Abstract
Purpose
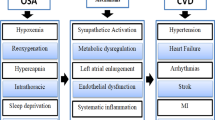
This study aimed to explore the role of hypoxia in the relationship between obstructive sleep apnea (OSA) and cardiovascular disease (CVD) death risk based on data from the Sleep Heart Health Study (SHHS).
Methods
Multivariate logistic regression analysis was used to analyze the association between OSA, hypoxia, and CVD death risk. Causal mediation analysis was performed to assess the role of hypoxia. The severity of OSA was evaluated by the apnea–hypopnea index (AHI), and the hypoxia was quantified by the percentage of sleep time with less than 90% oxygen saturation (PCTST90).
Results
Of these 5,145 participants, 989 had no OSA, 2,110 had mild OSA, and 2,046 had moderate-to-severe OSA. After adjusting all confounders, mild OSA [odds ratio (OR): 1.800; 95% confidence interval (CI), 1.192–2.802], moderate-to-severe OSA (OR: 1.745; 95%CI, 1.148–2.758), 0 < PCTST90 < 1 (OR: 1.668; 95%CI, 1.184–2.385), and PCTST90 ≥ 1 (OR: 1.649; 95%CI, 1.148–2.400) were associated with an increased death risk of CVD. Furthermore, participants with mild OSA (OR: 3.742; 95%CI, 3.183–4.398) and moderate-to-severe OSA (OR: 19.671; 95%CI, 16.303–23.734) had a higher risk of hypoxia than those without OSA. Causal mediation analysis indicated that the average direct effect (ADM) of moderate-to-severe OSA and average causal mediation effect (ACME) of hypoxia on CVD death risk were 0.024 (95%CI, 0.004–0.040) and 0.013 (95%CI, 0.005–0.020), respectively, and the average mediating effect ratio was 33.94%.
Conclusion
Hypoxia played a mediating role in the increased death risk of CVD caused by OSA, and the mediating effect of hypoxia did not account for a large proportion.





Similar content being viewed by others
Data availability
The dataset is available on request of corresponding author.
Abbreviations
- SHHS:
-
Sleep Heart Health Study
- AHI:
-
Apnea–hypopnea index
- PCTST90:
-
90% Oxygen saturation
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- ADM:
-
Average direct effect
- ACME:
-
Average causal mediation effect
- OSA:
-
Obstructive sleep apnea
- CVD:
-
Cardiovascular diseases
- HF:
-
Heart failure
- BMI:
-
Body mass index
- MI:
-
Myocardial infarction
- COPD:
-
Chronic obstructive pulmonary disease
- LIPID:
-
Lipid-lowering medication
- ACME:
-
Average causal mediation effect; SD: standard deviation
References
Gottlieb DJ (2020) Punjabi NM (2020) Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA 323:1389–1400
Lévy P, Kohler M, McNicholas WT, Barbé F, McEvoy RD, Somers VK et al (2015) Obstructive sleep apnoea syndrome. Nat Rev Dis Primers 1:15015
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177:1006–1014
Yu J, Zhou Z, McEvoy RD, Anderson CS, Rodgers A, Perkovic V et al (2017) Association of Positive Airway Pressure With Cardiovascular Events and Death in Adults With Sleep Apnea: A Systematic Review and Meta-analysis. JAMA 318:156–166
Floras JS (2018) Sleep Apnea and Cardiovascular Disease: An Enigmatic Risk Factor. Circ Res 122:1741–1764
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A et al (2008) Sleep apnea and cardiovascular disease: an American Heart Association/american College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation 118:1080–1111
Lévy P, Pépin JL, Arnaud C, Tamisier R, Borel JC, Dematteis M et al (2008) Intermittent hypoxia and sleep-disordered breathing: current concepts and perspectives. Eur Respir J 32:1082–1095
Oldenburg O, Wellmann B, Buchholz A, Bitter T, Fox H, Thiem U et al (2016) Nocturnal hypoxaemia is associated with increased mortality in stable heart failure patients. Eur Heart J 37:1695–1703
Baumert M, Immanuel SA, Stone KL, Litwack Harrison S, Redline S, Mariani S et al (2020) Composition of nocturnal hypoxaemic burden and its prognostic value for cardiovascular mortality in older community-dwelling men. Eur Heart J 41:533–541
Azarbarzin A, Sands SA, Taranto-Montemurro L, Vena D, Sofer T, Kim SW et al (2020) The Sleep Apnea-Specific Hypoxic Burden Predicts Incident Heart Failure. Chest 158:739–750
Sleep Heart Health Study (SHHS), https://biolincc.nhlbi.nih.gov/studies/shhs/. Accessed on March 3st, 2021.
