Abstract
Purpose
To synthesize findings of economic evaluations investigating cost-effectiveness of continuous positive airway pressure (CPAP) for obstructive sleep apnea (OSA) and of strategies of organization of care related to CPAP therapy.
Methods
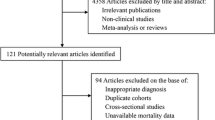
Scoping review with searches conducted in MEDLINE, CRD, LILACS, and Embase in August 2020. Eligible studies were economic evaluations comparing CPAP to other alternative or assessing strategies of care for CPAP therapy. Results were presented narratively, and incremental cost-effectiveness ratios (ICER) were presented in evidence maps.
Results
Of 34 studies, 3 concluded that CPAP is less costly and more effective when compared to usual care. Most studies indicated that CPAP is associated with better health outcomes, but at higher prices. ICER ranged from USD 316 to 98,793 per quality-adjusted life years (QALY) gained (median 16,499; IQR 8267 to 33,119). One study concluded that CPAP is more costly and less effective, when treatment is applied to all patients, regardless of disease severity. Variability of ICER was mainly due to definition of population and applied time horizons. When CPAP was compared to mandibular advancement device, ICER ranged from USD 21,153 to 361,028 (median 89,671; IQR 26,829 to 295,983), which represents the investment in CPAP therapy required to obtain one extra QALY. Three studies assessed the effects of organizing CPAP therapy in primary care, which was cost-effective or cost-saving.
Conclusions
Compared to usual care, CPAP is cost-effective after the second year of treatment, when indicated for moderate-to-severe OSA. CPAP therapy may be even more cost-effective by using different strategies of organization of care. These findings may inform decision making related to CPAP reimbursement in health systems.
Clinical Trial Registration number
Not applicable



Similar content being viewed by others
Data availability
Relevant data is presented in Supplemental material.
References
American Academy of Sleep Medicine (ed) (2014) International classification of sleep disorders. Third edit, American Academy of Sleep Medicine, Darien, IL
Garvey JF, Pengo MF, Drakatos P, Kent BD (2015) Epidemiological aspects of obstructive sleep apnea. J Thorac Dis 7:920–929. https://doi.org/10.3978/j.issn.2072-1439.2015.04.52
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL, Peppard PE, Sinha S, Tufik S, Valentine K, Malhotra A (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7:687–698. https://doi.org/10.1016/S2213-2600(19)30198-5
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J (2000) Longitudinal study of moderate weight change and sleep-disordered breathing. J Am Med Assoc 284:3015–3021. https://doi.org/10.1001/jama.284.23.3015
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177:1006–1014. https://doi.org/10.1093/aje/kws342
Lorenzi-Filho G, Drager LF (2015) Type I diabetes: a new risk factor for obstructive sleep apnea. Rev Port Pneumol 21:53–54. https://doi.org/10.1016/j.rppnen.2015.02.002
Cakirer B, Hans MG, Graham G et al (2001) The relationship between craniofacial morphology and obstructive sleep apnea in whites and in African-Americans. Am J Respir Crit Care Med 163:947–950. https://doi.org/10.1164/ajrccm.163.4.2005136
Hou H, Zhao Y, Yu W, Dong H, Xue X, Ding J, Xing W, Wang W (2018) Association of obstructive sleep apnea with hypertension: a systematic review and meta-analysis. J Glob Health 8:1–10. https://doi.org/10.7189/jogh.08.010405
