Abstract
Purpose
This research aimed at determining the relationship between self-reported sleep duration during week-/work-days and metabolic syndrome (MetS) from NHANES 2013 to 2016.
Methods
This study analyzed data from 11,181 people aged 16 or older who took part in the NHANES (National Health and Nutrition Examination Surveys) from 2013 to 2016. A standard questionnaire was used to define self-reported sleep duration, and MetS was defined on the basis of the NCEP (National Cholesterol Education Program)/ATP III revised diagnostic criteria. Logistic regression and restricted cubic splines (RCS) models were used to assess the relationship between self-reported sleep duration and MetS.
Results
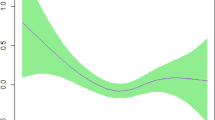
The overall prevalence of MetS in the study cohort was 26.1%, with 24.8% for males and 27.3% for females. After adjusting for potential confounding factors, MetS was significantly associated with self-reported short sleep duration (odds ratio = 1.16, 95% confidence interval = 1.03–1.31, P = 0.013) but not with long sleep duration (P = 0.117). RCS regression revealed that self-reported sleep duration was nonlinearly related to MetS (P for nonlinearity = 0.0026). The risk of MetS decreased with increased sleep duration for durations of less than 7 h/day, while there was no association for longer sleep durations.
Conclusion
These results suggest that self-reported short sleep duration is a risk factor for MetS, while long sleep duration is not.




Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F (2006) Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Curr Opin Cardiol 21(1):1–6. https://doi.org/10.1097/01.hco.0000200416.65370.a0
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr, International Diabetes Federation Task Force on E, Prevention, Hational Heart L, Blood I, American Heart A, World Heart F, International Atherosclerosis S, International Association for the Study of O (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645. https://doi.org/10.1161/CIRCULATIONAHA.109.192644
Borena W, Strohmaier S, Lukanova A, Bjorge T, Lindkvist B, Hallmans G, Edlinger M, Stocks T, Nagel G, Manjer J, Engeland A, Selmer R, Haggstrom C, Tretli S, Concin H, Jonsson H, Stattin P, Ulmer H (2012) Metabolic risk factors and primary liver cancer in a prospective study of 578,700 adults. Int J Cancer 131(1):193–200. https://doi.org/10.1002/ijc.26338
Ford ES (2005) Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care 28(7):1769–1778. https://doi.org/10.2337/diacare.28.7.1769
Esposito K, Giugliano D (2014) Healthy lifestyle for metabolic health: no more excuse! Endocrine 46(2):176–178. https://doi.org/10.1007/s12020-014-0165-6
Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, Miller MA (2008) Meta-analysis of short sleep duration and obesity in children and adults. Sleep 31(5):619–626. https://doi.org/10.1093/sleep/31.5.619
Feng X, Liu Q, Li Y, Zhao F, Chang H, Lyu J (2019) Longitudinal study of the relationship between sleep duration and hypertension in Chinese adult residents (CHNS 2004-2011). Sleep Med 58:88–92. https://doi.org/10.1016/j.sleep.2019.01.006
Wang J, Kwok MK, Au Yeung SL, Li AM, Lam HS, Leung JYY, Hui LL, Leung GM, Schooling CM (2019) Sleep duration and risk of diabetes: observational and Mendelian randomization studies. Prev Med 119:24–30. https://doi.org/10.1016/j.ypmed.2018.11.019
Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA (2011) Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J 32(12):1484–1492. https://doi.org/10.1093/eurheartj/ehr007
Ju SY, Choi WS (2013) Sleep duration and metabolic syndrome in adult populations: a meta-analysis of observational studies. Nutr Diabetes 3:e65. https://doi.org/10.1038/nutd.2013.8
Kim CE, Shin S, Lee HW, Lim J, Lee JK, Shin A, Kang D (2018) Association between sleep duration and metabolic syndrome: a cross-sectional study. BMC Public Health 18(1):720. https://doi.org/10.1186/s12889-018-5557-8
Hall MH, Muldoon MF, Jennings JR, Buysse DJ, Flory JD, Manuck SB (2008) Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep 31(5):635–643. https://doi.org/10.1093/sleep/31.5.635
Xi B, He D, Zhang M, Xue J, Zhou D (2014) Short sleep duration predicts risk of metabolic syndrome: a systematic review and meta-analysis. Sleep Med Rev 18(4):293–297. https://doi.org/10.1016/j.smrv.2013.06.001
Iftikhar IH, Donley MA, Mindel J, Pleister A, Soriano S, Magalang UJ (2015) Sleep duration and metabolic syndrome. An updated dose-risk metaanalysis. Ann Am Thorac Soc 12(9):1364–1372. https://doi.org/10.1513/AnnalsATS.201504-190OC
