Abstract
Objective
To investigate the relationship between secondhand smoke (SHS) exposure and sleep quality in never-smokers of Northwest China.
Methods
Never-smoking adults (≥ 15 years) from Xinjiang, Northwest China, were included in this cross-sectional survey between April and October 2019. SHS exposure in never-smokers was estimated using a structured questionnaire. Sleep quality was evaluated by Pittsburgh Sleep Quality Index (PSQI), with PSQI score > 5 classified as poor sleep quality. Association of SHS exposure and frequency and duration of SHS exposure with poor sleep quality were analyzed by using a multivariate logistic regression after adjusting for potential confounding factors, including stratification by sex.
Results
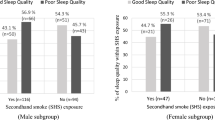
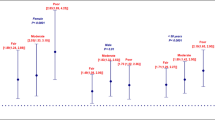
The mean age of participants was 48.0 years, and 77% were females. Of 21,198 never-smokers, 13% (n = 2703) reported SHS exposure and 35% (n = 7390) reported poor sleep quality. In multivariate logistic regression analysis, a significant association was observed between SHS exposure and poor sleep quality (adjusted odds ratio (OR), 1.36; 95% confidence interval (CI) 1.24–1.48). Subgroup analysis showed a negative association of SHS exposure with sleep quality in both sexes. However, a significant dose–response relationship of frequency and duration of SHS exposure per week with poor sleep quality was observed only in females. Consistent results were also observed in the aged ≥ 18 years.
Conclusion
Exposure to SHS is associated with poor sleep quality in never-smoking adults of Northwest China. A dose–response relationship between SHS exposure and poor sleep quality is found in women. Avoiding SHS exposure may have beneficial effects on sleep quality, especially for females.


Similar content being viewed by others
Availability of data and material
Materials included in the manuscript, excluding the relevant raw data, will be made freely available to any researchers who wish to use them for noncommercial purposes while preserving any necessary confidentiality and anonymity.
Code availability
Not applicable.
References
Tribl GG, Schmeiser-Rieder A, Rosenberger A, Saletu B, Bolitschek J, Kapfhammer G, Katschnig H, Holzinger B, Popovic R, Kunze M, Zeitlhofer J (2002) Sleeping habits in the Austrian population. Sleep Med 3(1):21–28. https://doi.org/10.1016/s1389-9457(01)00117-4
Hinz A, Glaesmer H, Brähler E, Löffler M, Engel C, Enzenbach C, Hegerl U, Sander C (2017) Sleep quality in the general population: psychometric properties of the Pittsburgh Sleep Quality Index, derived from a German community sample of 9284 people. Sleep Med 30:57–63. https://doi.org/10.1016/j.sleep.2016.03.008
Fatima Y, Doi SA, Najman JM, Mamun AA (2016) Exploring gender difference in sleep quality of young adults: findings from a large population study. Clin Med Res 14(3–4):138–144. https://doi.org/10.3121/cmr.2016.1338
Wang Y, Li Y, Liu X, Liu R, Mao Z, Tu R, Zhang H, Zhang X, Qian X, Jiang J, Qiao D, Luo Z, Dong X, Liu X, Wang C (2019) Gender-specific prevalence of poor sleep quality and related factors in a Chinese rural population: the Henan Rural Cohort Study. Sleep Med 54:134–141. https://doi.org/10.1016/j.sleep.2018.10.031
Bayon V, Leger D, Gomez-Merino D, Vecchierini MF, Chennaoui M (2014) Sleep debt and obesity. Ann Med 46(5):264–272. https://doi.org/10.3109/07853890.2014.931103
Kim BJ, Kang JG, Kim JH, Seo DC, Sung KC, Kim BS, Kang JH (2019) Association between secondhand smoke exposure and hypertension in 106,268 Korean self-reported never-smokers verified by cotinine. J Clin Med 8(8):1238. https://doi.org/10.3390/jcm8081238 (Published 2019 Aug 16)
Lu K, Chen J, Wang L, Wang C, Ding R, Wu S, Hu D (2017) Association of sleep duration, sleep quality and shift-work schedule in relation to hypertension prevalence in Chinese adult males: a cross-sectional survey. Int J Environ Res Public Health 14(2):210. https://doi.org/10.3390/ijerph14020210 (Published 2017 Feb 21)
