Abstract
Objectives
To compare the efficacy and success rates of lateral pharyngoplasty techniques (LP) vs. uvulopalatopharyngoplasty (UPPP) among adult patients surgically treated for obstructive sleep apnea.
Methods
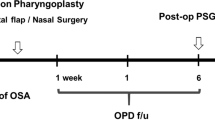
A systematic literature review of the last 20 years’ papers was conducted using PubMed/Medline, Embase, Web of Science, Scholar, and the Cochrane Library until April 2021. Only full-text English articles comparing LP and UPPP outcomes in adult patients with objective outcomes were included in the study.
Results
We included 9 articles for a total of 312 surgically treated patients with OSA. LP techniques for obstructive sleep apnea were used on 186 (60%) subjects, while 126 patients (40%) were treated with UPPP. Both surgical procedures resulted in significant improvements in apnea-hypopnea index (AHI), Epworth Sleepiness Scale (ESS) score, and lowest oxygen saturation (LOS) (p < 0.001 in all cases). Although better outcomes were reported with lateral pharyngoplasty, the differences were not significant compared to UPPP post-operative results (p > 0.05 in all cases).
Conclusions
UPPP and LP are both effective surgical procedures in treating OSA in adults. Although not significant, LPs demonstrated improved post-operative outcomes. However, further evidence comparing the surgical effect on patients with OSA is needed to discriminate post-operative outcomes.







Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Bilston LE, Gandevia SC (1985) Biomechanical properties of the human upper airway and their effect on its behavior during breathing and in obstructive sleep apnea. J Appl Physiol 116(3):314–324
Iannella G, Maniaci A, Magliulo G et al (2020) Current challenges in the diagnosis and treatment of obstructive sleep apnea syndrome in the elderly. Pol Arch Intern Med 130(7–8):649–654
Kushida CA, Littner MR, Hirshkowitz M et al (2006) American Academy of Sleep Medicine. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29(3):375–380. https://doi.org/10.1093/sleep/29.3.375
Li MX, Yan CY, Wang S (2015) New insights on the role of the insular cortex and habenula in OSA. Sleep Breath 19(4):1347–1353
Di Luca M, Iannella G, Montevecchi F et al (2020) Use of the transoral robotic surgery to treat patients with recurrent lingual tonsillitis. Int J Med Robot 16(4):e2106. https://doi.org/10.1002/rcs.2106
Pieters T, Collard P, Aubert G et al (1996) Acceptance and longterm compliance with nCPAP in patients with obstructive sleep apnoea syndrome. Eur Respir J 9:939–944
Ravesloot MJL, de Vries N, Stuck BA (2014) Treatment adherence should be taken into account when reporting treatment outcomes in obstructive sleep apnea. Laryngoscope 124:344–345
Vicini C, De Vito A, Benazzo M et al (2012) The nose oropharynx hypopharynx and larynx (NOHL) classification: a new system of diagnostic standardized examination for OSAHS patients. Eur Arch Otorhinolaryngol 269:1297–1300
De Vito A, Carrasco Llatas M, Vanni A et al (2014) European position paper on drug-induced sedation endoscopy (DISE). Sleep Breath 18:453–465
Fujita S, Conway W, Zorick F, Roth T (1981) Surgical correction of anatomic abnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 89(6):923–934
Golbin D, Musgrave B, Succar E, Yaremchuk K (2016) Clinical analysis of drug-induced sleep endoscopy for the OSA patient. Laryngoscope 126(1):249–253
Dickson RI, Blokmanis A (1987) Treatment of obstructive sleep apnea by uvulopalatopharyngoplasty. Laryngoscope 97:1054–1059
Tang JA, Salapatas AM, Bonzelaar LB, Friedman M (2017) Long-term incidence of velopharyngeal insufficiency and other sequelae following uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 156(4):606–610
Röösli C, Schneider S, Häusler R (2006) Long-term results and complications following uvulopalatopharyngoplasty in 116 consecutive patients. Eur Arch Otorhinolaryngol 263:754–758
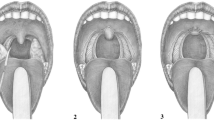
Cahali MB (2003) Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope 113:1961–1968