Deng HB, Tam T, Zee BC, Chung RY, Su X, Jin L, Chan TC, Chang LY, Yeoh EK, Lao XQ (2017) Short sleep duration increases metabolic impact in healthy adults: a population-based cohort study. Sleep 40 (10). https://doi.org/10.1093/sleep/zsx130
Borrud L, Chiappa MM, Burt VL, Gahche J, Zipf G, Johnson CL, Dohrmann SM (2014) National health and nutrition examination survey: national youth fitness survey plan, operations, and analysis, 2012. Vital and health statistics Series 2, Data evaluation and methods research (163):1–24
Desquilbet L, Mariotti F (2010) Dose-response analyses using restricted cubic spline functions in public health research. Stat Med 29(9):1037–1057. https://doi.org/10.1002/sim.3841
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D (2012) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175(1):66–73. https://doi.org/10.1093/aje/kwr265
Wu MC, Yang YC, Wu JS, Wang RH, Lu FH, Chang CJ (2012) Short sleep duration associated with a higher prevalence of metabolic syndrome in an apparently healthy population. Prev Med 55(4):305–309. https://doi.org/10.1016/j.ypmed.2012.07.013
Choi JK, Kim MY, Kim JK, Park JK, Oh SS, Koh SB, Eom A (2011) Association between short sleep duration and high incidence of metabolic syndrome in midlife women. Tohoku J Exp Med 225(3):187–193. https://doi.org/10.1620/tjem.225.187
Rodriguez A, Gomez-Ambrosi J, Catalan V, Gil MJ, Becerril S, Sainz N, Silva C, Salvador J, Colina I, Fruhbeck G (2009) Acylated and desacyl ghrelin stimulate lipid accumulation in human visceral adipocytes. Int J Obes 33(5):541–552. https://doi.org/10.1038/ijo.2009.40
Nogueiras R, Tschop MH, Zigman JM (2008) Central nervous system regulation of energy metabolism: ghrelin versus leptin. Ann N Y Acad Sci 1126:14–19. https://doi.org/10.1196/annals.1433.054
Bromley LE, Booth JN 3rd, Kilkus JM, Imperial JG, Penev PD (2012) Sleep restriction decreases the physical activity of adults at risk for type 2 diabetes. Sleep 35(7):977–984. https://doi.org/10.5665/sleep.1964
Oliveira RG, Guedes DP (2016) Physical activity, sedentary behavior, cardiorespiratory fitness and metabolic syndrome in adolescents: systematic review and meta-analysis of observational evidence. PLoS One 11(12):e0168503. https://doi.org/10.1371/journal.pone.0168503
Morselli L, Leproult R, Balbo M, Spiegel K (2010) Role of sleep duration in the regulation of glucose metabolism and appetite. Best Pract Res Clin Endocrinol Metab 24(5):687–702. https://doi.org/10.1016/j.beem.2010.07.005
Shan Z, Ma H, Xie M, Yan P, Guo Y, Bao W, Rong Y, Jackson CL, Hu FB, Liu L (2015) Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care 38(3):529–537. https://doi.org/10.2337/dc14-2073
Wang Y, Mei H, Jiang YR, Sun WQ, Song YJ, Liu SJ, Jiang F (2015) Relationship between Duration of sleep and hypertension in adults: a meta-analysis. J Clin Sleep Med : JCSM : Off Publ Am Acad Sleep Med 11(9):1047–1056. https://doi.org/10.5664/jcsm.5024
Gangwisch JE (2014) A review of evidence for the link between sleep duration and hypertension. Am J Hypertens 27(10):1235–1242. https://doi.org/10.1093/ajh/hpu071
Spiesshoefer J, Linz D, Skobel E, Arzt M, Stadler S, Schoebel C, Fietze I, Penzel T, Sinha AM, Fox H, Oldenburg O, On behalf of the German Cardiac Society Working Group On Sleep Disordered Breathing Ag-Deutsche Gesellschaft Fur Kardiologie Herz Und Kreislaufforschung EVO (2019) Sleep - the yet underappreciated player in cardiovascular diseases: a clinical review from the German Cardiac Society Working Group on Sleep Disordered Breathing. Eur J Prev Cardiol. https://doi.org/10.1177/2047487319879526
Funding
This study was supported by the National Social Science Foundation of China [No.16BGL183].
Author information
Authors and Affiliations
Contributions
XJ Feng: project development, data analysis, manuscript writing. WT Wu: data analysis, manuscript writing. FF Zhao: manuscript writing/editing. X Li: manuscript editing. DD Han: manuscript editing. CZ Li: data analysis. FS Xu: manuscript editing. J Lyu: project development, manuscript editing, data analysis.
Corresponding author
Ethics declarations
Research involving human participants and/or animals
The NHANES study protocol was approved by the National Center for Health Statistics ethics review board.
Informed consent
All participants in the NHANES provided written informed consent.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Feng, X., Wu, W., Zhao, F. et al. Relationship between self-reported sleep duration during week-/work-days and metabolic syndrome from NHANES 2013 to 2016. Sleep Breath 26, 1593–1601 (2022). https://doi.org/10.1007/s11325-021-02522-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02522-w