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA (2010) Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 33(2):414–420. https://doi.org/10.2337/dc09-1124
Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA (2011) Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J 32(12):1484–1492. https://doi.org/10.1093/eurheartj/ehr007
Sharma M, Sawhney JP, Panda S (2014) Sleep quality and duration - potentially modifiable risk factors for coronary artery disease? Indian Heart J 66(6):565–568. https://doi.org/10.1016/j.ihj.2014.10.412
Blask DE (2009) Melatonin, sleep disturbance and cancer risk. Sleep Med Rev 13(4):257–264. https://doi.org/10.1016/j.smrv.2008.07.007
Cheng W, Rolls ET, Ruan H, Feng J (2018) Functional connectivities in the brain that mediate the association between depressive problems and sleep quality. JAMA Psychiat 75(10):1052–1061. https://doi.org/10.1001/jamapsychiatry.2018.1941
Malhotra RK (2018) Neurodegenerative disorders and sleep. Sleep Med Clin 13(1):63–70. https://doi.org/10.1016/j.jsmc.2017.09.006
Sindi S, Kåreholt I, Johansson L, Skoog J, Sjöberg L, Wang HX, Johansson B, Fratiglioni L, Soininen H, Solomon A, Skoog I, Kivipelto M (2018) Sleep disturbances and dementia risk: a multicenter study. Alzheimers Dement 14(10):1235–1242. https://doi.org/10.1016/j.jalz.2018.05.012
de Mello MT, Narciso FV, Tufik S, Paiva T, Spence DW, Bahammam AS, Verster JC, Pandi-Perumal SR (2013) Sleep disorders as a cause of motor vehicle collisions. Int J Prev Med 4(3):246–257
Halperin D (2014) Environmental noise and sleep disturbances: a threat to health? Sleep Sci 7(4):209–212. https://doi.org/10.1016/j.slsci.2014.11.003
Lund HG, Reider BD, Whiting AB, Prichard JR (2010) Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health 46(2):124–132. https://doi.org/10.1016/j.jadohealth.2009.06.016
Soldatos CR, Kales JD, Scharf MB, Bixler EO, Kales A (1980) Cigarette smoking associated with sleep difficulty. Science 207(4430):551–553. https://doi.org/10.1126/science.7352268
McNamara JP, Wang J, Holiday DB, Warren JY, Paradoa M, Balkhi AM, Fernandez-Baca J, McCrae CS (2014) Sleep disturbances associated with cigarette smoking. Psychol Health Med 19(4):410–419. https://doi.org/10.1080/13548506.2013.832782
Jaehne A, Loessl B, Bárkai Z, Riemann D, Hornyak M (2009) Effects of nicotine on sleep during consumption, withdrawal and replacement therapy. Sleep Med Rev 13(5):363–377. https://doi.org/10.1016/j.smrv.2008.12.003
Saint-Mleux B, Eggermann E, Bisetti A, Bayer L, Machard D, Jones BE, Mühlethaler M, Serafin M (2004) Nicotinic enhancement of the noradrenergic inhibition of sleep-promoting neurons in the ventrolateral preoptic area. J Neurosci 24(1):63–67. https://doi.org/10.1523/JNEUROSCI.0232-03.2004
Morin CM, LeBlanc M, Bélanger L, Ivers H, Merette C, Savard J (2011) Prevalence of insomnia and its treatment in Canada. Can J Psychiatry. 56(9):540–548
Jacobs M, Alonso AM, Sherin KM, Koh Y, Dhamija A, Lowe AL, Prevention Practice Committee ACPM (2013) Policies to restrict secondhand smoke exposure: American College of Preventive Medicine Position Statement. Am J Prev Med 45(3):360–367. https://doi.org/10.1016/j.amepre.2013.05.007
Iversen B, Jacobsen BK, Løchen ML (2013) Active and passive smoking and the risk of myocardial infarction in 24,968 men and women during 11 year of follow-up: the Tromsø Study. Eur J Epidemiol 28(8):659–667. https://doi.org/10.1007/s10654-013-9785-z
Ballbè M, Martínez-Sánchez JM, Gual A, Martínez C, Fu M, Sureda X, Padrón-Monedero A, Galán I, Fernández E (2015) Association of second-hand smoke exposure at home with psychological distress in the Spanish adult population. Addict Behav 50:84–88. https://doi.org/10.1016/j.addbeh.2015.06.020