Pang KP, Woodson BT (2007) Expansion sphincter pharyngoplasty: a new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg 137:110–114
Hong S, Kim HG, Han S et al (2019) Indications for and outcomes of expansion sphincter pharyngoplasty to treat lateral pharyngeal collapse in patients with obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg 145(5):405–412
Pang KP, Pang EB, Win MT, Pang KA, Woodson BT (2016) Expansion sphincter pharyngoplasty for the treatment of OSA:a systemic review and meta-analysis. Eur Arch Otorhinolaryngol 273:2329–2333
Vicini C, Hendawy E, Campanini A, Eesa M, Bahgat A, AlGhamdi S et al (2015) Barbed reposition pharyngoplasty (BRP) for OSAHS: a feasibility, safety, efficacy and teachability pilot study. “We are on the giant’s shoulders.” Eur Arch Otorhinolaryngol 272(10):3065–70
Iannella G, Vallicelli B, Magliulo G et al (2020) Long-term subjective outcomes of barbed reposition pharyngoplasty for obstructive sleep apnea syndrome treatment. Int J Environ Res Public Health 17(5):1542. https://doi.org/10.3390/ijerph17051542
Montevecchi F, Meccariello G, Firinu E et al (2018) Prospective multicentre study on barbed reposition pharyngoplasty standing alone or as a part of multilevel surgery for sleep apnoea. Clin Otolaryngol 43:483–488
Gulotta G, Iannella G, Meccariello G et al (2021) Barbed suture extrusion and exposure in palatoplasty for OSA: what does it mean? Am J Otolaryngol 42(4):102994
Moher D, Shamseer L, Clarke M, PRISMA-P Group et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1):1. https://doi.org/10.1186/2046-4053-4-1
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536
Zhou Y, Dendukuri N (2014) Statistics for quantifying hetero-geneity in univariate and bivariate meta-analyses of binary data: the case of meta-analyses of diagnostic accuracy. Stat Med 33(16):27012717
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56:455e63. https://doi.org/10.1111/j.0006-341x.2000.00455.x
Cammaroto G, Montevecchi F, D’Agostino G, Zeccardo E, Bellini C, Meccariello G, Vicini C (2017) Palatal surgery in a transoral robotic setting (TORS): preliminary results of a retrospective comparison between uvulopalatopharyngoplasty (UPPP), expansion sphincter pharyngoplasty (ESP) and barbed repositioning pharyngoplasty (BRP). Acta Otorhinolaryngol Ital 37(5):406–409. https://doi.org/10.14639/0392-100X-1321
Rashwan MS, Montevecchi F, Cammaroto G et al (2018) Evolution of soft palate surgery techniques for obstructive sleep apnea patients: a comparative study for single-level palatal surgeries. Clin Otolaryngol 43:584–590
Carrasco-Llatas M, Marcano-Acuña M, Zerpa-Zerpa V, Dalmau-Galofre J (2015) Surgical results of different palate techniques to treat oropharyngeal collapse. Eur Arch Otorhinolaryngol 272:2535–2540
Vicini C, Montevecchi F, Pang K, Bahgat A, Dallan I, Frassineti S, Campanini A (2013) Combined transoral robotic tongue base surgery and palate surgery in obstructive sleep apnea-hypopnea syndrome: expansion sphincter pharyngoplasty versus uvulopalatopharyngoplasty. Head Neck 36(1):77–83
Dizdar D, Civelek Ş, Çaliş ZA, Dizdar SK, Coşkun BU, Vural A (2015) Comparative analysis of lateral pharyngoplasty and uvulopalatopharyngoplasty techniques with polisomnography and Epworth sleepiness scales. J Craniofac Surg 26(7):e647–e651. https://doi.org/10.1097/SCS.0000000000001979
Steinbichler TB, Bender B, Giotakis AI, Dejaco D, Url C, Riechelmann H (2018) Comparison of two surgical suture techniques in uvulopalatopharyngoplasty and expansion sphincter pharyngoplasty. Eur Arch Otorhinolaryngol 275(2):623–628
Chi JC, Chiang RP, Chou TY, Shu CH, Shiao AS, Lin CM (2015) The role of lateral pharyngoplasty in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 272(2):489–496. https://doi.org/10.1007/s00405-014-3253-6
Rashwan MS, Montevecchi F, Firinua E et al (2018) Let’s know from our patients: PPOPS score for palate surgery evaluation/a pilot study. Eur Arch Otorhinolaryngol 275(1):287–291. https://doi.org/10.1007/s00405-017-4795-1
