Abstract
Purpose
Allergic rhinitis (AR) is an independent risk factor for sleep disorders in children, including abnormal sleep behaviors. We investigated the occurrence of abnormal sleep behaviors in children with AR to determine indoor environmental risk factors affecting sleep.
Methods
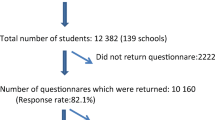
This case-control study collected the sleep status and characteristics of the indoor environment of children aged 3–14 years with and without AR using a questionnaire. The differences between the two groups were compared using the Mann–Whitney U test, chi-square test, and Fisher’s exact test. The indoor environmental factors affecting sleep behavior were analyzed using logistic regression analysis.
Results
Children with AR (n=427) had a higher probability of snoring (8.7 % vs. 2.9 %; P < 0.001), mouth breathing (14.1 % vs. 5.2 %; P < 0.001), restless sleep (6.6 % vs. 4.1 %; P = 0.047), sleep talking (3.3 % vs. 1.1 %; P = 0.003), and hyperhidrosis (16.4 % vs. 8.5 %; P < 0.001) than those without AR (n=1046). Emulsion wall paint (odds ratio (OR) = 2.779; 95 % confidence interval (CI), 1.332–5.796; P = 0.006) and tobacco exposure in early infancy (OR = 2.065; 95 % CI 1.079–3.950; P = 0.029) were associated with hyperhidrosis.
Conclusion
Children with AR are more likely to have abnormal sleep behaviors than those without, including snoring, mouth breathing, restless sleep, sleep talking, and hyperhidrosis. Emulsion paint wall and tobacco smoke exposure in early infancy had a twofold higher risk of hyperhidrosis during sleep.

Similar content being viewed by others
Availability of data and material
The datasets generated and/or analyzed during the current study are not publicly available due to data do not have consent from all patients to share their information online but are available from the corresponding author on reasonable request.
Code availability
Epidata Software v3.1 (Epidata Association, Odense, Denmark) and R program (version 3.6.2).
Abbreviations
- AR:
-
allergic rhinitis
- BMI:
-
body mass index
- OSAS:
-
obstructive sleep apnea syndrome
- OR:
-
odds ratio confidence interval
- SDB:
-
sleep-disordered breathing
- CI:
-
confidence interval
- IgE:
-
immunoglobulin E
- IQR:
-
interquartile range
- VOCs:
-
volatile organic compounds
References
Brożek JL, Bousquet J, Agache I et al (2017) Allergic rhinitis and its impact on asthma (ARIA) guidelines-2016 revision. J Allergy Clin Immunol 140:950–958. https://doi.org/10.1016/j.jaci.2017.03.050
Hu SJ, Wei P, Kou W et al (2017) Prevalence and risk factors of allergic rhinitis: a meta-analysis. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 31:1485–1491. https://doi.org/10.13201/j.issn.1001-1781.2017.19.006
Lavie P, Gertner R, Zomer J, Podoshin L (1981) Breathing disorders in sleep associated with “microarousals” in patients with allergic rhinitis. Acta Otolaryngol 92:529–533. https://doi.org/10.3109/00016488109133292
McNicholas WT, Tarlo S, Cole P et al (1982) Obstructive apneas during sleep in patients with seasonal allergic rhinitis. Am Rev Respir Dis 126:625–628. https://doi.org/10.1164/arrd.1982.126.4.625
Lin SY, Melvin TA, Boss EF, Ishman SL (2013) The association between allergic rhinitis and sleep-disordered breathing in children: a systematic review. Int Forum Allergy Rhinol 3:504–509. https://doi.org/10.1002/alr.21123
Chirakalwasan N, Ruxrungtham K (2014) The linkage of allergic rhinitis and obstructive sleep apnea. Asian Pac J Allergy Immunol 32:276–286
Cao Y, Wu S, Zhang L, Yang Y, Cao S, Li Q (2018) Association of allergic rhinitis with obstructive sleep apnea: a meta-analysis. Medicine (Baltimore) 97:e13783. https://doi.org/10.1097/MD.0000000000013783
Zheng M, Wang X, Zhang L (2018) Association between allergic and nonallergic rhinitis and obstructive sleep apnea. Curr Opin Allergy Clin Immunol 18:16–25. https://doi.org/10.1097/ACI.0000000000000414
Tsai JD, Chen HJ, Ku MS et al (2017) Association between allergic disease, sleep-disordered breathing, and childhood nocturnal enuresis: a population-based case-control study. Pediatr Nephrol 32:2293–2301. https://doi.org/10.1007/s00467-017-3750-0