Doonan RJ, Scheffler P, Lalli M, Kimoff RJ, Petridou ET, Daskalopoulos ME, Daskalopoulou SS (2011) Increased arterial stiffness in obstructive sleep apnea: a systematic review. Hypertens Res 34:23–32. https://doi.org/10.1038/hr.2010.200
Loke YK, Brown JWL, Kwok CS, Niruban A, Myint PK (2012) Association of obstructive sleep apnea with risk of serious cardiovascular events: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 5:720–728. https://doi.org/10.1161/CIRCOUTCOMES.111.964783
Youssef I, Kamran H, Yacoub M et al (2018) Obstructive sleep apnea as a risk factor for atrial fibrillation: a meta-analysis. J Sleep Disord Ther 7:282–148. https://doi.org/10.1016/j.physbeh.2017.03.040
Xie W, Zheng F, Song X (2014) Obstructive sleep apnea and serious adverse outcomes in patients with cardiovascular or cerebrovascular disease: a PRISMA-compliant systematic review and meta-analysis. Med (United States) 93:e336. https://doi.org/10.1097/MD.0000000000000336
Qie R, Zhang D, Liu L, Ren Y, Zhao Y, Liu D, Liu F, Chen X, Cheng C, Guo C, Li Q, Zhou Q, Tian G, Han M, Huang S, Wu X, Qin P, Li J, Cao J, Zhang M, Huang J, Lu J, Li H, Wang J, Cheng R, Hu D (2020) Obstructive sleep apnea and risk of type 2 diabetes mellitus: a systematic review and dose-response meta-analysis of cohort studies. J Diabetes 12:455–464. https://doi.org/10.1111/1753-0407.13017
Kario K (2009) Obstructive sleep apnea syndrome and hypertension: mechanism of the linkage and 24-h blood pressure control. Hypertens Res 32:537–541. https://doi.org/10.1038/hr.2009.73
Tregear S, Reston J, Schoelles K, Phillips B (2009) Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med 5:573–581
Garbarino S, Guglielmi O, Sanna A, Mancardi GL, Magnavita N (2016) Risk of occupational accidents in workers with obstructive sleep apnea: systematic review and meta-Analysis. Sleep 39:1211–1218
Engleman HM, Kingshott RN, Martin SE, Douglas NJ (2000) Cognitive function in the sleep apnea/hypopnea syndrome (SAHS). Sleep 23(Suppl 4):S102–S108
Bjornsdottir E, Keenan BT, Eysteinsdottir B, Arnardottir ES, Janson C, Gislason T, Sigurdsson JF, Kuna ST, Pack AI, Benediktsdottir B (2015) Quality of life among untreated sleep apnea patients compared with the general population and changes after treatment with positive airway pressure. J Sleep Res 24:328–338
Albarrak M, Banno K, Sabbagh A Al, et al (2005) Utilization of healthcare resources in obstructive sleep apnea syndrome: a 5-year follow-up study in men using CPAP. Sleep 28:1306–1311. doi:https://doi.org/10.1093/sleep/28.10.1306
Santos-Silva R, Castro LS, Taddei JA, Tufik S, Bittencourt LRA (2012) Sleep disorders and demand for medical services: evidence from a population-based longitudinal study. PLoS One 7:5–8. https://doi.org/10.1371/journal.pone.0030085
Banno K, Ramsey C, Walld R, Kryger MH (2009) Expenditure on health care in obese women with and without sleep apnea. Sleep 32:247–252. https://doi.org/10.1093/sleep/32.2.247
Knauert M, Naik S, Gillespie MB, Kryger M Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World J Otorhinolaryngol Head Neck Surg 1:17–27
Sassani A, Findley LJ, Kryger M, Goldlust E, George C, Davidson TM (2004) Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep 27:453–458
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American academy of sleep medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med 15:301–334. https://doi.org/10.5664/jcsm.7638
