Abstract
Purpose
This study aimed to develop a machine learning–based questionnaire (BASH-GN) to classify obstructive sleep apnea (OSA) risk by considering risk factor subtypes.
Methods
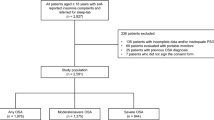
Participants who met study inclusion criteria were selected from the Sleep Heart Health Study Visit 1 (SHHS 1) database. Other participants from the Wisconsin Sleep Cohort (WSC) served as an independent test dataset. Participants with an apnea hypopnea index (AHI) ≥ 15/h were considered as high risk for OSA. Potential risk factors were ranked using mutual information between each factor and the AHI, and only the top 50% were selected. We classified the subjects into 2 different groups, low and high phenotype groups, according to their risk scores. We then developed the BASH-GN, a machine learning–based questionnaire that consists of two logistic regression classifiers for the 2 different subtypes of OSA risk prediction.
Results
We evaluated the BASH-GN on the SHHS 1 test set (n = 1237) and WSC set (n = 1120) and compared its performance with four commonly used OSA screening questionnaires, the Four-Variable, Epworth Sleepiness Scale, Berlin, and STOP-BANG. The model outperformed these questionnaires on both test sets regarding the area under the receiver operating characteristic (AUROC) and the area under the precision-recall curve (AUPRC). The model achieved AUROC (SHHS 1: 0.78, WSC: 0.76) and AUPRC (SHHS 1: 0.72, WSC: 0.74), respectively. The questionnaire is available at https://c2ship.org/bash-gn.
Conclusion
Considering OSA subtypes when evaluating OSA risk may improve the accuracy of OSA screening.


Similar content being viewed by others
Data availability
The datasets analyzed during the current study are publicly accessible via https://sleepdata.org/datasets/shhs and https://sleepdata.org/datasets/wsc.
References
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177:1006–1014
Gottlieb DJ, Punjabi NM (2020) Diagnosis and management of obstructive sleep apnea: a review. JAMA 323:1389–1400
Al Lawati NM, Patel SR, Ayas NT (2009) Epidemiology, risk factors, and consequences of obstructive sleep apnea and short sleep duration. Prog Cardiovasc Dis 51:285–293
Foster GD, Sanders MH, Millman R, Zammit G, Borradaile KE, Newman AB, Wadden TA, Kelley D, Wing RR, Sunyer FXP (2009) Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care 32:1017–1019
Harris M, Glozier N, Ratnavadivel R, Grunstein RR (2009) Obstructive sleep apnea and depression. Sleep Med Rev 13:437–444
Punjabi NM (2008) The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5:136–143
Mendonca F, Mostafa SS, Ravelo-Garcia AG, Morgado-Dias F, Penzel T (2019) A review of obstructive sleep apnea detection approaches. IEEE J Biomed Health Inform 23:825–837. https://doi.org/10.1109/JBHI.2018.2823265
Johns MW (1993) Daytime sleepiness, snoring, and obstructive sleep apnea: the Epworth Sleepiness Scale. Chest 103:30–36
Takegami M, Hayashino Y, Chin K, Sokejima S, Kadotani H, Akashiba T, Kimura H, Ohi M, Fukuhara S (2009) Simple four-variable screening tool for identification of patients with sleep-disordered breathing. Sleep 32:939–948
Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP (1999) Using the Berlin questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 131:485–491
Ong TH, Raudha S, Fook-Chong S, Lew N, Hsu A (2010) Simplifying STOP-BANG: use of a simple questionnaire to screen for OSA in an Asian population. Sleep and Breathing 14:371–376
Keenan BT, Kim J, Singh B, Bittencourt L, Chen NH, Cistulli PA, Magalang UJ, McArdle N, Mindel JW, Benediktsdottir B, Arnardottir ES, Prochnow LK, Penzel T, Sanner B, Schwab RJ, Shin C, Sutherland K, Tufik S, Maislin G, Gislason T, Pack AI (2018) Recognizable clinical subtypes of obstructive sleep apnea across international sleep centers: a cluster analysis. Sleep 41. https://doi.org/10.1093/sleep/zsx214
