Abstract
Background
Implementation of mandibular advancement splint (MAS) therapy as first-line treatment for obstructive sleep apnoea (OSA) is hindered by inter-individual variability of treatment outcomes and lack of robust patient selection methods. Optimal continuous positive airway pressure (CPAP) requirement provides an estimate of airway collapsibility severity, and high CPAP requirements predict MAS therapy failure in retrospective studies. Thus, understanding the effects of mandibular advancement on optimal CPAP requirements may enhance optimisation of patient selection for MAS therapy.
Objective
This study aims to determine dose-dependent effects of mandibular advancement on optimal CPAP requirements in OSA.
Methods
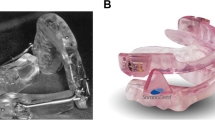
Prior to MAS therapy initiation, participants with OSA (apnoea-hypopnea index (AHI) > 10 events/h) underwent a research polysomnogram in which a remotely controlled mandibular positioner (RCMP) was used to determine dose–response effects of varying mandibular advancement positions (0% ‘habitual bite’ and 25, 50, 75 and 100% of maximum mandibular advancement, in random order) on optimal CPAP requirements. A separate polysomnography determined treatment outcome. Data are presented as mean ± SD or median (1st–3rd quartiles).
Results
Seventeen participants (age = 47 ± 9 years, body mass index = 26 kg/m2 (23–27), apnoea-hypopnea index = 18 events/h (14–44) and minimal oxygen saturation = 84 ± 7%) were studied. Optimal CPAP requirements were reduced with mandibular advancement in a dose-dependent manner (8.9 ± 2.4 vs. 7.9 ± 2.8, 6.4 ± 1.8, 5.7 ± 1.9 and 4.9 ± 1.8 cmH2O; respectively, p < 0.0001). Compared with non-responders, responders to MAS therapy had lower AHI, lower arousal index and greater MinSaO2 at baseline. Optimal CPAP requirements at 0% mandibular advancement (or other positions) were not different between groups.
Conclusions
Increasing mandibular advancement lowers optimal CPAP requirements in a dose-dependent manner. This supports prior work indicating a beneficial effect of MAS on upper airway collapsibility.



Similar content being viewed by others
References
Bixler E (2000) Association of hypertension and sleep-disordered breathing. Arch Intern Med 160(15):2289–2295
Nieto FJ, Young TB, Lind BK et al (2000) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study: Sleep Heart Health Study. JAMA. 283(14):1829–1836
Peker Y, Hedner J, Norum J, Kraiczi H, Carlson J (2002) Increased incidence of cardiovascular disease in middle-aged men with obstructive sleep apnea. Am J Respir Crit Care Med 166(2):159–165
Punjabi NM, Ahmed MM, Polotsky VY, Beamer BA, O’Donnell CP (2003) Sleep-disordered breathing, glucose intolerance, and insulin resistance. Respir Physiol Neurobiol 136(2–3):167–178
Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, Mooser V, Preisig M, Malhotra A, Waeber G, Vollenweider P, Tafti M, Haba-Rubio J (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3(4):310–318
Weaver TE, Grunstein RR (2008) Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 5(2):173–178
Catcheside PG (2010) Predictors of continuous positive airway pressure adherence. F1000 Med Rep 2:70
Rotenberg BW, Murariu D, Pang KP (2016) Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg 45(1):43
Ramar K, Dort LC, Katz SG et al (2015) Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update. J Clin Sleep Med 11(7):773–827
Aarab G, Lobbezoo F, Heymans MW, Hamburger HL, Naeije M (2011) Long-term follow-up of a randomized controlled trial of oral appliance therapy in obstructive sleep apnea. Respiration. 82(2):162–168
Phillips CL, Grunstein RR, Darendeliler MA, Mihailidou AS, Srinivasan VK, Yee BJ, Marks GB, Cistulli PA (2013) Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 187(8):879–887
Li W, Xiao L, Hu J (2013) The comparison of CPAP and oral appliances in treatment of patients with OSA: a systematic review and meta-analysis. Respir Care 58(7):1184–1195
Bloch KE, Iseli A, Zhang JN et al (2000) A randomized controlled crossover trial of two oral appliances for sleep apnea treatment. Am J Respir Crit Care Med 162(1):246–251
Pitsis AJ, Darendeliler MA, Gotsopoulos H, Petocz P, Cistulli PA (2002) Effect of vertical dimension on efficacy of oral appliance therapy in obstructive sleep apnea. Am J Respir Crit Care Med 166(6):860–864
Gotsopoulos H, Chen C, Qian J, Cistulli PA (2002) Oral appliance therapy improves symptoms in obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 166(5):743–748