Sharples LD, Clutterbuck-James AL, Glover MJ, Bennett MS, Chadwick R, Pittman MA, Quinnell TG (2014) Meta-analysis of randomised controlled trials of oral mandibular advancement devices and continuous positive airway pressure for obstructive sleep apnoea-hypopnoea. Sleep Med Rev 27:108–124. https://doi.org/10.1016/j.smrv.2015.05.003
Iftikhar IH, Bittencourt L, Youngstedt SD, Ayas N, Cistulli P, Schwab R, Durkin MW, Magalang UJ (2017) Comparative efficacy of CPAP, MADs, exercise-training, and dietary weight loss for sleep apnea: a network meta-analysis. Sleep Med 30:7–14. https://doi.org/10.1016/j.sleep.2016.06.001
Antic NA, Catcheside P, Buchan C, Hensley M, Naughton MT, Rowland S, Williamson B, Windler S, McEvoy RD (2011) The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep 34:111–119. https://doi.org/10.1093/sleep/34.1.111
Rotenberg BW, Murariu D, Pang KP (2016) Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg 45:1–9. https://doi.org/10.1186/s40463-016-0156-0
Nogueira JF, Poyares D, Simonelli G, Leiva S, Carrillo-Alduenda JL, Bazurto MA, Terán G, Valencia-Flores M, Serra L, de Castro JR, Santiago-Ayala V, Pérez-Chada D, Franchi ME, Lucchesi L, Tufik S, Bittencourt L (2020) Accessibility and adherence to positive airway pressure treatment in patients with obstructive sleep apnea: a multicenter study in Latin America. Sleep Breath 24:455–464. https://doi.org/10.1007/s11325-019-01881-9
Flemons WW, Douglas NJ, Kuna ST, Rodenstein DO, Wheatley J (2004) Access to diagnosis and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med 169:668–672. https://doi.org/10.1164/rccm.200308-1124
Sucharew H, Macaluso M (2019) Methods for research evidence synthesis: the scoping review approach. J Hosp Med 14:416–418. https://doi.org/10.12788/jhm.3248
Arksey H, Malley LO (2005) Scoping studies: towards a methodological framework. Int J Soc Res Methodol 8:19–32. https://doi.org/10.1080/1364557032000119616
Levac D, Colquhoun H, O’Brien KK (2010) Scoping studies: advancing the methodology. Implement Sci 5:69. https://doi.org/10.1186/1748-5908-5-69
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169:467–473. https://doi.org/10.7326/M18-0850
Pachito D V, Rocha A (2020) Economic models for estimating cost-effectiveness of CPAP treatment in OSAS patients: a scoping review. osf.io/sh32w. Accessed 16 Aug 2020
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev 5:210. https://doi.org/10.1186/s13643-016-0384-4
Gafni A, Birch S (2006) Incremental cost-effectiveness ratios (ICERs): the silence of the lambda. Soc Sci Med 62:2091–2100. https://doi.org/10.1016/j.socscimed.2005.10.023
Miake-Lye IM, Hempel S, Shanman R, Shekelle PG (2016) What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst Rev 5. https://doi.org/10.1186/s13643-016-0204-x
Wickham H (2016) ggplot2: elegant graphics for data analysis. Springer-Verlag, New York
Higgins J, Thomas J, Chandler J, et al (2019) Cochrane Handbook for systematic reviews of interventions version 6.0. www.training.cochrane.org/handbook. Accessed 19 Mar 2020
Ayas NT, FitzGerald JM, Fleetham JA et al (2006) Cost-effectiveness of continuous positive airway pressure therapy for moderate to severe obstructive sleep apnea/hypopnea. Arch Intern Med 166:977–984. https://doi.org/10.1001/archinte.166.9.977
Català R, Villoro R, Merino M, Sangenís S, Colomés L, Hernández Flix S, Pérez de Llano LA (2016) Análisis coste-efectividad del tratamiento con presión positiva continua de la vía aérea en el síndrome de apnea-hipopnea durante el sueño (SAHS) moderado-grave. Arch Bronconeumol 52:461–469. https://doi.org/10.1016/j.arbr.2016.07.006