Jaffe LM, Kjekshus J, Gottlieb SS (2013) Importance and management of chronic sleep apnoea in cardiology. Eur Heart J 34:809–815
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8:597–619
Variable description of the Sleep Heart Health Study (SHHS), https://sleepdata.org/datasets/ccshs/variables/pctlt90. Accessed on March 3st, 2021.
Zhang Z, Zheng C, Kim C, Van Poucke S, Lin S, Lan P (2016) Causal mediation analysis in the context of clinical research. Ann Transl Med 4:425
Strollo PJ Jr, Hedner J, Collop N, Lorch DG Jr et al (2019) Solriamfetol for the Treatment of Excessive Sleepiness in OSA: A Placebo-Controlled Randomized Withdrawal Study. Chest 155:364–374
Kawada T (2021) Obstructive sleep apnoea syndrome and cardiovascular risk with special reference to obesity and cognitive impairment. Sleep Med 77:14
Mazzotti DR, Keenan BT, Lim DC, Gottlieb DJ, Kim J, Pack AI (2019) Symptom Subtypes of Obstructive Sleep Apnea Predict Incidence of Cardiovascular Outcomes. Am J Respir Crit Care Med 200:493–506
Drager LF, McEvoy RD, Barbe F, Lorenzi-Filho G, Redline S (2017) Sleep Apnea and Cardiovascular Disease: Lessons From Recent Trials and Need for Team Science. Circulation 136:1840–1850
Baguet JP, Barone-Rochette G, Tamisier R, Levy P, Pépin JL (2012) Mechanisms of cardiac dysfunction in obstructive sleep apnea. Nat Rev Cardiol 9:679–688
Kohler M, Stradling JR (2010) Mechanisms of vascular damage in obstructive sleep apnea. Nat Rev Cardiol 7:677–685
Sánchez-de-la-Torre M, Campos-Rodriguez F, Barbé F (2013) Obstructive sleep apnoea and cardiovascular disease. Lancet Respir Med 1:61–72
Linz D, Loffler KA, Sanders P, Catcheside P, Anderson CS, Zheng D et al (2020) Prognostic Value of Novel Nocturnal Metrics in Patients With OSA and High Cardiovascular Event Risk: Post Hoc Analyses of the SAVE Study. Chest 158:2621–2631
Franczak A, Bil-Lula I, Sawicki G, Fenton M, Ayas N, Skomro R (2019) Matrix metalloproteinases as possible biomarkers of obstructive sleep apnea severity - A systematic review. Sleep Med Rev 46:9–16
Author information
Authors and Affiliations
Contributions
YZ and CL designed the study. YZ wrote the manuscript. XQT and JJL collected, analyzed, and interpreted the data. CL critically reviewed, edited, and approved the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This research analyzed de-identified information downloaded from the SHHS, which is exempt from future Institutional Review Board approval.
Manuscript approval
All authors declare that they have seen and approved the final version of the manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, Y., Tan, X., Lu, J. et al. Mediation effect of hypoxia in the relationship between obstructive sleep apnea and cardiovascular death risk. Sleep Breath 26, 1729–1737 (2022). https://doi.org/10.1007/s11325-022-02564-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02564-8