Abstract
Purpose
Severe cardiac dysfunction can manifest with diurnal breathing irregularity. However, it remains to be clarified whether or not diurnal breathing irregularity is observed in patients with heart diseases, including relatively mild chronic heart failure (CHF), compared to those without heart diseases.
Methods
In this cross-sectional study, consecutive inpatients who were admitted for evaluation of sleep-disordered breathing were enrolled. We extracted 3.5 min of stable respiratory signals before sleep onset using polysomnography, analyzed the airflow data using fast Fourier transform, and quantified breathing irregularities using Shannon entropy S.
Results
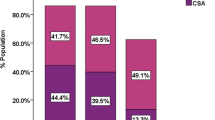
A total of 162 subjects were evaluated. Among these, 39 subjects had heart diseases, including ischemic heart disease (IHD), atrial fibrillation (Af), CHF, and a history of aortic dissection. The values of Shannon entropy S of airflow signals in subjects with heart diseases were significantly higher than in those without heart diseases (p < 0.001). After excluding CHF, the Shannon entropy S was also significantly higher in subjects with heart diseases than in those without heart diseases (p < 0.001). The values of Shannon entropy S were significantly correlated with plasma brain natriuretic peptide levels (r = 0.443, p < 0.001). Although the values were also significantly correlated with body mass index, the presence of heart diseases was independently associated with breathing irregularity in the multiple logistic analysis. Matching analysis revealed consistent differences between subjects with heart diseases and without heart diseases.
Conclusion
Breathing irregularity was observed before sleep onset in subjects with heart diseases who underwent polysomnography to diagnose sleep-disordered breathing.





Similar content being viewed by others
References
Mortara A, Sleight P, Pinna GD, Maestri R, Capomolla S, Febo O, La Rovere MT, Cobelli F (1999) Association between hemodynamic impairment and Cheyne-Stokes respiration and periodic breathing in chronic stable congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol 84:900–904. https://doi.org/10.1016/s0002-9149(99)00462-2
Oldenburg O (2012) Cheyne-stokes respiration in chronic heart failure. Treatment with adaptive servoventilation therapy. Circ J 76:2305–2317. https://doi.org/10.1253/circj.cj-12-0689
Brack T, Thüer I, Clarenbach CF, Senn O, Noll G, Russi EW, Bloch KE (2007) Daytime Cheyne-Stokes respiration in ambulatory patients with severe congestive heart failure is associated with increased mortality. Chest 132:1463–1471. https://doi.org/10.1378/chest.07-0121
Kumagai N, Dohi K, Fujimoto N, Tanimura M, Sato Y, Miyahara S, Nakamori S, Fujii E, Yamada N, Ito M (2018) A novel method for the quantitative evaluation of diurnal respiratory instability in patients with heart failure: a pilot study. J Cardiol 71:159–167. https://doi.org/10.1016/j.jjcc.2017.08.002
Asanoi H, Harada D, Oda Y, Ueno H, Takagawa J, Ishise H, Goso Y, Joho S, Inoue H (2017) Independent prognostic importance of respiratory instability and sympathetic nerve activity in patients with chronic heart failure. J Cardiol 70:476–483. https://doi.org/10.1016/j.jjcc.2017.02.011
Edwards BA, Eckert DJ, Jordan AS (2017) Obstructive sleep apnoea pathogenesis from mild to severe: is it all the same? Respirology 22:33–42. https://doi.org/10.1111/resp.12913
Sands SA, Edwards BA, Terrill PI, Taranto-Montemurro L, Azarbarzin A, Marques M, Hess LB, White DP, Wellman A (2018) Phenotyping pharyngeal pathophysiology using polysomnography in patients with obstructive sleep apnea. Am J Respir Crit Care Med 197:1187–1197. https://doi.org/10.1164/rccm.201707-1435OC
Yamauchi M, Tamaki S, Yoshikawa M, Ohnishi Y, Nakano H, Jacono FJ, Loparo KA, Strohl KP, Kimura H (2011) Differences in breathing patterning during wakefulness in patients with mixed apnea-dominant vs obstructive-dominant sleep apnea. Chest 140:54–61. https://doi.org/10.1378/chest.10-1082
Yamauchi M, Jacono FJ, Fujita Y, Yoshikawa M, Ohnishi Y, Nakano H, Campanaro CK, Loparo KA, Strohl KP, Kimura H (2013) Breathing irregularity during wakefulness associates with CPAP acceptance in sleep apnea. Sleep Breath 17:845–852. https://doi.org/10.1007/s11325-012-0775-2
Hibi S, Yamaguchi Y, Umeda-Kameyama Y, Iijima K, Takahashi M, Momose T, Akishita M, Ouchi Y (2013) Respiratory dysrhythmia in dementia with Lewy bodies: a cross-sectional study. BMJ Open 3:e002870. https://doi.org/10.1136/bmjopen-2013-002870