Trakada G, Economou NT, Nena E, Trakada A, Zarogoulidis P, Steiropoulos P (2015) A health-economic analysis of diagnosis and treatment of obstructive sleep apnea with continuous positive airway pressure in relation to cardiovascular disease. The Greek experience. Sleep Breath 19:467–472. https://doi.org/10.1007/s11325-014-1050-5
McDaid C, Griffin S, Weatherly H et al (2009) Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea-hypopnoea syndrome: a systematic review and economic analysis. Health Technol Assess (Rockv) 13:142. https://doi.org/10.3310/hta13040
Gay J, Valls M, Jose Luis C (2018) Cost-effectiveness of oxigen therapy with C-PAP for the treatment of obstructive sleep apnoea syndrome (OSA) versus the standard of care in the Mexican public health care system. Value Health 21:S258
Lucchetta R, Rosim M, Okumura L et al (2019) Continuous positive airway pressure device compared to usual care for severe obstructive sleep apnea: a cost-effectiveness analysis. Value Health 22:S217
Giannopoulou A, Burgers L, Van Bruggen M et al (2013) Economic evaluation of mandibular advancement device to treat obstructive sleep apnea. Value Health 16:A373
Pietzsch JB, Garner A, Cipriano LE, Linehan JH (2011) An integrated health-economic analysis of diagnostic and therapeutic strategies in the treatment of moderate-to-severe obstructive sleep Apnea. Sleep 34:695–709. https://doi.org/10.5665/SLEEP.1030
Tousignant P, Cosio MG, Levy RD, Groome PA (1994) Quality adjusted life years added by treatment of obstructive sleep apnea. Sleep 17:52–60. https://doi.org/10.1093/sleep/17.1.52
Sadatsafavi M, Marra CA, Ayas NT, Stradling J, Fleetham J (2009) Cost-effectiveness of oral appliances in the treatment of obstructive sleep apnoea - hypopnoea. Sleep Breath 13:241–252. https://doi.org/10.1007/s11325-009-0248-4
Poullié A-I, Cognet M, Gauthier A, Clementz M, Druais S, Späth HM, Perrier L, Scemama O, Pichon CR, Harousseau JL (2016) Cost-effectiveness of treatments for mild-to-moderate obstructive sleep apnea in France. Int J Technol Assess Health Care 32:37–45
Guest JF, Helter MT, Morga A, Stradling JR (2008) Cost-effectiveness of using continuous positive airway pressure in the treatment of severe obstructive sleep apnoea/hypopnoea syndrome in the UK. Thorax 63:860–865
Guest JF, Panca M, Sladkevicius E, Taheri S, Stradling J (2014) Clinical outcomes and cost-effectiveness of continuous positive airway pressure to manage obstructive sleep apnea in patients with type 2 diabetes in the U.K. Diabetes Care 37:1263–1271. https://doi.org/10.2337/dc13-2539
Lojander J, Räsänen P, Sintonen H, Roine RP, HUS QoL Study Group* (2008) Effect of nasal continuous positive airway pressure therapy on health-related quality of life in sleep apnoea patients treated in the routine clinical setting of a university hospital. J Int Med Res 36:760–770. https://doi.org/10.1177/147323000803600418
Mar J, Rueda JR, Durán-Cantolla J, Schechter C, Chilcott J (2003) The cost-effectiveness of nCPAP treatment in patients with moderate-to-severe obstructive sleep apnoea. Eur Respir J 21:515–522. https://doi.org/10.1183/09031936.03.00040903
McMillan A, Bratton DJ, Faria R, Laskawiec-Szkonter M, Griffin S, Davies RJ, Nunn AJ, Stradling JR, Riha RL, Morrell MJ (2015) A multicentre randomised controlled trial and economic evaluation of continuous positive airway pressure for the treatment of obstructive sleep apnoea syndrome in older people: PREDICT. Health Technol Assess 19:1–188
