Abstract
Purpose
To evaluate the effect of long-term continuous positive airway pressure (CPAP) treatment on disease severity of obstructive sleep apnea (OSA).
Methods
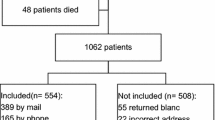
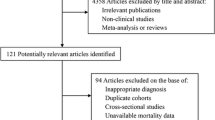
We analyzed results from the Sleep Apnea and Cardiovascular Events (SAVE) study involving participants recruited at the Guangdong Provincial People’s Hospital, China. Participants were aged 45–75 years with a history of cardiac or cerebrovascular disease. OSA was confirmed by home sleep apnea testing (HSAT). Participants were randomized to receive CPAP plus standard cardiovascular care (CPAP group) or standard care alone (UC group) and followed for several years. At the study conclusion, surviving participants were invited to repeat HSAT. Changes in OSA indicators were compared by independent samples t-tests and subgroup analysis was implied among groups stratified by OSA severity.
Results
One hundred two adults were recruited (51 per group) and followed for 48.0 ± 14.5 months. Daily CPAP usage in the CPAP group was 4.1 ± 1.9 h. AHI decreased from baseline to end-of-study in both CPAP and UC groups (− 5.0 (− 12.5,2.0), P = 0.000; − 4.0 (− 12.5,1.5), P = 0.007, respectively), with no between-group difference (P = 0.453). An improvement in nadir SpO2 showed from baseline to end-of-study in the CPAP but not UC group (2.3% ± 6.1%, P = 0.011 and − 0.7% ± 7.6%, P = 0.511, respectively; between-group difference P = 0.032). Subgroup analysis shows that CPAP could improve AHI in patients with moderate OSA (− 8.0 (− 11.8, − 2.8) in CPAP group, − 2.0 (− 0.8,6.0) in UC group, P = 0.022) and improve nadir SpO2 in patients with severe OSA (5.0 (− 0.8, − 0.8,7.0) in CPAP group, 0.0 (− 8.5,2.5) in UC group, P = 0.032).
Conclusion
Long-term CPAP use did not result in clinically significant changes in AHI or ODI overall but showed variable effects stratified by OSA severity.
Clinical Trial Registration
Registry: Clinical Trials.gov, title: Continuous Positive Airway Pressure Treatment of Obstructive Sleep Apnea to Prevent Cardiovascular Disease (SAVE), URL: www.clinicaltrials.gov, identifier: NCT00738179.


Similar content being viewed by others
Data availability
The detailed participant data are available from the corresponding author upon reasonable request.
References
Lévy P, Kohler M, McNicholas WT, Barbé F, McEvoy RD, Somers VK, Lavie L, Pépin J-L (2015) Obstructive sleep apnoea syndrome. Nat Rev Dis Primers 1:15015
Iftikhar IH, Bittencourt L, Youngstedt SD, Ayas N, Cistulli P, Schwab R, Durkin MW, Magalang UJ (2017) Comparative efficacy of CPAP, MADs, exercise-training, and dietary weight loss for sleep apnea: a network meta-analysis. Sleep Med 30:7–14
Radovanovic D, Rizzi M, Airoldi A, Mantero M, Di Marco F, Raccanelli R, Santus P (2019) Effect of continuous positive airway pressure on respiratory drive in patients with obstructive sleep apnea. Sleep Med 64
Dewan NA, Nieto FJ, Somers VK (2015) Intermittent hypoxemia and OSA: implications for comorbidities. Chest 147:266–274
Saboisky JP, Butler JE, Gandevia SC, Eckert DJ (2012) Functional role of neural injury in obstructive sleep apnea. Front Neurol 3:95
Eckert DJ, Younes MK (2014) Arousal from sleep: implications for obstructive sleep apnea pathogenesis and treatment. J Appl Physiol (Bethesda, Md.: 1985) 116:302–313
Kohler M, Stoewhas A-C, Ayers L, Senn O, Bloch KE, Russi EW, Stradling JR (2011) Effects of continuous positive airway pressure therapy withdrawal in patients with obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 184:1192–1199
Rolfe I, Olson LG, Saunders NA (1991) Long-term acceptance of continuous positive airway pressure in obstructive sleep apnea. Am Rev Respir Dis 144:1130–1133
McEvoy RD, Thornton AT (1984) Treatment of obstructive sleep apnea syndrome with nasal continuous positive airway pressure. Sleep 7:313–325
Young LR, Taxin ZH, Norman RG, Walsleben JA, Rapoport DM, Ayappa I (2013) Response to CPAP withdrawal in patients with mild versus severe obstructive sleep apnea/hypopnea syndrome. Sleep 36:405–412
Kribbs NB, Pack AI, Kline LR, Getsy JE, Schuett JS, Henry JN, Maislin G, Dinges DF (1993) Effects of one night without nasal CPAP treatment on sleep and sleepiness in patients with obstructive sleep apnea. Am Rev Respir Dis 147:1162–1168
Song P, Kim S, Kim D, Joo EY, Hong SB (2012) Long term effects of continuous positive airway pressure in obstructive sleep apnea patients: apnea-hypopnea index and blood pressure changes. Sleep Med Res 3:20–26
Rossi VA, Schwarz EI, Bloch KE, Stradling JR, Kohler M (2014) Is continuous positive airway pressure necessarily an everyday therapy in patients with obstructive sleep apnoea? Eur Respir J 43:1387–1393
