Abstract
Background
Infertility is a major health problem that affects both the family and the community. Women receiving infertility treatment may suffer from stress and even experience sleep disturbance. Sleep quality is an important factor of human health and well-being. Sleep disturbances tend to occur among infertile women during in vitro fertilization treatment. Many studies have focused on the stress and sleep quality associated with their treatment in infertile women. However, few studies have investigated factors linked to their sleep disturbances.
Objective
This study investigated the relationship between perceived stress and sleep quality before oocyte pick-up, in vitro fertilization-embryo transfer, and pregnancy test in women receiving in vitro fertilization treatment.
Material and methods
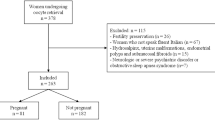
This prospective, longitudinal study was conducted between January and May 2020. One hundred fifty-seven women receiving infertility treatment were included in the study. A personal information form, the Perceived Stress Scale (PSS), and the Pittsburgh Sleep Quality Index (PSQI) were used to collect data.
Results
The relationship between the Perceived Stress Scale scores and the Pittsburgh Sleep Quality Index scores in all stages of infertility treatment was found to be positively significant at the p < .001 significance level.
Conclusion
Perceived stress level was high in women throughout the infertility treatment. Our study suggested that sleep quality was impaired as stress increased.
Trial registration
70904504/38
Similar content being viewed by others
Abbreviations
- ART:
-
assisted reproductive techniques
- ET:
-
embryo transfer
- IUI:
-
intrauterine insemination
- IVF:
-
in vitro fertilization
- OPU:
-
oocyte pick-up
- PCOS:
-
polycystic ovary syndrome
- PT:
-
pregnancy test
- PSS:
-
Perceived Stress Scale
- PSQI:
-
Pittsburgh Sleep Quality Index
- SPSS:
-
Statistical Package for the Social Sciences
- WHO:
-
World Health Organization
References
Zivaridelavar M, Kazemi A, Kheirabadi GR (2016) The effect of assisted reproduction treatment on mental health in fertile women. J Educ Health Promot 5:1–6. https://doi.org/10.4103/2277-9531.184552
Seymenler S, Siyez D (2018) Infertility counseling. Curr Approach Psychiatry 10:176–187. (in Turkish). https://doi.org/10.18863/pgy.358095
Domar AD, Rooney K, Hacker MR, Sakkas D, Dodge LE (2018) Burden of care is the primary reason why insured women terminate in vitro fertilisation treatment. Fertil Steril 109:1121–1126. https://doi.org/10.1016/j.fertnstert.2018.02.130
Freeman MP, Lee H, Savella GM, Sosinsky AZ, Marfurt SP, Murphy SK, Cohen LS (2018) Predictors of depressive relapse in women undergoing infertility treatment. J Women's Health 27:1408–1414. https://doi.org/10.1089/jwh.2017.6878
Haimovici F, Anderson JL, Bates GW, Racowsky C, Ginsburg ES, Simovici D, Fichorova RN (2018) Stress, anxiety, and depression of both partners in infertile couples are associated with cytokine levels and adverse IVF outcome. Am J Reprod Immunol 79:e12832. https://doi.org/10.1111/aji.12832
Hochschild FZ, Adamson GD, Dyer S, Racowsky C, Mouzon J, Sokol R et al (2017) The international glossary on infertility and fertility care, 2017. Hum Reprod 32:1786–1801. https://doi.org/10.1093/humrep/dex234
Hajiyan T, Afshari P, Abedi MR, Hashemi E (2017) Investigating infertility-related stress and adoption in İranian infertile females with assisted reproductive technology failure. Jundishapur J Chronic Dis Care 6:e39632. https://doi.org/10.17795/jjcdc-39632
Chen D, Zhang JP, Jiang L, Liu H, Shu L, Zhang Q, Jiang LP (2016) Factors that influence in vitro fertilisation treatment outcomes of Chinese men: a cross-sectional study. Appl Nurs Res 32:222–226. https://doi.org/10.1016/j.apnr.2016.07.003