Nakayama H, Hokari S, Ohshima Y, Matsuto T, Shimohata T (2018) Breathing irregularity is independently associated with the severity of obstructive sleep apnea in patients with multiple system atrophy. J Clin Sleep Med 14:1661–1667. https://doi.org/10.5664/jcsm.7368
Iber C, Ancoli-Israel S, Chesson A, Quan SF, for the American Academy of Sleep Medicine (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, 1st edn. American Academy of Sleep Medicine, Westchester
Sands SA, Owens RL (2015) Congestive heart failure and central sleep apnea. Crit Care Clin 31:473–495. https://doi.org/10.1016/j.ccc.2015.03.005
Shimokawa H, Miura M, Nochioka K, Sakata Y (2015) Heart failure as a general pandemic in Asia. Eur J Heart Fail 17:884–892. https://doi.org/10.1002/ejhf.319
Mosterd A, Hoes AW, de Bruyne MC, Deckers JW, Linker DT, Hofman A, Grobbee DE (1999) Prevalence of heart failure and left ventricular dysfunction in the general population; the Rotterdam study. Eur Heart J 20:447–455
Gottdiener JS, McClelland RL, Marshall R, Shemanski L, Furberg CD, Kitzman DW, Cushman M, Polak J, Gardin JM, Gersh BJ, Aurigemma GP, Manolio TA (2002) Outcome of congestive heart failure in elderly persons: influence of left ventricular systolic function. The Cardiovascular Health Study. Ann Intern Med 137:631–639. https://doi.org/10.7326/0003-4819-137-8-200210150-00006
Kasai T (2012) Sleep apnea and heart failure. J Cardiol 60:78–85. https://doi.org/10.1016/j.jjcc.2012.05.013
Ng AC, Freedman SB (2009) Sleep disordered breathing in chronic heart failure. Heart Fail Rev 14:89–99. https://doi.org/10.1007/s10741-008-9096-8
Aihara K, Oga T, Harada Y, Chihara Y, Handa T, Tanizawa K, Watanabe K, Hitomi T, Tsuboi T, Mishima M, Chin K (2012) Analysis of anatomical and functional determinants of obstructive sleep apnea. Sleep Breath 16:473–481. https://doi.org/10.1007/s11325-011-0528-7
Baratta F, Pastori D, Bucci T, Fabiani M, Fabiani V, Brunori M, Loffredo L, Lillo R, Pannitteri G, Angelico F, Del Ben M (2018) Long-term prediction of adherence to continuous positive air pressure therapy for the treatment of moderate/severe obstructive sleep apnea syndrome. Sleep Med 43:66–70. https://doi.org/10.1016/j.sleep.2017.09.032
Yang MC, Huang YC, Lan CC, Wu YK, Huang KF (2015) Beneficial effects of long-term CPAP treatment on sleep quality and blood pressure in adherent subjects with obstructive sleep apnea. Respir Care 60:1810–1818. https://doi.org/10.4187/respcare.04199
Drager LF, McEvoy RD, Barbe F, Lorenzi-Filho G, Redline S, INCOSACT Initiative (International Collaboration of Sleep Apnea Cardiovascular Trialists) (2017) Sleep apnea and cardiovascular disease: lessons from recent trials and need for team science. Circulation 136:1840–1850. https://doi.org/10.1161/CIRCULATIONAHA.117.029400
Khan SU, Duran CA, Rahman H, Lekkala M, Saleem MA, Kaluski E (2018) A meta-analysis of continuous positive airway pressure therapy in prevention of cardiovascular events in patients with obstructive sleep apnoea. Eur Heart J 39:2291–2297. https://doi.org/10.1093/eurheartj/ehx597
Testelmans D, Buyse B (2017) CPAP adherence: a matter of perfect airflow curves? Respir Care 62:515–516. https://doi.org/10.4187/respcare.05498
Douglas NJ, White DP, Weil JV, Pickett CK, Zwillich CW (1982) Hypercapnic ventilatory response in sleeping adults. Am Rev Respir Dis 126:758–762
Douglas NJ, White DP, Weil JV, Pickett CK, Martin RJ, Hudgel DW, Zwillich CW (1982) Hypoxic ventilatory response decreases during sleep in normal men. Am Rev Respir Dis 125:286–289
Flinta I, Ponikowski P (2016) Relationship between central sleep apnea and Cheyne-Stokes respiration. Int J Cardiol 206:S8-12. https://doi.org/10.1016/j.ijcard.2016.02.124
Acknowledgements
We would like to thank Editage (www.editage.jp) for English language editing.
Funding
This work was supported by Grants-in-aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (grant code 18K07440).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Given the retrospective nature of the study and the use of anonymized patient data, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Disclaimer
The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Okamoto, S., Ishii, M., Hibi, S. et al. Breathing irregularities before sleep onset on polysomnography in patients with heart diseases. Sleep Breath 26, 605–612 (2022). https://doi.org/10.1007/s11325-021-02403-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02403-2