Abstract
Purpose
To investigate the prevalence of obstructive sleep apnea hypopnea syndrome (OSAHS) in patients undergoing off-pump coronary artery bypass grafting (OPCABG) and analyze the effects of OSAHS on the incidence of post-OPCABG complications, length of stay in intensive care unit (ICU) and hospitalization, and hospital expense.
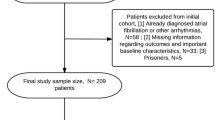
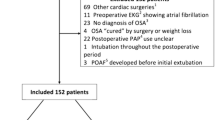
Materials and methods
This prospective study included patients undergoing OPCABG at Beijing An Zhen hospital from January 2018 to December 2018. OSAHS was diagnosed by using a portable sleep monitor before surgery.
Results
Among 74 patients, the prevalence of OSAHS and moderate to severe OSAHS (apnea hypopnea index (AHI) ≥ 15) was 70% and 53%, respectively. Compared with the no to mild OSAHS group (AHI < 15), the moderate to severe OSAHS group presented a lower ejection fraction (P = 0.013). Between these two groups, the incidence of post-OPCABG complications; the duration of intubation, ICU stay, and hospitalization; and the hospital expense did not differ. Notably, the ejection fraction was significantly negatively correlated with the duration of ICU stay and hospital expense.
Conclusions
Patients undergoing OPCABG with severe OSAHS are likely to exhibit a low ejection fraction and poor heart function, which may require a longer ICU stay and incur higher hospital expenses.


Similar content being viewed by others
Abbreviations
- AF:
-
Atrial fibrillation
- AHI:
-
Apnea hypopnea index
- BMI:
-
Body mass index
- CPAP:
-
Continuous positive airway pressure
- EF:
-
Ejection fraction
- ICU:
-
Intensive care unit
- OPCABG:
-
Off-pump coronary artery bypass grafting
- OSAHS:
-
Obstructive sleep apnea–hypopnea syndrome
- PG:
-
Polygraphy
- PSG:
-
Polysomnography
- SpO2 :
-
Blood oxygen saturation
- VA:
-
Ventricular arrhythmia
References
McEvoy RD, Antic NA, Heeley E, Luo Y, Ou Q, Zhang X et al (2016) SAVE Investigators and Coordinators. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med 375:919–31
Sforza E, Millasseau S, Hupin D, Barthélémy JC, Roche F (2019) Arterial stiffness alteration and obstructive sleep apnea in an elderly cohort free of cardiovascular event history: the PROOF cohort study. Sleep Breath 23(1):201–208
Yu Y, Gao MX, Wang C, Gu CX (2012) Bipolar radiofrequency ablation for left ventricular aneurysm related ventricular arrhythmia. J Thorac Cardiovasc Surg 144:101–102
Amra B, Niknam N, Sadeghi MM, Rabbani M, Fietze I, Penzel T (2014) Obstructive sleep apnea and postoperative complications in patients undergoing coronary artery bypass graft surgery: a need for preventive strategies. Int J Prev Med 5:1446–1451
Qaddoura A, Kabali C, Drew D, van Oosten EM, Michael KA, Redfearn DP et al (2014) Obstructive sleep apnea as a predictor of atrial fibrillation after coronary artery bypass grafting: a systematic review and meta-analysis. Can J Cardiol 30:1516–1522
Vecchiato M, Neunhaeuserer D, Quinto G, Bettini S, Gasperetti A, Battista F et al (2021) Cardiopulmonary exercise testing in patients with moderate-severe obesity: a clinical evaluation tool for OSA? Sleep Breath. https://doi.org/10.1007/s11325-021-02475-0
Gao M, Fan K, Yu W, Liu H, Wei Y, Yu Y (2007) The effects of high-sensitivity C-reactive protein on the clinical outcomes in obstructive sleep apnea patients undergoing off-pump coronary artery bypass grafting. BMC Cardiovasc Disord 21:366
Uchôa CH, Danzi-Soares Nde J, Nunes FS, de Souza AA, Nerbass FB, Pedrosa RP et al (2015) Impact of OSA on cardiovascular events after coronary artery bypass surgery. Chest 147:1352–1360
Ward NR, Roldao V, Cowie MR, Rosen SD, McDonagh TA, Simonds AK et al (2013) The effect of respiratory scoring on the diagnosis and classification of sleep disordered breathing in chronic heart failure. Sleep 36:1341–1348
Danzi-Soares NJ, Genta PR, Nerbass FB, Pedrosa RP, Soares FS, César LA et al (2012) Obstructive sleep apnea is common among patients referred for coronary artery bypass grafting and can be diagnosed by portable monitoring. Coron Artery Dis 23:31–38
van Oosten EM, Hamilton A, Petsikas D, Payne D, Redfearn DP, Zhang S et al (2014) Effect of preoperative obstructive sleep apnea on the frequency of atrial fibrillation after coronary artery bypass grafting. Am J Cardiol 113:919–923
Lee W, Nagubadi S, Kryger MH, Mokhlesi B (2008) Epidemiology of obstructive sleep apnea: a population-based perspective. Expert Rev Respir Med 2:349–364
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Cauley JA, Gutai JP, Glynn NW, Paternostro-Bayles M, Cottington E, Kuller LH (1994) Serum estrone concentrations and coronary artery disease in postmenopausal women. Arterioscler Thromb 14:14–18