World Health Organization (WHO). Human reproduction programme. Sexual and reproductive health. Available at http://www.who.int/reproductivehealth/topics/infertility/burden/en/. Accessed May 7, 2020
Wesselink AK, Hatch EE, Rothman KJ, Weuve JL, Aschengrau A, Song RJ, Wise LA (2018) Perceived stress and fecundability: a preconception cohort study of North American couples. Am J Epidemiol 187:2662–2671. https://doi.org/10.1093/aje/kwy186
Jamasian-Mobarake A, Dokanaeifard F (2017) The effectiveness of reality therapy on increasing resiliency, life expectancy and improve the quality of life of infertile women Infertility Center Sarim. Couns Cult Psychother 8:237–262. (in Persian). https://doi.org/10.22054/QCCPC.2017.19756.1462
Grunberg P, Miner S, Zelkowitz P (2020) Infertility and perceived stress: the role of identity concern in treatment-seeking men and women. Hum Fertil:1–11. https://doi.org/10.1080/14647273.2019.1709667
Chehreh R, Ozgoli G, Abolmaali K, Nasiri M, Mazaheri E (2019) Comparison of the infertility-related stress among couples and its relationship with infertility factors. Int J Women’s Health Reprod Sci 7:313–318. https://doi.org/10.15296/ijwhr.2019.52
Patel A, Sharma PS, Narayan P, Binu VS, Dinesh N, Pai PJ (2016) Prevalence and predictors of infertility-specific stress in women diagnosed with primary infertility: a clinic-based study. J Hum Reprod Sci 9:28–34. https://doi.org/10.4103/0974-1208.178630
Kloss JD, Perlis ML, Zamzow JA, Culnan EJ, Gracia CR (2015) Sleep, sleep disturbance, and fertility in women. Sleep Med Rev 22:78–87. https://doi.org/10.1016/j.smrv.2014.10.005
Azizi Kutenaee M, Amirjani S, Asemi Z, Taghavi SA, Allan H, Kamalnadian SN, Khashavi Z, Bazarganipour F (2020) The impact of depression, self-esteem, and body image on sleep quality in patients with PCOS: a cross-sectional study. Sleep Breath 24:1027–1034. https://doi.org/10.1007/s11325-019-01946-9
Lin YH, Chueh KH, Lin JL (2016) Somatic symptoms, sleep disturbance and psychological distress among women undergoing oocyte pick-up and in vitro fertilisation-embryo transfer. J Clin Nurs 25:1748–1756. https://doi.org/10.1111/jocn.13194
Goldstein CA, Lanham MS, Smith YR, O’Brien LM (2017) Sleep in women undergoing in vitro fertilisation: a pilot study. Sleep Med 32:105–113. https://doi.org/10.1016/j.sleep.2016.12.007
Kirca N, Pasinlioglu T (2019) The effect of yoga on stress level in infertile women. Perspect Psychiatr Care 55:319–327. https://doi.org/10.1111/ppc.12352
Maroufizadeh S, Hosseini M, Foroushani AR, Omami Samani R, Amini P (2019) The relationship between perceived stress and marital satisfaction in couples with infertility: actor-partner interdependence model. Fertil Steril 13:66–71. https://doi.org/10.22074/ijfs.2019.5437
Cohen S, Kamarck T, Mermelstein S (1983) A global measure of perceived stress. J Health Soc Behav 24:385–396
Erci B (2006) Reliability and validity of the Turkish version of perceived stress scale. Atatürk Univ J Nurs Schl 9:58–63
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193e213–193e213. https://doi.org/10.1016/0165-1781(89)90047-4
Agargun MY, Kara H, Anlar O (1996) The Validity and Reliability of the Pittsburgh Sleep Quality Index. Turk J Psychiatry 7:107–115 (in Turkish)
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum Associates
Eugster A, Vingerhoets AJ (1999) Psychological aspects of in vitro fertilization: a review. Soc Sci Med 48(5):575–589. https://doi.org/10.1016/s0277-9536(98)00386-4
Jansson-Frojmark M, Lindblom K (2008) Bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res 64(4):443–449. https://doi.org/10.1016/j.jpsychores.2007.10.016
Repokari L, Punamaki RL, Poikkeus P, Vilska S, Unkila-Kallio L, Sinkkonen J et al (2005) The impact of successful assisted reproduction treatment on female and male mental health during transition to parenthood: a prospective controlled study. Hum Reprod 20(11):3238–3247. https://doi.org/10.1093/humrep/dei214
