-analysis. Sleep Med Rev 49:101229. https://doi.org/10.1016/j.smrv.2019.101229
Lee WH, Wee JH, Lee CH, Kim MS, Rhee CS, Yun PY, Yoon IY, Kim JW (2013) Comparison between mono-bloc and bi-bloc mandibular advancement devices for obstructive sleep apnea. Eur Arch Otorhinolaryngol 270(11):2909–2913. https://doi.org/10.1007/s00405-013-2417-0
Author information
Authors and Affiliations
Contributions
IHI had full access to all extracted data in the network meta-analysis and takes responsibility for the integrity of the data and the accuracy of the data analysis. IHI conceptualized and designed the study protocol, extracted data, conducted the analyses, and wrote the first draft manuscript. HJ contributed to the study quality assessment. KA contributed to the database search. All authors contributed substantially to the interpretation of analyses and in revisions of the manuscript. All authors have seen and approved the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not required.
Informed consent
Not required.
Conflict of interest
IHI, ASB, JH, MS, AS, and KA have nothing to disclose. PAC has an appointment to an endowed academic Chair at the University of Sydney that was created from ResMed funding. He has received research support from ResMed, SomnoMed, Zephyr Sleep Technologies, and Bayer. He is a consultant/adviser to ResMed, SomnoMed, and Signifier Medical Technologies. He has a pecuniary interest in SomnoMed related to a previous role in R&D (2004). This study was not sponsored by any funding agency or pharmaceutical company.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Iftikhar, I.H., Cistulli, P.A., Jahrami, H. et al. Comparative efficacy of mandibular advancement devices in obstructive sleep apnea: a network meta-analysis. Sleep Breath 27, 1365–1381 (2023). https://doi.org/10.1007/s11325-022-02744-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02744-6