Sharples L, Glover M, Clutterbuck-James A, Bennett M, Jordan J, Chadwick R, Pittman M, East C, Cameron M, Davies M, Oscroft N, Smith I, Morrell M, Fox-Rushby J, Quinnell T (2014) Clinical effectiveness and cost-effectiveness results from the randomised controlled Trial of Oral Mandibular Advancement Devices for Obstructive sleep apnoea-hypopnoea (TOMADO) and long-term economic analysis of oral devices and continuous positive airwa. Health Technol Assess (Rockv) 18:1–296
Streatfeild J, Hillman D, Adams R, et al (2019) Cost-effectiveness of continuous positive airway pressure therapy for obstructive sleep apnea: healthcare system and societal perspectives. Sleep 42:zsz181
Tan MCY, Ayas NT, Mulgrew A, Cortes L, FitzGerald J, Fleetham JA, Schulzer M, Ryan CF, Ghaeli R, Cooperx P, Marra CA (2008) Cost-effectiveness of continuous positive airway pressure therapy in patients with obstructive sleep apnea-hypopnea in British Columbia. Can Respir J 15:159–165
Ángeles Sánchez-Quiroga M, Corral J, Gómez-de-Terreros FJ et al (2018) Primary care physicians can comprehensively manage patients with sleep apnea a noninferiority randomized controlled trial. Am J Respir Crit Care Med 198:648–656. https://doi.org/10.1164/rccm.201710-2061OC
Billings ME, Kapur VK (2013) Medicare long-term CPAP coverage policy: a cost-utility analysis. J Clin Sleep Med 9:1023–1029. https://doi.org/10.5664/jcsm.3074
Kim R, Kapur V, Redline Bruch J, Rueschman M et al (2012) Cost minimization analysis of a multi-site randomized clinical trial of home-based versus laboratory-based testing for the diagnosis and treatment of obstructive sleep apnea (Homepap Study). Value Health 15:A68–A69
Ekroos H, Karvonen T, Hahl J (2017) Telemonitoring versus usual care in continuous positive airway pressure users: Cost analysis. Eur Respir J 50:PA2281
Becker K, Chang N, Chang J et al (2012) Effectiveness of a respiratory therapist based CPAP follow-up program. Sleep 35:A172
Ramos F, Chatila W, Shariff T et al (2015) Cost effectiveness of incorporating positional therapy into a treatment algorithm for obstructive sleep apnea. Sleep 38:A442
Vega ME, Diaz-Abad M, Jaffe F et al (2019) Use of positional therapy when incorporated into a diagnosis-treatment algorithm for obstructive sleep apnea. Sleep Sci 12:15–20. https://doi.org/10.5935/1984-0063.20190052
Fischer J (2003) Kosten-Nutzen-Analyse bei Patienten mit schlafbezogenen Atmungsst. Biomed Tech Eng 48:245–251. https://doi.org/10.1515/bmte.2003.48.9.245
Isetta V, Negrín MA, Monasterio C, Masa JF, Feu N, Álvarez A, Campos-Rodriguez F, Ruiz C, Abad J, Vázquez-Polo FJ, Farré R, Galdeano M, Lloberes P, Embid C, de la Peña M, Puertas J, Dalmases M, Salord N, Corral J, Jurado B, León C, Egea C, Muñoz A, Parra O, Cambrodi R, Martel-Escobar M, Arqué M, Montserrat JM, the SPANISH SLEEP NETWORK (2015) A Bayesian cost-effectiveness analysis of a telemedicine-based strategy for the management of sleep apnoea: a multicentre randomised controlled trial. Thorax 70:1054–1061. https://doi.org/10.1136/thoraxjnl-2015-207032
Lugo VM, Garmendia O, Suarez-Girón M, Torres M, Vázquez-Polo FJ, Negrín MA, Moraleda A, Roman M, Puig M, Ruiz C, Egea C, Masa JF, Farré R, Montserrat JM (2019) Comprehensive management of obstructive sleep apnea by telemedicine: clinical improvement and cost-effectiveness of a Virtual Sleep Unit. A randomized controlled trial. PLoS One 14:1–15. https://doi.org/10.1371/journal.pone.0224069