Lin JL, Lin YH, Chueh KH (2014) Somatic symptoms, psychological distress and sleep disturbance among infertile women with intrauterine insemination treatment. J Clin Nurs 23(11-12):1677–1684. https://doi.org/10.1111/jocn.12306
Sowers MF, Zheng H, Kravitz HM, Matthews K, Bromberger JT, Gold EB, Owens J, Consens F, Hall M (2008) Sex steroid hormone profiles are related to sleep measures from polysomnography and the Pittsburgh Sleep Quality Index. Sleep 31(10):1339–1349
Humaidan P, Quartarolo J, Papanikolaou EG (2010) Preventing ovarian hyperstimulation syndrome: guidance for the clinician. Fertil Steril 94(2):389–400. https://doi.org/10.1016/j.fertnstert.2010.03.028
Su TJ, Chen YC, Yang YS (2001) Somatic symptoms during in vitro fertilization treatment. Formosan J Med 5:145–153
Delvigne A, Rozenberg S (2003) Review of clinical course and treatment of ovarian hyperstimulation syndrome (OHSS). Hum Reprod Update 9(1):77–96. https://doi.org/10.1093/humupd/dmg005
Gamble KL, Resuehr D, Johnson CH (2013) Shift work and circadian dysregulation of reproduction. Front Endocrinol 4:92.e1–92.10. https://doi.org/10.3389/fendo.2013.00092
Gozuyesil E, Karacay Yikar S, Nazik E (2019) An analysis of the anxiety and hopelessness levels of women during IVF-ET treatment. Perspect Psychiatr Care 56:338–346. https://doi.org/10.1111/ppc.12436
Onat G, Aba YA (2015) The effects of a healthy lifestyle and of anxiety levels on IVF outcomes. Afr J Reprod Health 19:92–101
Lee SH, Kuo BJ, Huang LS, Wang YM, Lee MS (2000) Psychosocial responses among infertile women in different stages of an IVF treatment program. J Nurs Res 8:515–528
Tseng YH, Mu PF, Hsia PH, Chao HT (2000) Family stress experienced by infertile women during IVF-ET therapy: a phenomenological study. J Nurs Res 8:325–337
Macey PM, Woo MA, Kumar R, Cross RL, Harper RM (2010) Relationship between obstructive sleep apnea severity and sleep, depression and anxiety symptoms in newly-diagnosed patients. PLoS One 5:e10211
Huang LH, Kuo CP, Lu YC, Lee MS, Lee SH (2019) Association of emotional distress and quality of sleep among women receiving in-vitro fertilisation treatment. Taiwan J Obstet Gynecol 58:168–172. https://doi.org/10.1016/j.tjog.2018.11.031
Anderson K, Nisenblat V, Norman R (2010) Lifestyle factors in people seeking infertility treatment-a review. Aust N Z J Obstet Gynecol 50(1):8–20. https://doi.org/10.1111/J.1479-828x.2009.01119.x
Yong P, Martin C, Thong J (2000) A comparison of psychological function in women at different stages of in vitro fertilisation treatment using the mean affect adjective check list. J Assist Reprod Genet 17:553–556. https://doi.org/10.1023/a:1026429712794
Acknowledgements
We would like to thank all the participants who shared their information with us.
Author information
Authors and Affiliations
Contributions
Study design, NK; data collection, NK; data analysis, NK; study supervision, NK; literature review, NK and MO; manuscript writing, NK and MO; and critical revisions for important intellectual content, NK.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presentation at a conference
It was presented as a verbal statement at the 1st National Women’s Health Congress organized by the Department of Midwifery, Faculty of Health Sciences, Halic University on September 12–13, 2020.
Rights and permissions
About this article
Cite this article
Kirca, N., Ongen, M. Perceived stress and sleep quality before oocyte pick-up, embryo transfer, and pregnancy test in women receiving in vitro fertilization treatment. Sleep Breath 25, 1977–1985 (2021). https://doi.org/10.1007/s11325-021-02328-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02328-w