Walker-Engstrom ML, Ringqvist I, Vestling O, Wilhelmsson B, Tegelberg A (2003) A prospective randomized study comparing two different degrees of mandibular advancement with a dental appliance in treatment of severe obstructive sleep apnea. Sleep Breath 7(3):119–130
Tegelberg A, Walker-Engstrom ML, Vestling O, Wilhelmsson B (2003) Two different degrees of mandibular advancement with a dental appliance in treatment of patients with mild to moderate obstructive sleep apnea. Acta Odontol Scand 61(6):356–362
Blanco J, Zamarron C, Abeleira Pazos MT, Lamela C, Suarez Quintanilla D (2005) Prospective evaluation of an oral appliance in the treatment of obstructive sleep apnea syndrome. Sleep Breath 9(1):20–25
Petri N, Svanholt P, Solow B, Wildschiodtz G, Winkel P (2008) Mandibular advancement appliance for obstructive sleep apnoea: results of a randomised placebo controlled trial using parallel group design. J Sleep Res 17(2):221–229
Tsuiki S, Ito E, Isono S, Ryan CF, Komada Y, Matsuura M, Inoue Y (2013) Oropharyngeal crowding and obesity as predictors of oral appliance treatment response to moderate obstructive sleep apnea. Chest. 144(2):558–563
Sutherland K, Takaya H, Qian J, Petocz P, Ng AT, Cistulli PA (2015) Oral appliance treatment response and polysomnographic phenotypes of obstructive sleep apnea. J Clin Sleep Med 11(8):861–868
Eckert DJ, White DP, Jordan AS, Malhotra A, Wellman A (2013) Defining phenotypic causes of obstructive sleep apnea: identification of novel therapeutic targets. Am J Respir Crit Care Med 188(8):996–1004
Eckert DJ (2018) Phenotypic approaches to obstructive sleep apnoea: new pathways for targeted therapy. Sleep Med Rev 37:45–59
Edwards BA, Andara C, Landry S, Sands SA, Joosten SA, Owens RL, White DP, Hamilton GS, Wellman A (2016) Upper airway collapsibility and loop gain predict the response to oral appliance therapy in patients with obstructive sleep apnea. Am J Respir Crit Care Med 194(11):1413–1422
Bamagoos AA, Cistulli PA, Sutherland K et al (2019) Dose-dependent effects of mandibular advancement on upper airway collapsibility and muscle function in obstructive sleep apnea. Sleep 42(6)
Ng AT, Qian J, Cistulli PA (2006) Oropharyngeal collapse predicts treatment response with oral appliance therapy in obstructive sleep apnea. Sleep. 29(5):666–671
Sutherland K, Phillips CL, Davies A, Srinivasan VK, Dalci O, Yee BJ, Darendeliler MA, Grunstein RR, Cistulli PA (2014) CPAP pressure for prediction of oral appliance treatment response in obstructive sleep apnea. J Clin Sleep Med 10(9):943–949
Chan AS, Sutherland K, Schwab RJ et al (2010) The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax. 65(8):726–732
Landry SA, Joosten SA, Eckert DJ et al (2017) Therapeutic CPAP level predicts upper airway collapsibility in patients with obstructive sleep apnea. Sleep 40(6)
Storesund A, Johansson A, Bjorvatn B, Lehmann S (2018) Oral appliance treatment outcome can be predicted by continuous positive airway pressure in moderate to severe obstructive sleep apnea. Sleep Breath 22(2):385–392
Tsuiki S, Kobayashi M, Namba K, Oka Y, Komada Y, Kagimura T, Inoue Y (2010) Optimal positive airway pressure predicts oral appliance response to sleep apnoea. Eur Respir J 35(5):1098–1105
Remmers J, Charkhandeh S, Grosse J, Topor Z, Brant R, Santosham P, Bruehlmann S (2013) Remotely controlled mandibular protrusion during sleep predicts therapeutic success with oral appliances in patients with obstructive sleep apnea. Sleep. 36(10):1517–1525
Berry RB, Budhiraja R, Gottlieb DJ et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 American Academy of Sleep Medicine manual for the scoring of sleep and associated events. J Clin Sleep Med 8(5):597–619
Petelle B, Vincent G, Gagnadoux F, Rakotonanahary D, Meyer B, Fleury B (2002) One-night mandibular advancement titration for obstructive sleep apnea syndrome: a pilot study. Am J Respir Crit Care Med 165(8):1150–1153
Tsai WH, Vazquez JC, Oshima T, Dort L, Roycroft B, Lowe AA, Hajduk E, Remmers JE (2004) Remotely controlled mandibular positioner predicts efficacy of oral appliances in sleep apnea. Am J Respir Crit Care Med 170(4):366–370
Dort LC, Hadjuk E, Remmers JE (2006) Mandibular advancement and obstructive sleep apnoea: a method for determining effective mandibular protrusion. Eur Respir J 27(5):1003–1009
