Abstract
Purpose
The identification of subgroups of obstructive sleep apnea (OSA) is critical to understand disease outcome and treatment response and ultimately develop optimal care strategies customized for each subgroup. In this sense, we aimed to perform a cluster analysis to identify subgroups of individuals with OSA based on clinical parameters in the Epidemiological Sleep Study of São Paulo city (EPISONO). We aimed to analyze whether or not subgroups remain after 8 years, since there is not any evidence showing if these subtypes of clinical presentation of OSA in the same population can change overtime.
Methods
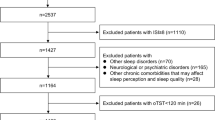
We used data derived from EPISONO cohort, which was followed over 8 years after baseline evaluation. All individuals underwent polysomnography, answered questionnaires, and had their blood collected for biochemical examinations. OSA was defined according to AHI ≥ 15 events/h. Cluster analysis was performed using latent class analysis (LCA).
Results
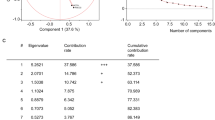
Of the 1042 individuals in the EPISONO cohort, 68% agreed to participate in the follow-up study (n = 712), and 704 were included in the analysis. We were able to replicate the OSA 3-cluster solution observed in previous studies: disturbed sleep, minimally symptomatic and excessively sleepy in both baseline (36%, 45% and 19%, respectively) and follow-up studies (42%, 43%, and 15%, respectively). The optimal cluster solution for our sample based on Bayesian information criterion (BIC) was 2 cluster for baseline (disturbed sleep and excessively sleepy) and 3 clusters for follow-up (disturbed sleep, minimally symptomatic, and excessively sleepy). A total of 45% of the participants migrated clusters between the two evaluations (and the factor associated with this was a greater delta-AHI (B = − 0.033, df = 1, p = 0.003).
Conclusions
The results replicate and confirm previously identified clinical clusters in OSA which remain in the longitudinal analysis, with some percentage of migration between clusters.
Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Tufik S, Santos-Silva R, Taddei JA, Bittencourt LR (2010) Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med 11(5):441–446. https://doi.org/10.1016/j.sleep.2009.10.005
Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N et al (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3(4):310–318. https://doi.org/10.1016/S2213-2600(15)00043-0
Darien, IL (2014) American Academy of Sleep Medicine. In: International Classification of Sleep Disorders, 3rd (edn).
Rapoport DM (2016) POINT: is the Apnea-Hypopnea Index the best way to quantify the severity of sleep-disordered breathing? Yes Chest 149(1):14–16. https://doi.org/10.1378/chest.15-1319
Zinchuk A, Yaggi HK (2019) Phenotypic subtypes of OSA: a challenge and opportunity for precision medicine. Chest. https://doi.org/10.1016/j.chest.2019.09.002
Ye L, Pien GW, Ratcliffe SJ, Björnsdottir E, Arnardottir ES, Pack AI et al (2014) The different clinical faces of obstructive sleep apnoea: a cluster analysis. Eur Respir J 44(6):1600–1607. https://doi.org/10.1183/09031936.00032314
Kim J, Keenan BT, Lim DC, Lee SK, Pack AI, Shin C (2018) Symptom-based subgroups of Koreans with obstructive sleep apnea. J Clin Sleep Med 14(3):437–443. https://doi.org/10.5664/jcsm.6994
Keenan BT, Kim J, Singh B, Bittencourt L, Chen NH, Cistulli PA et al (2018) Recognizable clinical subtypes of obstructive sleep apnea across international sleep centers: a cluster analysis. Sleep 41(3). https://doi.org/10.1093/sleep/zsx214
Pien GW, Ye L, Keenan BT, Maislin G, Björnsdóttir E, Arnardottir ES et al (2018) Changing faces of obstructive sleep apnea: treatment effects by cluster designation in the Icelandic Sleep Apnea Cohort. Sleep 41(3). https://doi.org/10.1093/sleep/zsx201
Mazzotti DR, Keenan BT, Lim DC, Gottlieb DJ, Kim J, Pack AI (2019) Symptom subtypes of obstructive sleep apnea predict incidence of cardiovascular outcomes. Am J Respir Crit Care Med 200(4):493–506. https://doi.org/10.1164/rccm.201808-1509OC