Cahali MB, Formigoni GG, Gebrim EM, Miziara ID (2004) Lateral pharyngoplasty versus uvulopalatopharyngoplasty: a clinical, polysomnographic and computed tomography measurement comparison. Sleep 27:942–950
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Redline S (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. J Clin Sleep Med 8:597–619
Maniaci A, Iannella G, Cocuzza S et al (2021) Oxidative stress and inflammation biomarker expression in obstructive sleep apnea patients. J Clin Med 10(2):277. https://doi.org/10.3390/jcm10020277
Iannella G, Magliulo G, Maniaci A et al (2021) Olfactory function in patients with obstructive sleep apnea: a meta-analysis study. Eur Arch Otorhinolaryngol 278(3):883–891. https://doi.org/10.1007/s00405-020-06316-w
Young T, Finn L, Peppard PE et al (2008) Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 31:1071–1078
Pace A, Iannella G, Rossetti V et al (2020) Diagnosis of obstructive sleep apnea in patients with allergic and non-allergic rhinitis. Medicina (Kaunas) 56(9):454. https://doi.org/10.3390/medicina56090454
Hewitt RJD, Dasgupta A, Singh A, Dutta C, Kotecha BT (2009) Is sleep nasendoscopy a valuable adjunct to clinical examination in the evaluation of upper airway obstruction? Eur Arch Otorhinolaryngol 266:691–697
Eichler C, Sommer JU, Stuck BA, Hörmann K, Maurer JT (2013) Does drug-induced sleep endoscopy change the treatment concept of patients with snoring and obstructive sleep apnea? Sleep Breath 17:63–68
Fernández-Julián E, García-Pérez M, García-Callejo J, Ferrer F, Martí F, Marco J (2014) Surgical planning after sleep versus awake techniques in patients with obstructive sleep apnea. Laryngoscope 124(8):1970–1974
Zerpa Zerpa V, Carrasco Llatas M, Agostini Porras G, Dalmau Galofre J (2015) Drug-induced sedation endoscopy versus clinical exploration for the diagnosis of severe upper airway obstruction in OSAHS patients. Sleep Breath 19(4):1367–1372
Iannella G, Magliulo G, di Luca M et al (2020) Lateral pharyngoplasty techniques for obstructive sleep apnea syndrome: a comparative experimental stress test of two different techniques. Eur Arch Otorhinolaryngol 277:1793–1800
Grillo C, La Mantia I, Zappala G, Cocuzza S, Ciprandi G, Andaloro C (2019) Oral health in children with sleep-disordered breathing: a cross-sectional study. Acta Biomed 90(7-S):52–59. https://doi.org/10.23750/abm.v90i7-S.8661
Värendh M, Berg S, Andersson M (2012) Long-term follow-up of patients operated with uvulopalatopharyngoplasty from 1985 to 1991. Respir Med 106:1788–1793
Goh YH, Mark I, Fee WE Jr (2007) Quality of life 17 to 20 years after uvulopalatopharyngoplasty. Laryngoscope 117:503–506
Haavisto L, Suonpaa J (1994) Complications of uvulopalatopharyngoplasty. Clin Otolaryngol Allied Sci 19:243–247
Tang JA, Salapatas AM, Bonzelaar LB, Friedman M (2017) Long-term incidence of velopharyngeal insufficiency and other sequelae following uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 156(4):606–610. https://doi.org/10.1177/0194599816688646
Modica DM, Lorusso F, Presti G, Fasola S, Gallina S (2019) Our assessment using palate postoperative problems score (PPOPS): tool for the evaluation of results in palatal surgery techniques. Indian J Otolaryngol Head Neck Surg 71(Suppl 1):766–770. https://doi.org/10.1007/s12070-018-1540-z
Acknowledgements
We thank Professor Antony Bridgewood for the significant guidance provided during the drafting of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All authors give consent to the publication.
Conflict of interest
The author declares no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maniaci, A., Di Luca, M., Lechien, J.R. et al. Lateral pharyngoplasty vs. traditional uvulopalatopharyngoplasty for patients with OSA: systematic review and meta-analysis. Sleep Breath 26, 1539–1550 (2022). https://doi.org/10.1007/s11325-021-02520-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02520-y