McEvoy RD, Antic NA, Heeley E, Luo Y, Ou Q, Zhang X, Mediano O, Chen R, Drager LF, Liu Z, Chen G, Du B, McArdle N, Mukherjee S, Tripathi M, Billot L, Li Q, Lorenzi-Filho G, Barbe F, Redline S, Wang J, Arima H, Neal B, White DP, Grunstein RR, Zhong N, Anderson CS (2016) CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med 375:919–931
Ou Q, Chen B, Loffler KA, Luo Y, Zhang X, Chen R, Wang Q, Drager LF, Lorenzi-Filho G, Hlavac M, McArdle N, Mukherjee S, Mediano O, Barbe F, Anderson CS, McEvoy RD, Woodman RJ (2019) the effects of long-term CPAP on weight change in patients with comorbid OSA and cardiovascular disease: data from the SAVE trial. Chest 155:720–729
Antic NA, Heeley E, Anderson CS, Luo Y, Wang J, Neal B, Grunstein R, Barbe F, Lorenzi-Filho G, Huang S, Redline S, Zhong N, McEvoy RD (2015) The Sleep Apnea cardioVascular Endpoints (SAVE) Trial: rationale, ethics, design, and progress. Sleep 38:1247–1257
Heeley E, Billot L, Anderson CS, Antic NA, Neal B, McEvoy RD (2016) Statistical analysis plan for the Sleep Apnea cardioVascular Endpoints study: an international randomised controlled trial to determine whether continuous positive airways pressure treatment for obstructive sleep apnea in patients with CV disease prevents secondary cardiovascular events. Int J Stroke 11:148–150
Collop NA, Anderson WM, Boehlecke B, Claman D, Goldberg R, Gottlieb DJ, Hudgel D, Sateia M, Schwab R (2007) Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. J Clin Sleep Med 3:737
Godin G, Shephard RJ (1985) A simple method to assess exercise behavior in the community. Canadian journal of applied sport sciences. Can J Appl Sport Sci 10:141–146
Yesavage JA, Kinoshita LM, Noda A, Lazzeroni LC, Fairchild JK, Friedman L, Sekhon G, Thompson S, Cheng J, Zeitzer JM (2014) Longitudinal assessment of sleep disordered breathing in Vietnam veterans with post-traumatic stress disorder. Nat Sci Sleep 6:123–127
Sforza E, Addati G, Cirignotta F, Lugaresi E (1994) Natural evolution of sleep apnoea syndrome: a five year longitudinal study. Eur Respir J 7:1765–1770
Sforza E, Hupin D, Pichot V, Barthélémy JC, Roche F (2017) A 7-year follow-up study of obstructive sleep apnoea in healthy elderly: The PROOF cohort study. Respirology (Carlton, Vic.) 22:1007–1014
Mortimore IL, Kochhar P, Douglas NJ (1996) Effect of chronic continuous positive airway pressure (CPAP) therapy on upper airway size in patients with sleep apnoea/hypopnoea syndrome. Thorax 51:190–192
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med 15:335–343
Gantner D, Ge JY, Li LH, Antic N, Windler S, Wong K, Heeley E, Huang SG, Cui P, Anderson C, Wang JG, McEvoy D (2010) Diagnostic accuracy of a questionnaire and simple home monitoring device in detecting obstructive sleep apnoea in a Chinese population at high cardiovascular risk. Respirology 15:952–960
Acknowledgements
We gratefully thank the Statistics Office, Information and Statistics Center, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences) for excellent statistical assistance in this work.
Funding
The Sleep Apnea Cardiovascular Endpoints (SAVE) trial was funded by project grants [1006501 and 1060078] from the National Health and Medical Research Council of Australia and by the Respironics Sleep and Respiratory Research Foundation and Philips Respironics. Supplementary funding was provided by Fisher & Paykel Healthcare and the Australasian Sleep Trials Network [enabling grant 343020 from the National Health and Medical Research Council]. In-kind donations were provided by Respironics for the CPAP equipment and by ResMed for the sleep apnea diagnostic devices. This sub-study was supported by a grant [National Natural Science Foundation of China 81870077] to Q. O.
Author information
Authors and Affiliations
Contributions
The study was designed by DM, QO, KL, and YC; data were collected by YC, QO, BC, YX, QW, and ML; data were analyzed by YC and results interpreted by all authors. The manuscript and figures were drafted by YC and critically revised by QO, DM, and KL. QO serves as the guarantor of the paper, taking responsibility for the integrity of the work as a whole, from inception to publication of the article.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Participants signed ethics committee-approved consent forms prior to participation.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cheng, Y., Ou, Q., Chen, B. et al. The changes of AHI after long-term CPAP in patients with comorbid OSA and cardiovascular disease. Sleep Breath 27, 511–518 (2023). https://doi.org/10.1007/s11325-022-02633-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02633-y