Santos-Silva R, Tufik S, Conway SG, Taddei JA, Bittencourt LR (2009) Sao Paulo Epidemiologic Sleep Study: rationale, design, sampling, and procedures. Sleep Med 10(6):679–685. https://doi.org/10.1016/j.sleep.2008.11.001
Associação Brasileira de Empresas de Pesquisa – ABEP. (2003) Critério de Classificação Econômica Brasil (CCEB)
Buysse DJ, Reynolds CF, Monk TH, Hoch CC, Yeager AL, Kupfer DJ (1991) Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI). Sleep 14(4):331–338
Pires ML, Benedito-Silva AA, Mello MT, Pompeia SG, Tufik S (2007) Sleep habits and complaints of adults in the city of São Paulo, Brazil, in 1987 and 1995. Braz J Med Biol Res 40(11):1505–1515
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Bertolazi AN, Fagondes SC, Hoff LS, Pedro VD, Menna Barreto SS, Johns MW (2009) Portuguese-language version of the Epworth sleepiness scale: validation for use in Brazil. J Bras Pneumol 35(9):877–883
Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP (1999) Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 131(7):485–491. https://doi.org/10.7326/0003-4819-131-7-199910050-00002
Cunha, J.A. (2001). Manual da versão em português da Escala Beck. São Paulo, Casa do Psicólogo
American Diabetes Association (2010) Diagnosis and classification of diabetes mellitus. Diabetes Care 33(Suppl 1):S62–S69. https://doi.org/10.2337/dc10-S062
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA et al (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645. https://doi.org/10.1161/CIRCULATIONAHA.109.192644
World Health Organization (2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1-253.
Hara K, Matsushita Y, Horikoshi M, Yoshiike N, Yokoyama T, Tanaka H et al (2006) A proposal for the cutoff point of waist circumference for the diagnosis of metabolic syndrome in the Japanese population. Diabetes Care 29(5):1123–1124. https://doi.org/10.2337/diacare.2951123
Rechtschaffen A (1968) A manual for standardized terminology, techniques and scoring system for sleep stages in human subjects. Brain information service
Iber C (2007) The AASM manual for the scoring of sleep and associated events: Rules. Terminology and Technical Specification.
RB B. The AASM Manual for the Scoring of Sleep and Associated Events: rules, terminology and technical specifications, Version 2.0.2. In: R B, editor. www.aasmnet.org2013.
Chowdhuri S, Quan SF, Almeida F, Ayappa I, Batool-Anwar S, Budhiraja R et al (2016) An Official American Thoracic Society Research statement: impact of mild obstructive sleep apnea in adults. Am J Respir Crit Care Med 193(9):e37-54. https://doi.org/10.1164/rccm.201602-0361ST
Eckert DJ, White DP, Jordan AS, Malhotra A, Wellman A (2013) Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am J Respir Crit Care Med 188(8):996–1004. https://doi.org/10.1164/rccm.201303-0448OC
Vavougios GD, George DG, Pastaka C, Zarogiannis SG, Gourgoulianis KI (2016) Phenotypes of comorbidity in OSAS patients: combining categorical principal component analysis with cluster analysis. J Sleep Res 25(1):31–38. https://doi.org/10.1111/jsr.12344
McArdle N, Hillman D, Beilin L, Watts G (2007) Metabolic risk factors for vascular disease in obstructive sleep apnea: a matched controlled study. Am J Respir Crit Care Med 175(2):190–195. https://doi.org/10.1164/rccm.200602-270OC
Feng J, Zhang D, Chen B (2012) Endothelial mechanisms of endothelial dysfunction in patients with obstructive sleep apnea. Sleep Breath 16(2):283–294. https://doi.org/10.1007/s11325-011-0519-8
Zychowski KE, Sanchez B, Pedrosa RP, Lorenzi-Filho G, Drager LF, Polotsky VY et al (2016) Serum from obstructive sleep apnea patients induces inflammatory responses in coronary artery endothelial cells. Atherosclerosis 254:59–66. https://doi.org/10.1016/j.atherosclerosis.2016.09.017