Lai PH, Yang PS, Lai WY, Lin CL, Hsu CY, Wei CC (2018) Allergic rhinitis and the associated risk of nocturnal enuresis in children: a population-based cohort study. Int Forum Allergy Rhinol 8:1260–1266. https://doi.org/10.1002/alr.22219
Sateia MJ (2014) International classification of sleep disorders-third edition: highlights and modifications. Chest 146:1387–1394. https://doi.org/10.1378/chest.14-0970
Kheirandish-Gozal L, De Jong MR, Spruyt K, Chamuleau SA, Gozal D (2010) Obstructive sleep apnoea is associated with impaired pictorial memory task acquisition and retention in children. Eur Respir J 36:164–169. https://doi.org/10.1183/09031936.00114209
Carberry JC, Amatoury J, Eckert DJ (2018) Personalized management approach for OSA. Chest 153:744–755. https://doi.org/10.1016/j.chest.2017.06.011
Brockmann PE, Urschitz MS, Schlaud M, Poets CF (2012) Primary snoring in school children: prevalence and neurocognitive impairments. Sleep Breath 16:23–29. https://doi.org/10.1007/s11325-011-0480-6
Biggs SN, Nixon GM, Horne RS (2014) The conundrum of primary snoring in children: what are we missing in regards to cognitive and behavioural morbidity. Sleep Med Rev 18:463–475. https://doi.org/10.1016/j.smrv.2014.06.009
Beebe DW, Gozal D (2002) Obstructive sleep apnea and the prefrontal cortex: towards a comprehensive model linking nocturnal upper airway obstruction to daytime cognitive and behavioral deficits. J Sleep Res 11:1–16. https://doi.org/10.1046/j.1365-2869.2002.00289.x
Hahm MI, Chae Y, Kwon HJ et al (2014) Do newly built homes affect rhinitis in children? The ISAAC phase III study in Korea. Allergy 69:479–487. https://doi.org/10.1111/all.12355
Zacharasiewicz A, Zidek T, Haidinger G et al (2000) Symptoms suggestive of atopic rhinitis in children aged 6-9 years and the indoor environment. Allergy 55:945–950. https://doi.org/10.1034/j.1398-9995.2000.00575.x
Jaakkola JJ, Hwang BF, Jaakkola MS (2010) Home dampness and molds as determinants of allergic rhinitis in childhood: a 6-year, population-based cohort study. Am J Epidemiol 172:451–459. https://doi.org/10.1093/aje/kwq110
Wang J, Zhao Z, Zhang Y et al (2019) Asthma, allergic rhinitis and eczema among parents of preschool children in relation to climate, and dampness and mold in dwellings in China. Environ Int 130:104910. https://doi.org/10.1016/j.envint.2019.104910
Boulay ME, Boulet LP (2003) The relationships between atopy, rhinitis and asthma: pathophysiological considerations. Curr Opin Allergy Clin Immunol 3:51–55. https://doi.org/10.1097/00130832-200302000-00009
Bertelsen RJ, Instanes C, Granum B et al (2010) Gender differences in indoor allergen exposure and association with current rhinitis. Clin Exp Allergy 40:1388–1397. https://doi.org/10.1111/j.1365-2222.2010.03543.x
Packer CN, Stewart-Brown S, Fowle SE (1994) Damp housing and adult health: results from a lifestyle study in Worcester, England. J Epidemiol Community Health 48:555–559. https://doi.org/10.1136/jech.48.6.555
Janson C, Norbäck D, Omenaas E et al (2005) Insomnia is more common among subjects living in damp buildings. Occup Environ Med 62:113–118. https://doi.org/10.1136/oem.2003.011379
Tiesler CM, Thiering E, Tischer C et al (2015) Exposure to visible mould or dampness at home and sleep problems in children: results from the LISAplus study. Environ Res 137:357–363. https://doi.org/10.1016/j.envres.2014.11.023
Jedrychowski W, Maugeri U, Perera F et al (2011) Cognitive function of 6-year-old children exposed to mold-contaminated homes in early postnatal period. Prospective birth cohort study in Poland. Physiol Behav 104:989–995. https://doi.org/10.1016/j.physbeh.2011.06.019
Otolaryngology Professional Committees Pediatrician Branch, Chinese Medical Doctor Association (2019) Diagnosis and treatment of allergic rhinitis in children-guidelines for clinical practice. Chin J Pract Pediatr 34:169–175 (in Chinese). https://doi.org/10.19538/j.ek2019030601
Respirology Group, Chinese Medical Afterscience Branch, Editorial Board of Chinese Journal of Pediatrics (2016) Guidelines for the diagnosis and management of bronchial asthma in children (2016 Edition). Chin J Pediatr 54:167–181 (in Chinese). https://doi.org/10.3760/cma.j.issn.0578-1310.2016.03.003