Zeng YN, Li YM (2016) Secondhand smoke exposure and mental health in adults: a meta-analysis of cross-sectional studies. Soc Psychiatry Psychiatr Epidemiol 51(9):1339–1348. https://doi.org/10.1007/s00127-015-1164-5
Yolton K, Xu Y, Khoury J, Succop P, Lanphear B, Beebe DW, Owens J (2010) Associations between secondhand smoke exposure and sleep patterns in children. Pediatrics 125(2):e261–e268. https://doi.org/10.1542/peds.2009-0690
Morioka H, Jike M, Kanda H, Osaki Y, Nakagome S, Otsuka Y, Kaneita Y, Itani O, Higuchi S, Ohida T (2018) The association between sleep disturbance and second-hand smoke exposure: a large-scale, nationwide, cross-sectional study of adolescents in Japan. Sleep Med 50:29–35. https://doi.org/10.1016/j.sleep.2018.04.014
Ohida T, Kaneita Y, Osaki Y, Harano S, Tanihata T, Takemura S, Wada K, Kanda H, Hayashi K, Uchiyama M (2007) Is passive smoking associated with sleep disturbance among pregnant women? Sleep 30(9):1155–1161. https://doi.org/10.1093/sleep/30.9.1155
Boakye D, Wyse CA, Morales-Celis CA, Biello SM, Bailey MES, Dare S, Ward J, Gill JMR, Pell JP, Mackay DF (2018) Tobacco exposure and sleep disturbance in 498 208 UK Biobank participants. J Public Health (Oxf) 40(3):517–526. https://doi.org/10.1093/pubmed/fdx102
Davila EP, Lee DJ, Fleming LE, LeBlanc WG, Arheart K, Dietz N, Lewis JE, McCollister K, Caban-Martinez A, Bandiera F (2010) Sleep disorders and secondhand smoke exposure in the U.S. population. Nicotine Tob Res 12(3):294–299. https://doi.org/10.1093/ntr/ntp193
Safa F, Chaiton M, Mahmud I, Ahmed S, Chu A (2020) The association between exposure to second-hand smoke and sleep disturbances: a systematic review and meta-analysis. Sleep Health 6(5):702–714
Wang P, Song L, Wang K, Han X, Cong L, Wang Y, Zhang L, Yan Z, Tang S, Du Y (2020) Prevalence and associated factors of poor sleep quality among Chinese older adults living in a rural area: a population-based study. Aging Clin Exp Res 32(1):125–131. https://doi.org/10.1007/s40520-019-01171-0
Cai H, Shu XO, Xiang YB, Yang G, Li H, Ji BT, Gao J, Gao YT, Zheng W (2015) Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women. Sleep 38(4):529–536. https://doi.org/10.5665/sleep.4564 (Published 2015 Apr 1)
Tsai PS, Wang SY, Wang MY, Su CT, Yang TT, Huang CJ, Fang SC (2005) Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res 14(8):1943–1952. https://doi.org/10.1007/s11136-005-4346-x
Global Recommendations on Physical Activity for Health. Geneva: World Health Organization; 2010
Zung WW (1965) A Self-Rating Depression Scale. Arch Gen Psychiatry 12:63–70. https://doi.org/10.1001/archpsyc.1965.01720310065008
Jegede RO (1976) Psychometric properties of the self-rating depression scale (SDS). J Psychol 93((1st Half)):27–30
Wang CF, Cai ZH, Xu Q (2009) Evaluation analysis of self-rating disorder scale in 1,340 people. Chin J Nervous Mental Dis 12:267–268
Gabrys JB, Peters K (1985) Reliability, discriminant and predictive validity of the Zung self-rating depression scale. Psychol Rep 57(3 Pt 2):1091–1096
eronda AC, Irish LA, Delahanty DL (2020) Effect of smoke exposure on young adults’ sleep quality. Nurs Health Sci 22(1):57–63. https://doi.org/10.1111/nhs.12644
Jaehne A, Unbehaun T, Feige B, Lutz UC, Batra A, Riemann D (2012) How smoking affects sleep: a polysomnographical analysis. Sleep Med 13(10):1286–1292. https://doi.org/10.1016/j.sleep.2012.06.026
Balfour DJ (1994) Neural mechanisms underlying nicotine dependence. Addiction 89(11):1419–1423. https://doi.org/10.1111/j.1360-0443.1994.tb03738.x
Franklin KA, Gíslason T, Omenaas E, Jõgi R, Jensen EJ, Lindberg E, Gunnbjörnsdóttir M, Nyström L, Laerum BN, Björnsson E, Torén K, Janson C (2004) The influence of active and passive smoking on habitual snoring. Am J Respir Crit Care Med 170(7):799–803. https://doi.org/10.1164/rccm.200404-474OC
