Abstract
Background
This international study aimed at determining current routine palate surgeries and surgical methods adopted by otolaryngologists who practice surgical management of obstructive sleep apnea (OSA).
Methods
An international online survey was developed with the collaboration of the YO-IFOS (Young Otolaryngologists-International Federation of Otorhinolaryngological Societies) to assess the current routines in palatal procedures. The surgeons were asked 33 multiple-choice questions.
Results
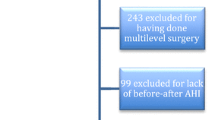
A total of 141 sleep surgeons answered the questionnaire, of whom 27% were from Africa, 30% from Asia, 24% from Centre-South America, and 19% from Europe. According to otolaryngology surgical specialties, 51% were sleep surgeons, 31% general ENTs, 8% Rhinologists, 7% Head & Neck surgeons, 2% otologists, and 1% maxillofacial surgeons. Of the 141 respondents, 51% answered they were sleep specialists, whereas 49% were non-sleep specialists. According to specific medical degree, 38% were specialists, 33% were consultants, 25% were professors, and 4% were residents or trainees.
Conclusion
This study gives an overview of the current surgical practice in OSA management in otolaryngology in different countries.
Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study was available from the corresponding author on reasonable request.
References
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ et al (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7(8):687–698
Gottlieb DJ, Punjabi NM (2020) Diagnosis and management of obstructive sleep apnea: a review. JAMA - J Am Med Assoc 323(14):1380–1400
Aurora RN, Casey KR, Kristo D, Auerbach S, Bista SR, Chowdhuri S et al (2010) Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults. Sleep 33(10):1408–1413
De Vito A, Woodson BT, Koka V, Cammaroto G, Iannella G, Bosi M et al (2021) OSA upper airways surgery: a targeted approach. Medicina (Kaunas) [Internet]. 57(7). Available from: http://www.ncbi.nlm.nih.gov/pubmed/34356971
Ja P (2016) Lessons from 50 years of uvulopalatopharyngoplasty. J Sleep Disord Ther 5(3):3–5
Pang KP, Baptista PM, Olszewska E, Braverman I, Carrasco-Llatas M, Kishore S et al (2020) Does drug-induced sleep endoscopy affect surgical outcome? A multicenter study of 326 obstructive sleep apnea patients. Laryngoscope [Internet]. 130(2):551–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30993741
Cammaroto G, Bianchi G, Zhang H, Veer V, Kotecha B, Jacobowitz O et al (2020) Sleep medicine in otolaryngology units: an international survey. Sleep Breath
Fakhry N, Teissier N (2019) Young otolaryngologists of the International Federation of Oto-rhino-laryngological Societies (YO-IFOS). Eur Ann Otorhinolaryngol Head Neck Dis [Internet]. 136(3):S1. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1879729619300638
Ayad T, Stephenson K, (A.L.) Smit D, Ben-Ari O, Késmárszky R, Lechien JR et al (2018) Young Otolaryngologists of International Federation of Oto-rhino-laryngological Societies (YO-IFOS) committees. Eur Ann Otorhinolaryngol Head Neck Dis [Internet]. 135(5):S61–5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1879729618301194
Mantovani M, Minetti A, Torretta S, Pincherle A, Tassone G, Pignataro L (2012) The velo-uvulo-pharyngeal lift or “roman blinds” technique for treatment of snoring: a preliminary report. Acta Otorhinolaryngol Ital [Internet]. 32(1):48–53. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22500068%0A, http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC3324968
Mantovani M, Rinaldi V, Torretta S, Carioli D, Salamanca F, Pignataro L (2016) Barbed Roman blinds technique for the treatment of obstructive sleep apnea: how we do it? Eur Arch Oto-Rhino-Laryngology [Internet]. 273(2):517–23. Available from: http://link.springer.com/10.1007/s00405-015-3726-2
Vicini C, Meccariello G, Montevecchi F, De Vito A, Frassineti S, Gobbi R et al (2020) Effectiveness of barbed repositioning pharyngoplasty for the treatment of obstructive sleep apnea (OSA): a prospective randomized trial. Sleep Breath [Internet]. 24(2):687–94. Available from: http://link.springer.com/10.1007/s11325-019-01956-7
Quesada P, Pedro-Botet J, Fuentes E et al (1979) Reseccion parcial del paladar blando como tratamiento del sındrome de hipersomia y respiracion periodica de los obesos. Acta Otorrinolaringol Esp 30:119–124
Fujita S, Conway W, Zorick F, Roth T (1981) Surgical correction of anatomic azbnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 89(06):923–934
Ikematsu T (1964) Study of snoring, fourth report. Therapy Japan. J Oto- Rhino-Laryngol 64:434–435
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep [Internet]. 19(2):156–77. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8855039