Simon JA, Hunninghake DB, Agarwal SK, Lin F, Cauley JA, Ireland CC et al (2001) Effect of estrogen plus progestin on risk for biliary tract surgery in postmenopausal women with coronary artery disease. The heart and estrogen/progestin replacement study. Ann Intern Med 135:493–501
Mikami M, Tatsumi K, Kimura H, Honda Y, Kuriyama T (1989) Respiration effect of synthetic progestin in small doses in normal men. Chest 96:1073–1075
Whittle AT, Marshall I, Mortimore IL, Wraith PK, Sellar RJ, Douglas NJ (1999) Neck soft tissue and fat distribution: comparison between normal men and women by magnetic resonance imaging. Thorax 54:323–328
Ali SF, Smith EE, Reeves MJ, Zhao X, Xian Y, Hernandez AF et al (2015) Smoking paradox in patients hospitalized with coronary artery disease or acute ischemic stroke: findings from Get with the Guidelines. Circ Cardiovasc Qual Outcomes 8:S73–S80
Malerba M, Montuschi P (2012) Non-invasive biomarkers of lung inflammation in smoking subjects. Curr Med Chem 19:187–196
Taillé C, Rouvel-Tallec A, Stoica M, Danel C, Dehoux M, Marin-Esteban V et al (2016) Obstructive sleep apnoea modulates airway inflammation and remodelling in severe asthma. PLoS One 11:e0150042
Wang J, Yu W, Gao M, Zhang F, Gu C, Yu Y et al (2015) Impact of obstructive sleep apnea syndrome per se on endothelial function, arterial stiffening, and serum inflammatory markers: an update meta-analysis and meta-regression of 18 studies. JAHA 4:e002454
Hall AB, Ziadi MC, Leech JA, Chen SY, Burwash IG, Renaud J et al (2014) Effects of short-term continuous positive airway pressure on myocardial sympathetic nerve function and energetics in patients with heart failure and obstructive sleep apnea: a randomized study. Circulation 130:892–901
Bitter T, Fox H, Dimitriadis Z, Niedermeyer J, Prib N, Prinz C et al (2014) Circadian variation of defibrillator shocks in patients with chronic heart failure: the impact of Cheyne-Stokes respiration and obstructive sleep apnea. Int J Cardiol 176:1033–1035
Li S, Feng J, Wei S, Qian X, Cao J, Chen B (2016) Delayed neutrophil apoptosis mediates intermittent hypoxia-induced progressive heart failure in pressure-overloaded rats. Sleep Breath 20:95–102
Gami AS, Hodge DO, Herges RM, Olson EJ, Nykodym J, Kara T et al (2007) Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J Am Coll Cardiol 49:565–571
Miller JD, Aronis KN, Chrispin J, Patil KD, Marine JE, Martin SS et al (2015) Obesity, exercise, obstructive sleep apnea, and modifiable atherosclerotic cardiovascular disease risk factors in atrial fibrillation. J Am Coll Cardiol 66:2899–2906
Wong JK, Maxwell BG, Kushida CA, Sainani KL, Lobato RL, Woo YJ et al (2015) Obstructive sleep apnea is an independent predictor of postoperative atrial fibrillation in cardiac surgery. J Cardiothorac Vasc Anesth 29:1140–1147
Mooe T, Gullsby S, Rabben T, Eriksson P (1996) Sleep-disordered breathing: a novel predictor of atrial fibrillation after coronary artery bypass surgery. Coron Artery Dis 7:475–478
Abuelo JG (2015) Low dialysate potassium concentration: an overrated risk factor for cardiac arrhythmia? Semin Dial 28:266–275
Huang B, Zhou X, Wang Z, Wang S, Yu L, Jiang H (2015) Extracardiac autonomic modulations: potential therapeutic options for myocardial ischemia-induced ventricular arrhythmia. Int J Cardiol 188:45–46
Raghuram A, Clay R, Kumbam A, Tereshchenko LG, Khan A (2014) A systematic review of the association between obstructive sleep apnea and ventricular arrhythmias. J Clin Sleep Med 10:1155–1160
Wang J, Yu W, Gao M, Zhang F, Li Q, Gu C et al (2015) Continuous positive airway pressure treatment reduce cardiovascular death and non-fatal cardiovascular events in patients with obstructive sleep apnea: a meta-analysis of 11 studies. Int J Cardiol 191:218–231
Acknowledgements
The authors of this study would like to thank all the study participants.
Funding
This study was supported by the International Science & Technology Cooperation Program of China (No. 2015DFA30160), Beijing Municipal Science & Technology Commission (No. Z141100006014057), and Beijing Municipal Administration of Hospitals Ascent Plan under Grant (No. DFL20150602). These three funds had provided portable sleep monitors for the research. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Board of Beijing An Zhen Hospital of Capital Medical University (Approval No: 2013025).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gao, M., Wang, P., Tang, T. et al. Effects of obstructive sleep apnea hypopnea syndrome on postoperative complications in patients who undergo off-pump coronary artery bypass grafting. Sleep Breath 26, 1897–1905 (2022). https://doi.org/10.1007/s11325-022-02649-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02649-4