Subspecialty Group of Rhinology, Editorial Board of Chinese Journal of Otorhinolaryngology Head and Neck Surgery; Subspecialty Group of Rhinology, Society of Otorhinolaryngology Head and Neck Surgery, Chinese Medical Association (2019) Chinese guidelines for diagnosis and treatment of chronic rhinosinusitis (2018). Chin J Otorhinolaryngol Head Neck Surg 54:81–100. https://doi.org/10.3760/cma.j.issn.1673-0860.2019.02.001
Owens JA, Spirito A, McGuinn M (2000) The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep 23:1043–1051
Paruthi S, Brooks LJ, D’Ambrosio CD et al (2016) Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med 12:785–786. https://doi.org/10.5664/jcsm.5866
Liu J, Wu Y, Wu P, Xu Z, Ni X (2020) Analysis of the impact of allergic rhinitis on the children with sleep disordered breathing. Int J Pediatr Otorhinolaryngol 138:110380. https://doi.org/10.1016/j.ijporl.2020.110380
Zhou S, Hur K, Shen J, Wrobel B (2017) Impact of sinonasal disease on depression, sleep duration, and productivity among adults in the United States. Laryngoscope Investig Otolaryngol 2:288–294. https://doi.org/10.1002/lio2.87
Bartel KA, Gradisar M, Williamson P (2015) Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Med Rev 21:72–85. https://doi.org/10.1016/j.smrv.2014.08.002
Liu JW, Tu YK, Lai YF et al (2019) Associations between sleep disturbances and suicidal ideation, plans, and attempts in adolescents: a systematic review and meta-analysis. Sleep 42:zsz054. https://doi.org/10.1093/sleep/zsz054
American Academy of Sleep Medicine (2014) International classification of sleep disorders, 3rd end edn. Academy of Sleep Medicine, Darien
Poachanukoon O, Kitcharoensakkul M (2015) Snoring and sleep problems in children with and without allergic rhinitis: a case control study. J Med Assoc Thail 98(Suppl 2):S138–S144
Sato K, Kang WH, Saga K, Sato KT (1989) Biology of sweat glands and their disorders. I. Normal sweat gland function. J Am Acad Dermatol 20:537–563. https://doi.org/10.1016/s0190-9622(89)70063-3
Sato K, Kang WH, Saga K, Sato KT (1989) Biology of sweat glands and their disorders. II. Disorders of sweat gland function. J Am Acad Dermatol 20:713–726. https://doi.org/10.1016/s0190-9622(89)70081-5
Lear W, Kessler E, Solish N, Glaser DA (2007) An epidemiological study of hyperhidrosis. Dermatol Surg 33:S69–S75. https://doi.org/10.1111/j.1524-4725.2006.32334.x
Liu J, Zhang X, Zhao Y, Wang Y (2020) The association between allergic rhinitis and sleep: a systematic review and meta-analysis of observational studies. PLoS One 15:e0228533. https://doi.org/10.1371/journal.pone.0228533
Shusterman D, Baroody FM, Craig T, Friedlander S, Nsouli T, Silverman B (2017) Role of the allergist-immunologist and upper airway allergy in sleep-disordered breathing. J Allergy Clin Immunol Pract 5:628–639. https://doi.org/10.1016/j.jaip.2016.10.007
Lung MA (1995) The role of the autonomic nerves in the control of nasal circulation. Biol Signals 4:179–185. https://doi.org/10.1159/000109439
Loehrl TA, Smith TL, Darling RJ et al (2002) Autonomic dysfunction, vasomotor rhinitis, and extraesophageal manifestations of gastroesophageal reflux. Otolaryngol Head Neck Surg 126:382–387. https://doi.org/10.1067/mhn.2002.123857
Mitchell RB, Garetz S, Moore RH et al (2015) The use of clinical parameters to predict obstructive sleep apnea syndrome severity in children: the Childhood Adenotonsillectomy (CHAT) study randomized clinical trial. JAMA Otolaryngol Head Neck Surg 141:130–136. https://doi.org/10.1001/jamaoto.2014.3049
Jiang RS, Liang KL, Hsin CH, Su MC (2016) The impact of chronic rhinosinusitis on sleep-disordered breathing. Rhinology 54:75–79. https://doi.org/10.4193/Rhino15.204
Wang X, Gao X, Yang Q et al (2017) Sleep disorders and allergic diseases in Chinese toddlers. Sleep Med 37:174–179. https://doi.org/10.1016/j.sleep.2017.02.011
Camfferman D, Kennedy JD, Gold M, Simpson C, Lushington K (2013) Sleep and neurocognitive functioning in children with eczema. Int J Psychophysiol 89:265–272. https://doi.org/10.1016/j.ijpsycho.2013.01.006
Zandieh SO, Cespedes A, Ciarleglio A, Bourgeois W, Rapoport DM, Bruzzese JM (2017) Asthma and subjective sleep disordered breathing in a large cohort of urban adolescents. J Asthma 54:62–68. https://doi.org/10.1080/02770903.2016.1188942