Kim J, Keenan BT, Lim DC, Lee SK, Pack AI, Shin C (2018) Mar 15) Symptom-based subgroups of Koreans with obstructive sleep apnea. J Clin Sleep Med 14:437–443. https://doi.org/10.5664/jcsm.6994
Quan SF, Howard BV, Iber C, Kiley JP, Nieto FJ, O’Connor GT, Rapoport DM, Redline S, Robbins J, Samet JM (1997) The sleep heart health study: design, rationale, and methods. Sleep 20:1077–1085
Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, Hla KM (2009) Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ Off Publ State Med Soc Wis 108:246
Zhang G-Q, Cui L, Mueller R, Tao S, Kim M, Rueschman M, Mariani S, Mobley D, Redline S (2018) The National Sleep Research Resource: towards a sleep data commons. J Am Med Inform Assoc 25:1351–1358
Yaggi HK, Strohl KP (2010) Adult obstructive sleep apnea/hypopnea syndrome: definitions, risk factors, and pathogenesis. Clin Chest Med 31:179
Koo P, McCool FD, Hale L, Stone K, Eaton CB (2016) Association of obstructive sleep apnea risk factors with nocturnal enuresis in postmenopausal women. Menopause (New York, NY) 23:175
Young T, Skatrud J, Peppard PE (2004) Risk factors for obstructive sleep apnea in adults. JAMA 291:2013–2016
Rundo JV (2019) Obstructive sleep apnea basics. Cleve Clin J Med 86:2–9
Buman MP, Kline CE, Youngstedt SD, Phillips B, De Mello MT, Hirshkowitz M (2015) Sitting and television viewing: novel risk factors for sleep disturbance and apnea risk? Results from the 2013 National Sleep Foundation Sleep in America Poll. Chest 147:728–734
Millman RP, Redline S, Carlisle CC, Assaf AR, Levinson PD (1991) Daytime hypertension in obstructive sleep apnea: prevalence and contributing risk factors. Chest 99:861–866
Hudgel DW (2016) Sleep apnea severity classification—revisited. Sleep 39:1165–1166
Ross BC (2014) Mutual information between discrete and continuous data sets. PLoS ONE 9:e87357
Kale SS, Kakodkar P, Shetiya SH (2018) Assessment of oral findings of dental patients who screen high and no risk for obstructive sleep apnea (OSA) reporting to a dental college-a cross sectional study. Sleep Science 11:112
Chung F, Abdullah HR, Liao P (2016) STOP-BANG questionnaire: a practical approach to screen for obstructive sleep apnea. Chest 149:631–638
Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF (2011) Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-BANG, and Epworth Sleepiness Scales. J Clin Sleep Med 7:467–472
Davis J, Goadrich M (2006) The relationship between Precision-Recall and ROC curves. Proceedings of the 23rd international conference on Machine learning, pp 233–240
Nagappa M, Wong J, Singh M, Wong DT, Chung F (2017) An update on the various practical applications of the STOP-BANG questionnaire in anesthesia, surgery, and perioperative medicine. Curr Opin Anaesthesiol 30:118
Chowdhuri S, Quan SF, Almeida F, Ayappa I, Batool-Anwar S, Budhiraja R, Cruse PE, Drager LF, Griss B, Marshall N (2016) An official American Thoracic Society research statement: impact of mild obstructive sleep apnea in adults. Am J Respir Crit Care Med 193:e37-54
Funding
National Science Foundation (#2052528) and National Heart, Lung, and Blood Institute (#R21HL159661-01) provided financial support in the form of research funding. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
For this type of study, formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Dr. Quan is a consultant from Bryte Bed, Whispersom, DR Capital and Best Doctors. Other authors have nothing to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Huo, J., Quan, S.F., Roveda, J. et al. BASH-GN: a new machine learning–derived questionnaire for screening obstructive sleep apnea. Sleep Breath 27, 449–457 (2023). https://doi.org/10.1007/s11325-022-02629-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02629-8