Zinchuk AV, Gentry MJ, Concato J, Yaggi HK (2017) Phenotypes in obstructive sleep apnea: a definition, examples and evolution of approaches. Sleep Med Rev 35:113–123. https://doi.org/10.1016/j.smrv.2016.10.002
Joosten SA, Hamza K, Sands S, Turton A, Berger P, Hamilton G (2012) Phenotypes of patients with mild to moderate obstructive sleep apnoea as confirmed by cluster analysis. Respirology 17(1):99–107. https://doi.org/10.1111/j.1440-1843.2011.02037.x
Lacedonia D, Carpagnano GE, Sabato R, Storto MM, Palmiotti GA, Capozzi V et al (2016) Characterization of obstructive sleep apnea-hypopnea syndrome (OSA) population by means of cluster analysis. J Sleep Res 25(6):724–730. https://doi.org/10.1111/jsr.12429
Zinchuk AV, Jeon S, Koo BB, Yan X, Bravata DM, Qin L et al (2018) Polysomnographic phenotypes and their cardiovascular implications in obstructive sleep apnoea. Thorax 73(5):472–480. https://doi.org/10.1136/thoraxjnl-2017-210431
Mander BA, Winer JR, Walker MP (2017) Sleep and human aging. Neuron 94(1):19–36. https://doi.org/10.1016/j.neuron.2017.02.004
Crowley K (2011) Sleep and sleep disorders in older adults. Neuropsychol Rev 21(1):41–53. https://doi.org/10.1007/s11065-010-9154-6
Lack L, Sweetman A (2016) Diagnosis and treatment of insomnia comorbid with obstructive sleep apnea. Sleep Med Clin 11(3):379–388. https://doi.org/10.1016/j.jsmc.2016.05.006
Morrell MJ, Finn L, McMillan A, Peppard PE (2012) The impact of ageing and sex on the association between sleepiness and sleep disordered breathing. Eur Respir J 40(2):386–393. https://doi.org/10.1183/09031936.00177411
McMillan A, Morrell MJ (2016) Sleep disordered breathing at the extremes of age: the elderly. Breathe (Sheff) 12(1):50–60. https://doi.org/10.1183/20734735.003216
Funding
This work was supported by grants from the Associação Fundo de Incentivo à Pesquisa (AFIP), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP, 2018/00955–4 to PFT). MLA, LB and ST are recipients of CNPq fellowship.
Author information
Authors and Affiliations
Contributions
PFT, LB, and ST designed the study. PFT, LOS, and LB wrote the analyses protocol. PFT, LOS, TMG, TAV, VD, MLA, LB, and ST have helped with manuscript preparation, reviewing the text format, references, terminology, and overall structure.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Ethics Committee of Universidade Federal de São Paulo (CEP: 593/2006; 610514/2014).
Consent to participate
Written informed consent forms were completed and signed by all participants.
Consent for publication
Written informed consent forms were completed and signed by all participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Comments
This study presents essential scientific contributions to the evident need for grounding the diagnosis of obstructive sleep apnea (OSA), and particularly its therapy choice, on parameters and classifications other than the apnea and hypopnea index (AHI).
Also, despite the well-known difficulties in developing follow-up studies, the investigation stands out in that the authors follow the methodology proposed unprecedentedly pointing out evidence that the clinical subtypes of OSA in the same population change over time.
Luciano Moraes Studart-Pereira
Brazil
Supplementary Information
Below is the link to the electronic supplementary material.
11325_2021_2470_MOESM1_ESM.docx
Supplementary file1 Supplemental Table 1. Bayesian Information Criterion (BIC) values for up to 10 clusters for baseline and follow-up EPISONO cohorts (DOCX 14 KB)
11325_2021_2470_MOESM2_ESM.docx
Supplementary file2 Supplemental Table 2. Clinical and polysomnographic characteristics of the 2 symptom clusters in the baseline EPISONO study (DOCX 19 KB)
Rights and permissions
About this article
Cite this article
Tempaku, P.F., Oliveira e Silva, L., Guimarães, T.M. et al. The reproducibility of clinical OSA subtypes: a population-based longitudinal study. Sleep Breath 26, 1253–1263 (2022). https://doi.org/10.1007/s11325-021-02470-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02470-5