Mong JA, Cusmano DM (2016) Sex differences in sleep: impact of biological sex and sex steroids. Philos Trans R Soc Lond B Biol Sci 371(1688):20150110. https://doi.org/10.1098/rstb.2015.0110
Mong JA, Baker FC, Mahoney MM, Paul KN, Schwartz MD, Semba K, Silver R (2011) Sleep, rhythms, and the endocrine brain: influence of sex and gonadal hormones. J Neurosci 31(45):16107–16116. https://doi.org/10.1523/JNEUROSCI.4175-11.2011
Terry PD, Rohan TE (2002) Cigarette smoking and the risk of breast cancer in women: a review of the literature. Cancer Epidemiol Biomarkers Prev 11(10 Pt 1):953–971
Fu M, Fernandez E, Martínez-Sánchez JM, Pascual JA, Schiaffino A, Agudo A, Ariza C, Borràs JM, Samet JM, DCOT Study investigators (2009) Salivary cotinine concentrations in daily smokers in Barcelona, Spain: a cross-sectional study. BMC Public Health 9:320. https://doi.org/10.1186/1471-2458-9-320 (Published 2009 Sep 3)
Lo K, Woo B, Wong M, Tam W (2018) Subjective sleep quality, blood pressure, and hypertension: a meta-analysis. J Clin Hypertens (Greenwich) 20:592–605
Kim K, Uchiyama M, Okawa M, Liu X, Ogihara R (2000) An epidemiological study of insomnia among the Japanese general population. Sleep 23(1):41–47
Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A (2016) The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non- clinical samples: a systematic review and meta-analysis. Sleep Med Rev 25:52–73
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Acknowledgements
We thank all the individuals who participated in the present study. We thank the Ministry of Science and Technology of the People’s Republic of China and the Department of Science and Technology of Xinjiang Uygur Autonomous Region of China for funding the project.
Funding
This work was supported by a grant from the national key research and development plan projects (2018YFC1311503) and the Department of Science and Technology of Xinjiang Uygur Autonomous Region of China (2017B03015).
Author information
Authors and Affiliations
Contributions
NL, LW, and MH was involved in the study design. NL, LW, MH, ML, ZY, ZW, RA, WY, and LY participated in the data collection. LW and MH designed the survey and performed the statistical analysis. LW drafted the manuscript. MH critically revised the manuscript. NL, ML, ZY, ZW, RA, WY, and LY gave important suggestions and did significant changes. All authors reviewed and approved the final version of the paper.
Corresponding author
Ethics declarations
Ethics approval
Ethics approval was obtained from the Ethics Review Committee of People’s Hospital of Xinjiang Uygur Autonomous Region.
Consent to participate
All subjects signed the informed consent.
Consent for publication
All authors agree with the publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Comment
The authors are commended for undertaking a study on the effects of second hand smoking in a population that includes adolescents through adults over 60 years and more importantly, that the study was undertaken on a population living in a less developed region where there is generally poor health awareness. Such populations are often ignored in health research. The outcomes identified that in women there was a dose response relationship between exposure to second hand smoke and poor sleep quality for those who were exposed but never smoked. The results highlight the important need for equity for all through education on improving health awareness about smoking cessation. a
Margot Skinner
Dunedin, New Zealand
Lin Wang and Mulalibieke Heizhati contributed equally to this work and are the co-first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, L., Heizhati, M., Li, M. et al. Secondhand smoke is associated with poor sleep quality in self-reported never-smokers of Northwest China: a cross-sectional study. Sleep Breath 26, 1417–1426 (2022). https://doi.org/10.1007/s11325-021-02505-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02505-x