Pelletier-Fleury N, Meslier N, Gagnadoux F, Person C, Rakotonanahary D, Ouksel H, Fleury B, Racineux JL (2004) Economic arguments for the immediate management of moderate-to-severe obstructive sleep apnoea syndrome. Eur Respir J 23:53–60. https://doi.org/10.1183/09031936.03.00066903
Sánchez-De-La-Torre M, Nadal N, Cortijo A et al (2015) Role of primary care in the follow-up of patients with obstructive sleep apnoea undergoing CPAP treatment: a randomised controlled trial. Thorax 70:346–352. https://doi.org/10.1136/thoraxjnl-2014-206287
Tarraubella N, Sánchez-De-La-Torre M, Nadal N et al (2018) Management of obstructive sleep apnoea in a primary care vs sleep unit setting: a randomised controlled trial. Thorax 73:1152–1160. https://doi.org/10.1136/thoraxjnl-2017-211237
Trenaman L, Sadatsafavi M, Almeida F, Ayas N, Lynd L, Marra C, Stacey D, Bansback N (2015) Exploring the potential cost-effectiveness of patient decision aids for use in adults with obstructive sleep apnea: a case study. Med Decis Mak 35:671–682. https://doi.org/10.1177/0272989X14556676
Turino C, De Batlle J, Woehrle H et al (2017) Management of continuous positive airway pressure treatment compliance using telemonitoring in obstructive sleep apnoea. Eur Respir J 49:1601128. https://doi.org/10.1183/13993003.01128-2016
Moro M, Westover MB, Kelly J, Bianchi MT (2016) Decision modeling in sleep apnea: the critical roles of pretest probability, cost of untreated obstructive sleep apnea, and time horizon. J Clin Sleep Med 12:409–418
Wickwire EM, Albrecht JS, Towe MM, Abariga SA, Diaz-Abad M, Shipper AG, Cooper LM, Assefa SZ, Tom SE, Scharf SM (2019) The impact of treatments for OSA on monetized health economic outcomes: a systematic review. Chest 155:947–961. https://doi.org/10.1016/j.chest.2019.01.009
Toraldo DM, Passali D, Sanna A et al (2017) Cost-effectiveness strategies in OSAS management: a short review. Acta Otorhinolaryngol Ital 37:447–453. https://doi.org/10.14639/0392-100X-1520
Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB (1996) Recommendations of the panel on cost-effectiveness in health and medicine. JAMA 276:1253–1258
Brazier J, Ara R, Azzabi I, Busschbach J, Chevrou-Séverac H, Crawford B, Cruz L, Karnon J, Lloyd A, Paisley S, Pickard AS (2019) Identification, review, and use of health state utilities in cost-effectiveness models: an ISPOR good practices for outcomes research task force report. Value Health 22:267–275. https://doi.org/10.1016/j.jval.2019.01.004
Acknowledgements
Authors are grateful to Beny Finkelstein, who kindly translated the study conducted by Fischer et al., originally published in German.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
DVP developed the study protocol. DVP and AR performed searches, screened references, and extracted data. DVP, AMB, and AR performed narrative synthesis and developed and revised the manuscript. ALE and LFD contributed to study design and revised the manuscript critically.
Corresponding author
Ethics declarations
Conflict of interest
DVP, ALE, and LFD have been developing consulting activities for ResMed Brasil. AMB and AR declare no potential conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presentation at a conference: This study has not been previously presented.
Supplementary Information
ESM 1
(DOCX 70 kb)
Rights and permissions
About this article
Cite this article
Pachito, D.V., Bagattini, Â.M., Drager, L.F. et al. Economic evaluation of CPAP therapy for obstructive sleep apnea: a scoping review and evidence map. Sleep Breath 26, 17–30 (2022). https://doi.org/10.1007/s11325-021-02362-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02362-8