Tischer CG, Hohmann C, Thiering E et al (2011) Meta-analysis of mould and dampness exposure on asthma and allergy in eight European birth cohorts: an ENRIECO initiative. Allergy 66:1570–1579. https://doi.org/10.1111/j.1398-9995.2011.02712.x
Zhang J, Sun C, Liu W et al (2018) Associations of household renovation materials and periods with childhood asthma, in China: a retrospective cohort study. Environ Int 113:240–248. https://doi.org/10.1016/j.envint.2018.02.001
Norbäck D, Hashim JH, Hashim Z, Ali F (2017) Volatile organic compounds (VOC), formaldehyde and nitrogen dioxide (NO(2)) in schools in Johor Bahru, Malaysia: associations with rhinitis, ocular, throat and dermal symptoms, headache and fatigue. Sci Total Environ 592:153–160. https://doi.org/10.1016/j.scitotenv.2017.02.215
Naclerio R, Ansotegui IJ, Bousquet J et al (2020) International expert consensus on the management of allergic rhinitis (AR) aggravated by air pollutants: impact of air pollution on patients with AR: Current knowledge and future strategies. World Allergy Organ J 13:100106. https://doi.org/10.1016/j.waojou.2020.100106
Liu H, Chen S, Zhu H et al (2017) Correlation between preconception maternal non-occupational exposure to interior decoration or oil paint odour and average birth weight of neonates: findings from a nationwide cohort study in China’s rural areas. BMJ Open 7:e013700. https://doi.org/10.1136/bmjopen-2016-013700
Alford KL, Kumar N (2021) Pulmonary health effects of indoor volatile organic compounds-a meta-analysis. Int J Environ Res Public Health 18:1578. https://doi.org/10.3390/ijerph1804157
Li JS, Peat JK, Xuan W, Berry G (1999) Meta-analysis on the association between environmental tobacco smoke (ETS) exposure and the prevalence of lower respiratory tract infection in early childhood. Pediatr Pulmonol 27:5–13.
Strachan DP, Cook DG (1997) Health effects of passive smoking. 1. Parental smoking and lower respiratory illness in infancy and early childhood. Thorax 52:905–914. https://doi.org/10.1136/thx.52.10.905
Strachan DP, Cook DG (1998) Health effects of passive smoking .5. Parental smoking and allergic sensitisation in children. Thorax 53:117–123. https://doi.org/10.1136/thx.53.2.117
Thacher JD, Gehring U, Gruzieva O et al (2018) Maternal smoking during pregnancy and early childhood and development of asthma and rhinoconjunctivitis - a MeDALL project. Environ Health Perspect 126:047005. https://doi.org/10.1289/EHP2738
Acknowledgements
We would like to thank the fund of the Medical Innovation Team of Jiangsu Province and Wuxi Municipal Bureau on Science and Technology. We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This study was funded by the Medical Innovation Team of Jiangsu Province (Grant No. CXTDB 2017016). Wuxi Municipal Bureau on Science and Technology (Grant No. NZ2019026). The funding had support data collection, analysis, interpretation of the data, materials, labor service free, and the publication charges for this article. The funding did not include analysis tools.
Author information
Authors and Affiliations
Contributions
L.L. and J.Q. designed and led the research. Q.W. drafted the work and led the writing of the paper. Y.G. revised the paper. X.P.W. and Z.Z.P. analyzed the participants’ data. S.S.P., S.Y.X., and Q.Z. gathered and organized the data. All authors contributed to the implementation of the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was provided by the medical ethics committee of the Affiliated Wuxi Children’s Hospital of Nanjing Medical University (No. WXCH2016-11-002).
Consent to participate
Informed consent was obtained from the parents or guardians of all participants.
Consent for publication
The participant has consented to the submission of the article to the journal.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Q., Guo, Y., Wu, X. et al. Effect of allergic rhinitis on sleep in children and the risk factors of an indoor environment. Sleep Breath 26, 1265–1275 (2022). https://doi.org/10.1007/s11325-021-02546-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02546-2