Sutherland K, Ngiam J, Cistulli PA (2017) Performance of remotely controlled mandibular protrusion sleep studies for prediction of oral appliance treatment response. J Clin Sleep Med 13(3):411–417
Kushida CA, Chediak A, Berry RB et al (2008) Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med 4(2):157–171
Kato J, Isono S, Tanaka A, Watanabe T, Araki D, Tanzawa H, Nishino T (2000) Dose-dependent effects of mandibular advancement on pharyngeal mechanics and nocturnal oxygenation in patients with sleep-disordered breathing. Chest. 117(4):1065–1072
Ng AT, Gotsopoulos H, Qian J, Cistulli PA (2003) Effect of oral appliance therapy on upper airway collapsibility in obstructive sleep apnea. Am J Respir Crit Care Med 168(2):238–241
Marques M, Genta P, Sands SA et al (2017) Characterizing site and severity of upper airway collapse to guide patient selection for oral appliance therapy for obstructive sleep apnea [abstract]. Am J Respir Crit Care Med 195:A2584–A2584
Edwards BA, Eckert DJ, Jordan AS (2017) Obstructive sleep apnoea pathogenesis from mild to severe: is it all the same? Respirology. 22(1):33–42
Gray EL, McKenzie DK, Eckert DJ (2017) Obstructive sleep apnea without obesity is common and difficult to treat: evidence for a distinct pathophysiological phenotype. J Clin Sleep Med 13(1):81–88
Lai V, Tong BK, Tran C et al (2019) Combination therapy with mandibular dvancement and expiratory positive airway pressure valves reduces obstructive sleep apnea severity. Sleep
Zeng B, Ng AT, Qian J, Petocz P, Darendeliler MA, Cistulli PA (2008) Influence of nasal resistance on oral appliance treatment outcome in obstructive sleep apnea. Sleep. 31(4):543–547
Anitua E, Duran-Cantolla J, Almeida GZ, Alkhraisat MH (2017) Minimizing the mandibular advancement in an oral appliance for the treatment of obstructive sleep apnea. Sleep Med 34:226–231
Mayoral P, Lagravere MO, Miguez-Contreras M, Garcia M (2019) Antero-posterior mandibular position at different vertical levels for mandibular advancing device design. BMC Oral Health 19(1):85
Vroegop AV, Vanderveken OM, Van de Heyning PH, Braem MJ (2012) Effects of vertical opening on pharyngeal dimensions in patients with obstructive sleep apnoea. Sleep Med 13(3):314–316
Acknowledgements
The authors of this study are grateful for the support provided by members of the Sleep and Breathing Laboratory at NeuRA and the Centre for Sleep Health and Research at Royal North Shore Hospital including their roles in participants setup, data acquisition and data analysis. These individuals include: Carolin Tran, Andrea Ricciardiello, Alan Chiang, Benjamin Tong, Paras Acharya, Hanna Hensen, Mohammed Ahmadi and Aimee Lowth. The authors are also grateful to the study participants for taking the time to volunteer for the study.
Funding
This study was funded by the institutional research funds of PAC, DJE (NHMRC Senior Research Fellowship 1116942) and AAB (Scholarship for PhD studies from King Abdul-Aziz University). The study received equipment support from SomnoMed in the form of mandibular advancement splints.
Author information
Authors and Affiliations
Contributions
Study conception and design: PAC conceived the study and received design input from AAB, KS and DJE. Data collection: AAB, DJE and JN. Data analysis: AAB. Dental consultation and technical oversight: JN and AAB. Data interpretation, discussion, editing and critical revision of the manuscript: all authors.
Corresponding author
Ethics declarations
Conflict of interest
DJE held a Project Grant from the Commonwealth Government of Australia Cooperative Research Centres (industry partner: Oventus Medical) during the conduct of the study and received research grants from Bayer and Apnimed outside the submitted work. PAC has an appointment to an endowed academic Chair at the University of Sydney that was established from ResMed funding. He has received research support from ResMed, SomnoMed, Zephyr Sleep Technologies, and Bayer. He is a consultant to Zephyr Sleep Technologies and ResMed Narval. He has a pecuniary interest in SomnoMed related to a previous role in R&D (2004). AAB, KS and JN has no conflict of interest to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bamagoos, A.A., Eckert, D.J., Sutherland, K. et al. Dose-dependent effects of mandibular advancement on optimal positive airway pressure requirements in obstructive sleep apnoea. Sleep Breath 24, 961–969 (2020). https://doi.org/10.1007/s11325-019-01930-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01930-3