Abstract
Study objectives
This analysis determined the association between obstructive sleep apnea (OSA) with hypopneas defined by a 3% O2 desaturation or arousal (3%A), but not by a hypopnea criterion of ≥ 4% (4%), and subjective sleepiness.
Methods
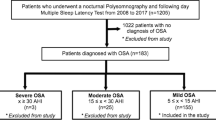
Data were analyzed from Sleep Heart Health Study participants who had polysomnography (N = 6307) regarding OSA and subjective sleepiness scores (Epworth Sleepiness Scale, ESS). The apnea hypopnea index (AHI) was classified based on 3% only, 3%A only, and 4% definitions of hypopneas.
Results
Of the 3326 participants without 4% OSA, 67.6% (n = 2247) had 3%A only OSA. The ESS score was higher in 3%A only OSA than in those without OSA (7.44 ± 4.2 vs 7.07 ± 4.3, P = 0.02). Of those without 4% OSA, 40.2% (n = 1336) had 3% only OSA. The ESS score was higher in those with 3% only OSA than those with no OSA (7.72 ± 4.3 vs 7.05 ± 4.2, P < 0.001). A linear regression model demonstrated a trend towards significance for the 3%A only AHI as an independent predictor of ESS when controlled for age, BMI, and sex (P = 0.051). The association of 3% only AHI with the ESS was stronger (P = 0.003). However, 23.3% of the participants with hypersomnia would not qualify as having OSA if arousals were excluded from the definition of OSA.
Conclusion
The current study found that the presence and severity of OSA is associated with higher ESS scores in persons with 3%A only OSA. Hence, the use of the 4% hypopnea definition will result in the failure to identify and treat a significant number of individuals with OSA who have subjective sleepiness.

Similar content being viewed by others
References
Berry RB, Budhiraja R, Gottlieb DJ et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8(5):597–619. https://doi.org/10.5664/jcsm.2172
Budhiraja R, Javaheri S, Parthasarathy S, Berry RB, Quan SF (2019) The association between obstructive sleep apnea characterized by a minimum 3 percent oxygen desaturation or arousal hypopnea definition and hypertension. J Clin Sleep Med 15(9):1261–1270. https://doi.org/10.5664/jcsm.7916
Quan SF, Budhiraja R, Javaheri S, Parthasarathy S, Berry RB (2020) The association between obstructive sleep apnea defined by 3 percent oxygen desaturation or arousal definition and self-reported cardiovascular disease in the Sleep Heart Health Study. Southwest J Pulm Crit Care 21(4):86–103. https://doi.org/10.13175/swjpcc054-20
Budhiraja R, Javaheri S, Parthasarathy S, Berry RB, Quan SF (2020) Incidence of hypertension in obstructive sleep apnea using hypopneas defined by 3 percent oxygen desaturation or arousal but not by only 4 percent oxygen desaturation. J Clin Sleep Med 16(10):1753–1760. https://doi.org/10.5664/jcsm.8684
Quan SF, Howard BV, Iber C et al (1997) The Sleep Heart Health Study: design, rationale, and methods. Sleep 20(12):1077–1085
Redline S, Sanders MH, Lind BK et al (1998) Methods for obtaining and analyzing unattended polysomnography data for a multicenter study. Sleep Heart Health Research Group. Sleep 21(7):759–767
Whitney CW, Gottlieb DJ, Redline S et al (1998) Reliability of scoring respiratory disturbance indices and sleep staging. Sleep 21(7):749–757
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, technique and scoring system for sleep stages of human sleep. Brain Information Service, Los Angeles
Redline S, Kapur VK, Sanders MH et al (2000) Effects of varying approaches for identifying respiratory disturbances on sleep apnea assessment. Am J Respir Crit Care Med 161(2 Pt 1):369–374. https://doi.org/10.1164/ajrccm.161.2.9904031
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Budhiraja R, Kushida CA, Nichols DA et al (2017) Predictors of sleepiness in obstructive sleep apnoea at baseline and after 6 months of continuous positive airway pressure therapy. Eur Respir J 50(5):1700348. https://doi.org/10.1183/13993003.00348-2017
Brink-Kjaer A, Olesen AN, Peppard PE et al (2020) Automatic detection of cortical arousals in sleep and their contribution to daytime sleepiness. Clin Neurophysiol 131(6):1187–1203. https://doi.org/10.1016/j.clinph.2020.02.027
Bonnet MH, Doghramji K, Roehrs T et al (2007) The scoring of arousal in sleep: reliability, validity, and alternatives. J Clin Sleep Med 3(2):133–145
Wimms AJ, Kelly JL, Turnbull CD et al (2020) Continuous positive airway pressure versus standard care for the treatment of people with mild obstructive sleep apnoea (MERGE): a multicentre, randomised controlled trial. Lancet Respir Med 8(4):349–358. https://doi.org/10.1016/S2213-2600(19)30402-3
Fong SY, Ho CK, Wing YK (2005) Comparing MSLT and ESS in the measurement of excessive daytime sleepiness in obstructive sleep apnoea syndrome. J Psychosom Res 58(1):55–60. https://doi.org/10.1016/j.jpsychores.2004.05.004
Acknowledgements
The Sleep Heart Health Study was supported by National Heart, Lung and Blood Institute cooperative agreements U01HL53940 (University of Washington), U01HL53941 (Boston University), U01HL53938 (University of Arizona), U01HL53916 (University of California, Davis), U01HL53934 (University of Minnesota), U01HL53931 (New York University), U01HL53937 and U01HL64360 (Johns Hopkins University), U01HL63463 (Case Western Reserve University), and U01HL63429 (Missouri Breaks Research). A list of SHHS investigators, staff and their participating institutions is available on the SHHS website, http://jhuccs1.us/shhs/details/investigators.htm.
Author information
Authors and Affiliations
Contributions
All authors have read and approve this manuscript.
Corresponding author
Ethics declarations
Informed consent
SHHS was approved by the respective institutional review boards for human subjects research at each site, and informed written consent was obtained from all subjects at the time of their enrollment into each stage of the study.
Research involving human participants and/or animals
The current study involved analysis of publicly available data from Sleep Heart Health Study (SHHS). All procedures performed in SHHS were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
Dr. Budhiraja reports no conflicts of interest or grant funding. Dr. Quan reports research funding from the National Institutes of Health, serves as a consultant to Jazz Pharmaceuticals and Whispersom, and is a committee chair and hypopnea taskforce member for the American Academy of Sleep Medicine.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Budhiraja, R., Quan, S.F. Sleepiness in obstructive sleep apnea using hypopneas defined by a 3% oxygen desaturation or arousal but not by 4% or greater oxygen desaturation. Sleep Breath 26, 1135–1139 (2022). https://doi.org/10.1007/s11325-021-02494-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02494-x