Rashwan MS, Montevecchi F, Cammaroto G, Badr el Deen M, Iskander N, El Hennawi D et al (2018) Evolution of soft palate surgery techniques for obstructive sleep apnea patients: a comparative study for single-level palatal surgeries. Clin Otolaryngol 43(2):584–90
Neruntarat C, Khuancharee K, Saengthong P (2021) Barbed reposition pharyngoplasty versus expansion sphincter pharyngoplasty: a meta-analysis. Laryngoscope [Internet]. 131(6):1420–8. Available from: https://onlinelibrary.wiley.com/doi/10.1002/lary.29357
Pang KP, Vicini C, Montevecchi F, Piccin O, Chandra S, Yang HC et al (2020) Long-term complications of palate surgery: a multicenter study of 217 patients. Laryngoscope [Internet]. 130(9):2281–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31765026
Camacho M, Li D, Kawai M, Zaghi S, Teixeira J, Senchak AJ et al (2016) Tonsillectomy for adult obstructive sleep apnea: a systematic review and meta-analysis. Laryngoscope [Internet]. 126(9):2176–86. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27005314
Baudouin R, Blumen M, Chaufton C, Chabolle F (2019) Adult sleep apnea and tonsil hypertrophy: should pharyngoplasty be associated with tonsillectomy? Sleep Breath [Internet]. 23(3):917–23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31115738
Sommer JU, Heiser C, Gahleitner C, Herr RM, Hörmann K, Maurer JT et al (2016) Tonsillectomy with uvulopalatopharyngoplasty in obstructive sleep apnea. Dtsch Aerzteblatt Online [Internet]. Available from: https://www.aerzteblatt.de/10.3238/arztebl.2016.0001
Pang KP, Montevecchi F, Vicini C, Carrasco-Llatas M, Baptista PM, Olszewska E et al (2020) Does nasal surgery improve multilevel surgical outcome in obstructive sleep apnea: a multicenter study on 735 patients. Laryngoscope Investig Otolaryngol [Internet]. 5(6):1233–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/33364416
Green KK, Kent DT, D’Agostino MA, Hoff PT, Lin H-S, Soose RJ et al (2019) Drug-induced sleep endoscopy and surgical outcomes: a multicenter cohort study. Laryngoscope [Internet]. 129(3):761–70. Available from: https://onlinelibrary.wiley.com/doi/10.1002/lary.27655
Hsu Y-S, Jacobowitz O (2017) Does sleep endoscopy staging pattern correlate with outcome of advanced palatopharyngoplasty for moderate to severe obstructive sleep apnea? J Clin Sleep Med [Internet]. 13(10):1137–44. Available from: http://jcsm.aasm.org/doi/10.5664/jcsm.6756
Salzano G, Maglitto F, Bisogno A, Vaira LA, De Riu G, Cavaliere M et al (2021) Obstructive sleep apnoea/hypopnoea syndrome: relationship with obesity and management in obese patients. Acta Otorhinolaryngol Ital [Internet]. 41(2):120–30. Available from: https://www.actaitalica.it/article/view/1100
Cahali MB (2003) Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope 113(11):1961–1968
Gulotta G, Iannella G, Meccariello G, Cammaroto G, Visconti IC, de Vincentiis M et al (2021) Barbed suture extrusion and exposure in palatoplasty for OSA: what does it mean? Am J Otolaryngol - Head Neck Med Surg 42(4):102994
Ravesloot MJL, De Raaff CAL, Van De Beek MJ, Benoist LBL, Beyers J, Corso RM et al (2019) Perioperative care of patients with obstructive sleep apnea undergoing upper airway surgery: a review and consensus recommendations. Vol. 145, JAMA Otolaryngology - Head and Neck Surgery. American Medical Association; p. 751–60
Meoli AL, Rosen CL, Kristo D, Kohrman M, Gooneratne N, Aguillard RN et al (2003) Upper airway management of the adult patient with obstructive sleep apnea in the perioperative period—avoiding complications. Vol. 26, Sleep. American Academy of Sleep Medicine; 1060–5
Practice guidelines for the perioperative management of patients with obstructive sleep apnea. Vol. 120, Anesthesiology. 2014. p. 268–86
Abdelhamid AO, Sobhy TS, El-Mehairy HM, Hamid O (2019) Role of antibiotics in post-tonsillectomy morbidities; a systematic review. Int J Pediatr Otorhinolaryngol [Internet]. 118:192–200. Available from
Author information
Authors and Affiliations
Contributions
AB, MC, and GC formulated the survey, AB collected answers, GC and HDS analyzed the statistics. UA and HDS wrote the manuscript. All authors read and revised the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethics committee of Alexandria University approved this study.
Consent for publication
Not applicable
Competing interests
All authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix Palate surgery questionnaire
Appendix Palate surgery questionnaire








Rights and permissions
About this article
Cite this article
Bahgat, A., Alkan, U., Carrasco Ilatas, M. et al. International palate surgery questionnaire. Sleep Breath 27, 569–590 (2023). https://doi.org/10.1007/s11325-022-02631-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02631-0